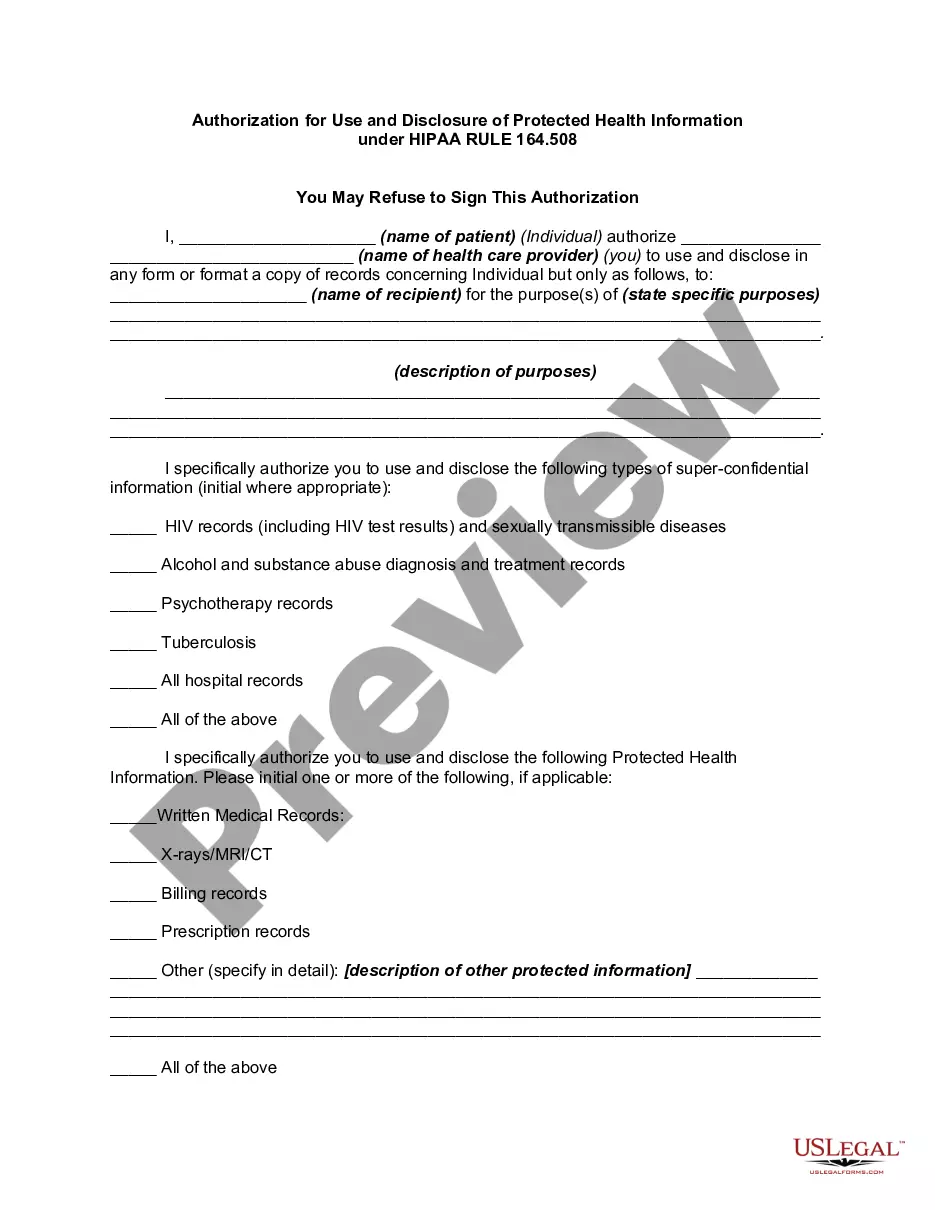
Under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the Privacy Regulations written pursuant to the Act, the general rule is that covered entities may not use or disclose an individual's protected health information for purposes unrelated to treatment, payment, healthcare operations, or certain defined exceptions without first obtaining the individual's prior written authorization.
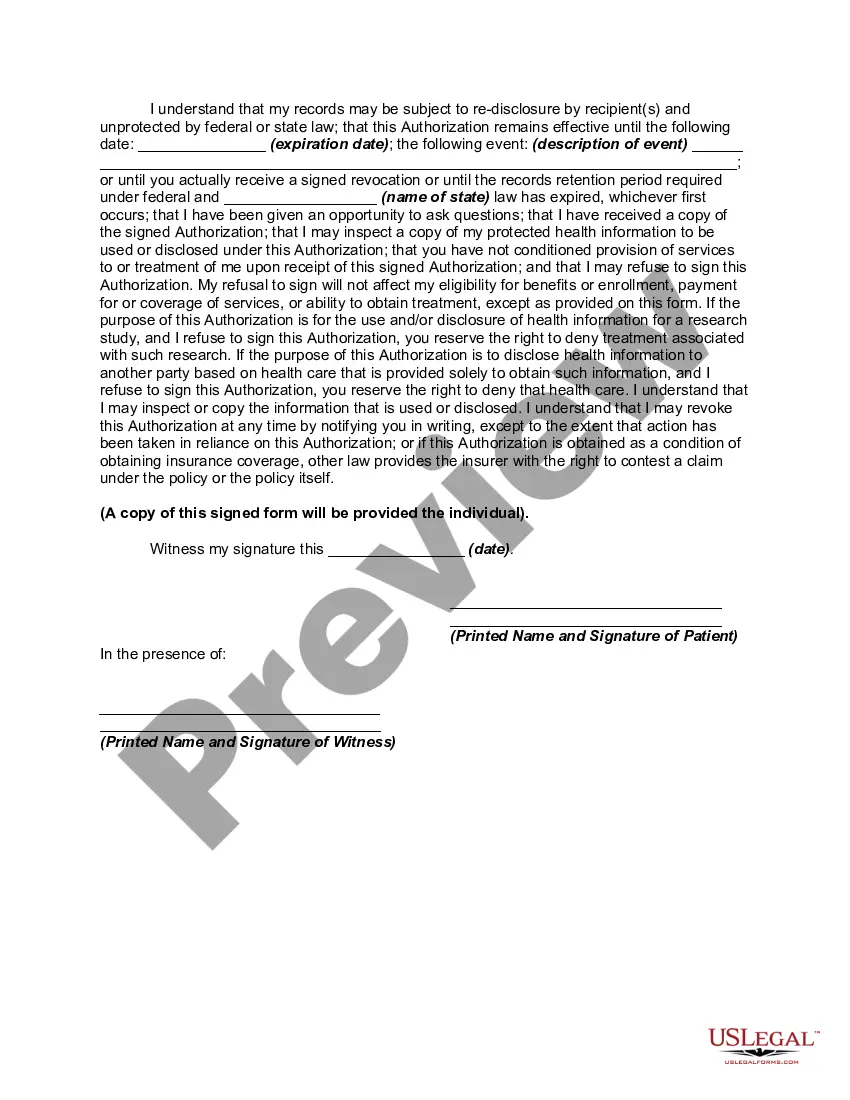
Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508: A Comprehensive Guide In Kentucky, the Authorization for Use and Disclosure of Protected Health Information (PHI) plays a crucial role in ensuring patient privacy and the proper sharing of sensitive medical information. Under the Health Insurance Portability and Accountability Act (HIPAA) Rule 164.508, patients have the right to control how their PHI is used and disclosed by healthcare providers or organizations. This detailed description will provide a comprehensive overview of the Kentucky Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508, highlighting its significance and addressing any types that may exist. The Kentucky Authorization for Use and Disclosure of PHI is a legal document that allows individuals to grant or deny permission for healthcare providers, health plans, or other covered entities to use and disclose their PHI for specific purposes. This authorization empowers patients to maintain control over their personal health information and make informed decisions about its disclosure. Key terms and concepts related to Kentucky Authorization for Use and Disclosure of PHI include: 1. Protected Health Information (PHI): PHI refers to any individually identifiable health information that is transmitted or maintained by a covered entity. This includes medical records, test results, treatment information, billing information, and any other health-related information. 2. Use and Disclosure: Use refers to the internal sharing of PHI within a healthcare organization for activities such as treatment, payment, and healthcare operations. Disclosure, on the other hand, involves the external sharing of PHI with individuals, organizations, or entities outside the covered entity. 3. Authorization: An authorization is a form or written document signed by the patient that grants permission to use or disclose specific PHI for a particular purpose or to a specific recipient. The Kentucky Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508 outlines the permissible uses and disclosures and must adhere to the standards set forth by HIPAA. Types of Kentucky Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508: While there may not be specific types of Kentucky Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508, it's essential to understand that the authorization may vary based on the purpose or entity involved. Here are some instances where an authorization may be required: 1. Research studies: When PHI is needed for research purposes, individuals may be asked to sign an authorization that specifies how their information will be used, who will have access to it, and how privacy will be maintained. 2. Marketing activities: If a healthcare provider, health plan, or third-party entity intends to use PHI for marketing purposes, a specific authorization is required, giving patients the choice to opt-in or opt-out of such activities. 3. Psychotherapy notes: To access and disclose psychotherapy notes, which are separate from regular medical records, a specific authorization is necessary as they contain sensitive information from mental health sessions. 4. Substance abuse treatment: In cases of substance abuse treatment, a separate authorization may be required due to additional privacy protections provided by federal regulations such as the Confidentiality of Substance Use Disorder Patient Records (42 CFR Part 2). It is important to note that these examples are not exhaustive, and there may be other situations where a Kentucky Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508 is required. In conclusion, the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA Rule 164.508 gives individuals control over their PHI and ensures that healthcare providers and organizations adhere to privacy regulations. While various instances may require specific authorizations, the overall goal is to protect patient privacy, promote transparency, and facilitate the appropriate sharing of health information within the legal framework established by HIPAA.Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508: A Comprehensive Guide In Kentucky, the Authorization for Use and Disclosure of Protected Health Information (PHI) plays a crucial role in ensuring patient privacy and the proper sharing of sensitive medical information. Under the Health Insurance Portability and Accountability Act (HIPAA) Rule 164.508, patients have the right to control how their PHI is used and disclosed by healthcare providers or organizations. This detailed description will provide a comprehensive overview of the Kentucky Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508, highlighting its significance and addressing any types that may exist. The Kentucky Authorization for Use and Disclosure of PHI is a legal document that allows individuals to grant or deny permission for healthcare providers, health plans, or other covered entities to use and disclose their PHI for specific purposes. This authorization empowers patients to maintain control over their personal health information and make informed decisions about its disclosure. Key terms and concepts related to Kentucky Authorization for Use and Disclosure of PHI include: 1. Protected Health Information (PHI): PHI refers to any individually identifiable health information that is transmitted or maintained by a covered entity. This includes medical records, test results, treatment information, billing information, and any other health-related information. 2. Use and Disclosure: Use refers to the internal sharing of PHI within a healthcare organization for activities such as treatment, payment, and healthcare operations. Disclosure, on the other hand, involves the external sharing of PHI with individuals, organizations, or entities outside the covered entity. 3. Authorization: An authorization is a form or written document signed by the patient that grants permission to use or disclose specific PHI for a particular purpose or to a specific recipient. The Kentucky Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508 outlines the permissible uses and disclosures and must adhere to the standards set forth by HIPAA. Types of Kentucky Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508: While there may not be specific types of Kentucky Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508, it's essential to understand that the authorization may vary based on the purpose or entity involved. Here are some instances where an authorization may be required: 1. Research studies: When PHI is needed for research purposes, individuals may be asked to sign an authorization that specifies how their information will be used, who will have access to it, and how privacy will be maintained. 2. Marketing activities: If a healthcare provider, health plan, or third-party entity intends to use PHI for marketing purposes, a specific authorization is required, giving patients the choice to opt-in or opt-out of such activities. 3. Psychotherapy notes: To access and disclose psychotherapy notes, which are separate from regular medical records, a specific authorization is necessary as they contain sensitive information from mental health sessions. 4. Substance abuse treatment: In cases of substance abuse treatment, a separate authorization may be required due to additional privacy protections provided by federal regulations such as the Confidentiality of Substance Use Disorder Patient Records (42 CFR Part 2). It is important to note that these examples are not exhaustive, and there may be other situations where a Kentucky Authorization for Use and Disclosure of PHI under HIPAA Rule 164.508 is required. In conclusion, the Kentucky Authorization for Use and Disclosure of Protected Health Information under HIPAA Rule 164.508 gives individuals control over their PHI and ensures that healthcare providers and organizations adhere to privacy regulations. While various instances may require specific authorizations, the overall goal is to protect patient privacy, promote transparency, and facilitate the appropriate sharing of health information within the legal framework established by HIPAA.