Kentucky Sample COBRA Enrollment and / or Waiver Letter
Description
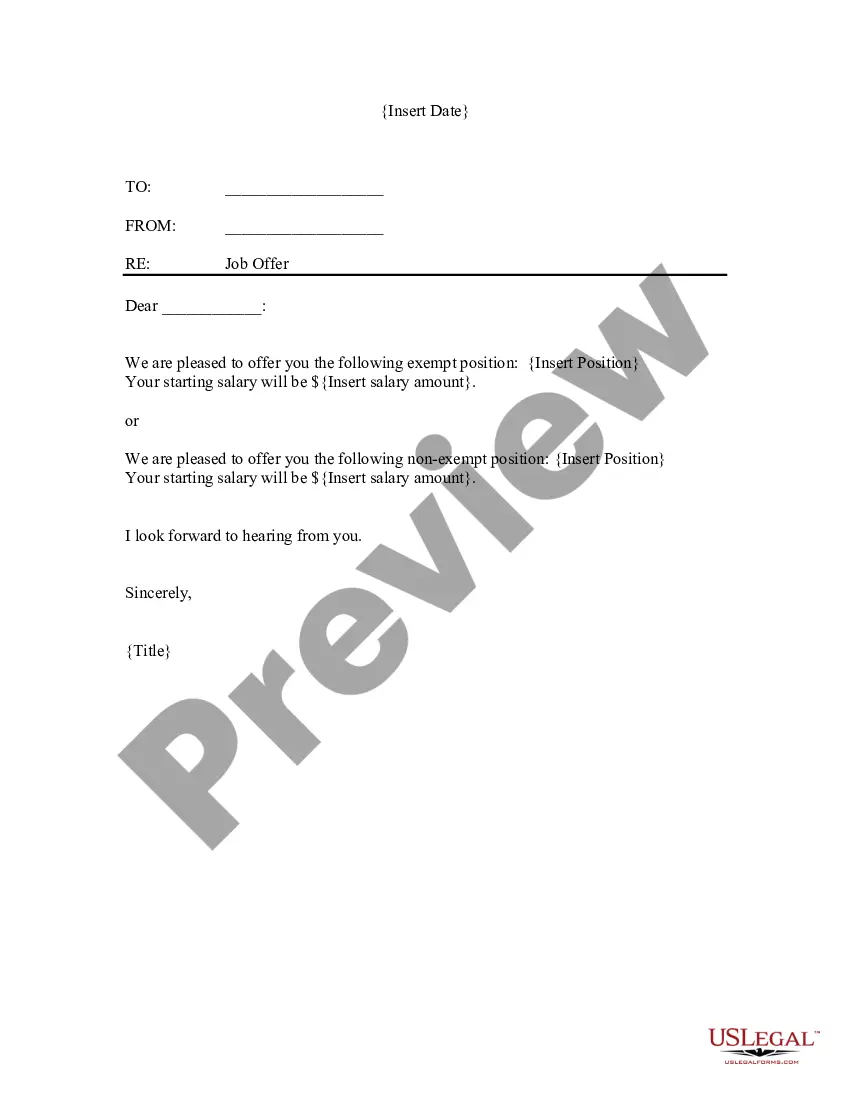
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
Are you inside a position where you will need documents for possibly organization or individual functions nearly every time? There are tons of legal papers web templates available on the Internet, but finding versions you can rely on isn`t effortless. US Legal Forms gives a huge number of form web templates, just like the Kentucky Sample COBRA Enrollment and / or Waiver Letter, which are composed to satisfy state and federal specifications.
In case you are currently knowledgeable about US Legal Forms web site and get an account, basically log in. Following that, you may obtain the Kentucky Sample COBRA Enrollment and / or Waiver Letter format.
If you do not come with an account and want to begin to use US Legal Forms, abide by these steps:
- Discover the form you require and ensure it is to the proper area/region.
- Take advantage of the Preview button to examine the shape.
- Read the explanation to ensure that you have chosen the proper form.
- If the form isn`t what you`re trying to find, utilize the Look for industry to get the form that suits you and specifications.
- Once you find the proper form, click on Buy now.
- Choose the rates program you desire, complete the necessary details to create your account, and purchase your order using your PayPal or charge card.
- Select a hassle-free file file format and obtain your version.
Find every one of the papers web templates you may have bought in the My Forms food list. You can aquire a more version of Kentucky Sample COBRA Enrollment and / or Waiver Letter at any time, if necessary. Just click on the necessary form to obtain or printing the papers format.
Use US Legal Forms, by far the most comprehensive assortment of legal varieties, to save lots of efforts and steer clear of blunders. The services gives appropriately manufactured legal papers web templates that you can use for a variety of functions. Make an account on US Legal Forms and commence making your daily life a little easier.
Form popularity
FAQ
When does COBRA continuation coverage startCOBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
How long would my continued coverage be in effect? If you qualify for state continuation, you and your dependents can extend your group health insurance for 18 months after the date on which the coverage would have ended because you were no longer a group member.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
Does COBRA Count as Creditable Coverage for Medicare? To avoid penalties with Medicare, you must have creditable coverage. This means coverage that's at least equivalent to Medicare. COBRA does NOT meet these standards.