Kentucky Individual Notice of Preexisting Condition Exclusion
Description
How to fill out Individual Notice Of Preexisting Condition Exclusion?
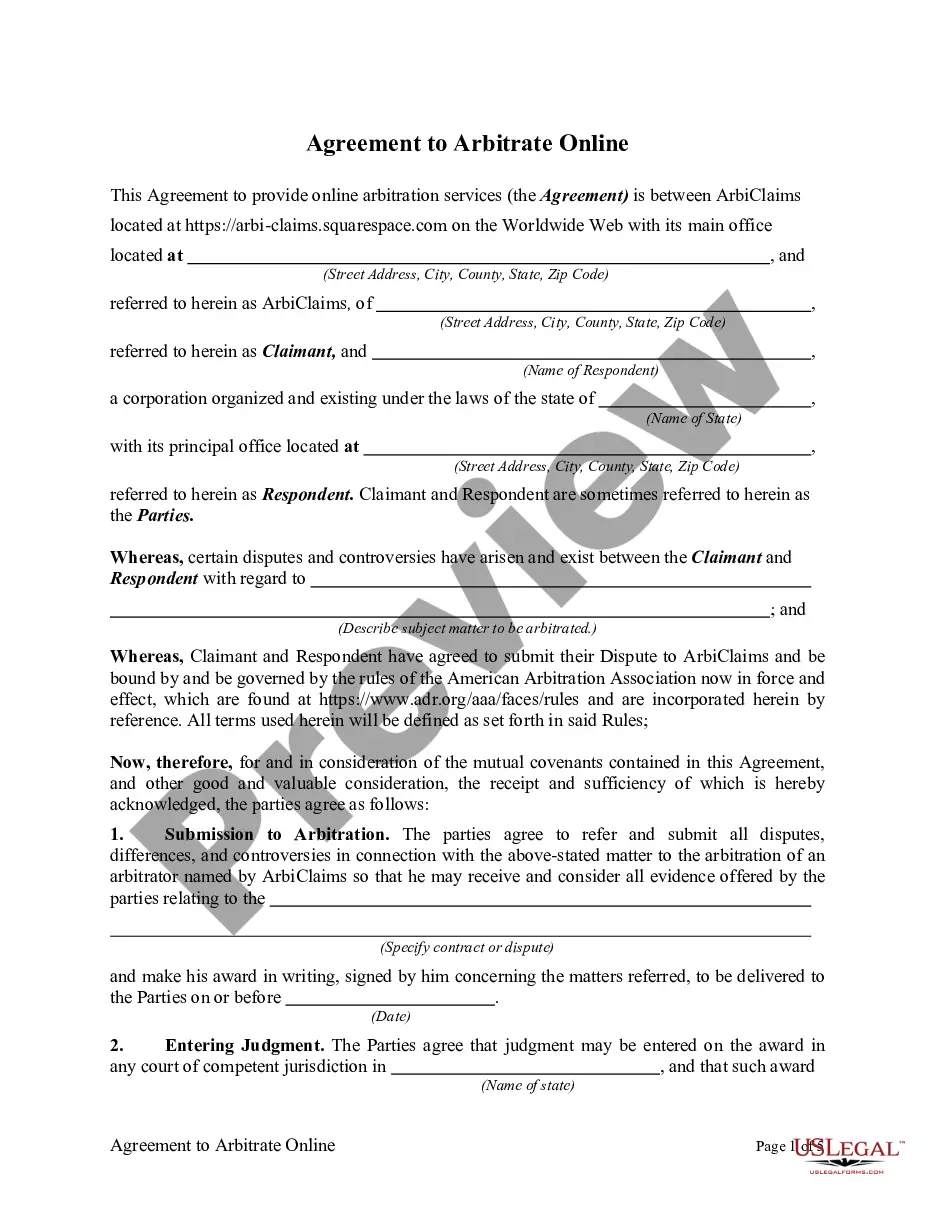
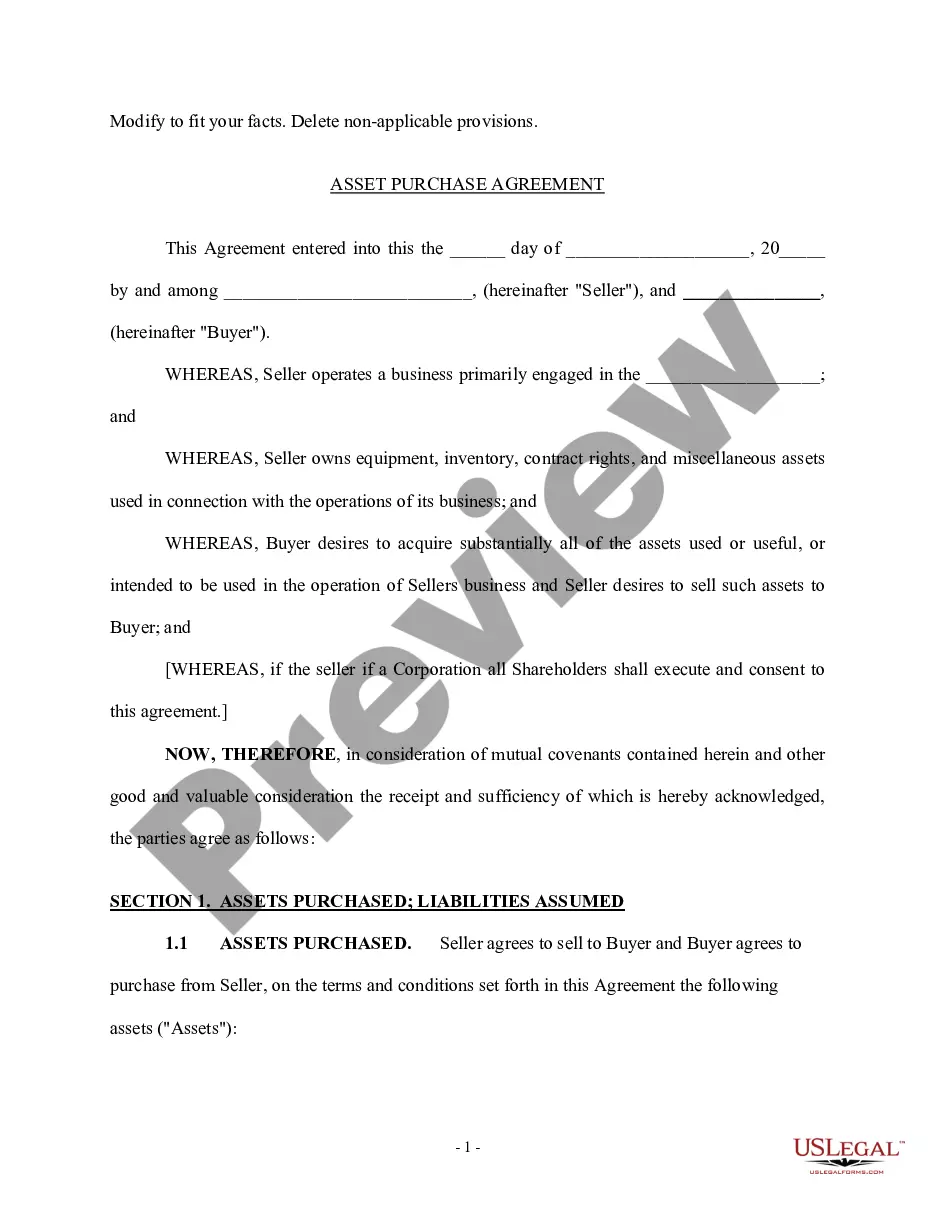
Choosing the right legal document format can be a have a problem. Needless to say, there are plenty of layouts available online, but how would you obtain the legal kind you need? Make use of the US Legal Forms internet site. The services gives a large number of layouts, like the Kentucky Individual Notice of Preexisting Condition Exclusion, which you can use for organization and private needs. Every one of the varieties are examined by specialists and fulfill federal and state specifications.
If you are presently authorized, log in for your accounts and then click the Down load button to obtain the Kentucky Individual Notice of Preexisting Condition Exclusion. Make use of your accounts to search through the legal varieties you have acquired previously. Go to the My Forms tab of the accounts and get another backup of the document you need.
If you are a whole new user of US Legal Forms, listed below are easy guidelines that you can comply with:
- Initially, make sure you have chosen the appropriate kind for the metropolis/county. You may look over the shape using the Review button and study the shape outline to guarantee this is basically the right one for you.
- When the kind does not fulfill your needs, take advantage of the Seach area to find the proper kind.
- When you are sure that the shape would work, go through the Get now button to obtain the kind.
- Opt for the costs prepare you want and enter in the essential details. Create your accounts and pay money for the order utilizing your PayPal accounts or bank card.
- Choose the document format and download the legal document format for your device.
- Full, revise and produce and sign the acquired Kentucky Individual Notice of Preexisting Condition Exclusion.
US Legal Forms may be the greatest collection of legal varieties that you can discover various document layouts. Make use of the company to download professionally-produced documents that comply with express specifications.
Form popularity
FAQ
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
What Is the Pre-existing Condition Exclusion Period? The pre-existing condition exclusion period is a health insurance provision that limits or excludes benefits for a period of time. The determination is based on the policyholder having a medical condition prior to enrolling in a health plan.
If you had a pre-existing condition exclusion period, you didn't have coverage for any care or services related to your pre-existing condition for a predetermined amount of time, despite paying your monthly premiums.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
Yes. Under the Affordable Care Act, health insurance companies can't refuse to cover you or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts. They also can't charge women more than men.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.