The Kentucky Notice of Special Enrollment Rights is an essential document that provides important information about the rights and options available to individuals residing in Kentucky to enroll in or change health insurance coverage outside the usual open enrollment period. This notice aims to educate and empower residents by outlining specific circumstances in which they may be eligible to enroll or alter their existing insurance plans. One type of Kentucky Notice of Special Enrollment Rights is the notice for individuals who recently experienced a qualifying life event. These events include marriage, divorce, birth or adoption of a child, loss of previous health coverage, or a change in employment status. By promptly notifying the insurance provider within a specified timeframe, individuals can seize the opportunity to enroll in or switch to another healthcare plan that better suits their evolving needs. Another form of the Kentucky Notice of Special Enrollment Rights pertains to those eligible for Medicaid or the Children's Health Insurance Program (CHIP). This notice ensures that individuals who become eligible for these government programs are made aware of the rights and options available to them. It emphasizes the importance of timely enrollment and explains the steps to follow to secure proper coverage and access to healthcare services. In addition to the above, the Kentucky Notice of Special Enrollment Rights may also cover specific guidelines for those who experienced a loss of minimum essential coverage, such as job loss or expiration of COBRA coverage. It educates individuals on the significance of maintaining continuous coverage to avoid potential penalties and highlights the options for obtaining new insurance during such transitional periods. Keywords: Kentucky, Notice of Special Enrollment Rights, health insurance coverage, open enrollment period, qualifying life event, marriage, divorce, birth, adoption, loss of previous health coverage, change in employment status, insurance provider, healthcare plan, Medicaid, Children's Health Insurance Program (CHIP), government programs, timely enrollment, access to healthcare services, loss of minimum essential coverage, COBRA coverage, continuous coverage, penalties.
Kentucky Notice of Special Enrollment Rights
Description
How to fill out Kentucky Notice Of Special Enrollment Rights?
If you have to full, acquire, or printing lawful file web templates, use US Legal Forms, the largest variety of lawful forms, which can be found on-line. Use the site`s easy and convenient search to obtain the files you require. Different web templates for enterprise and personal functions are categorized by categories and states, or search phrases. Use US Legal Forms to obtain the Kentucky Notice of Special Enrollment Rights within a number of clicks.
When you are presently a US Legal Forms customer, log in to your account and click on the Download option to find the Kentucky Notice of Special Enrollment Rights. You can also entry forms you previously saved inside the My Forms tab of the account.
Should you use US Legal Forms the very first time, follow the instructions below:
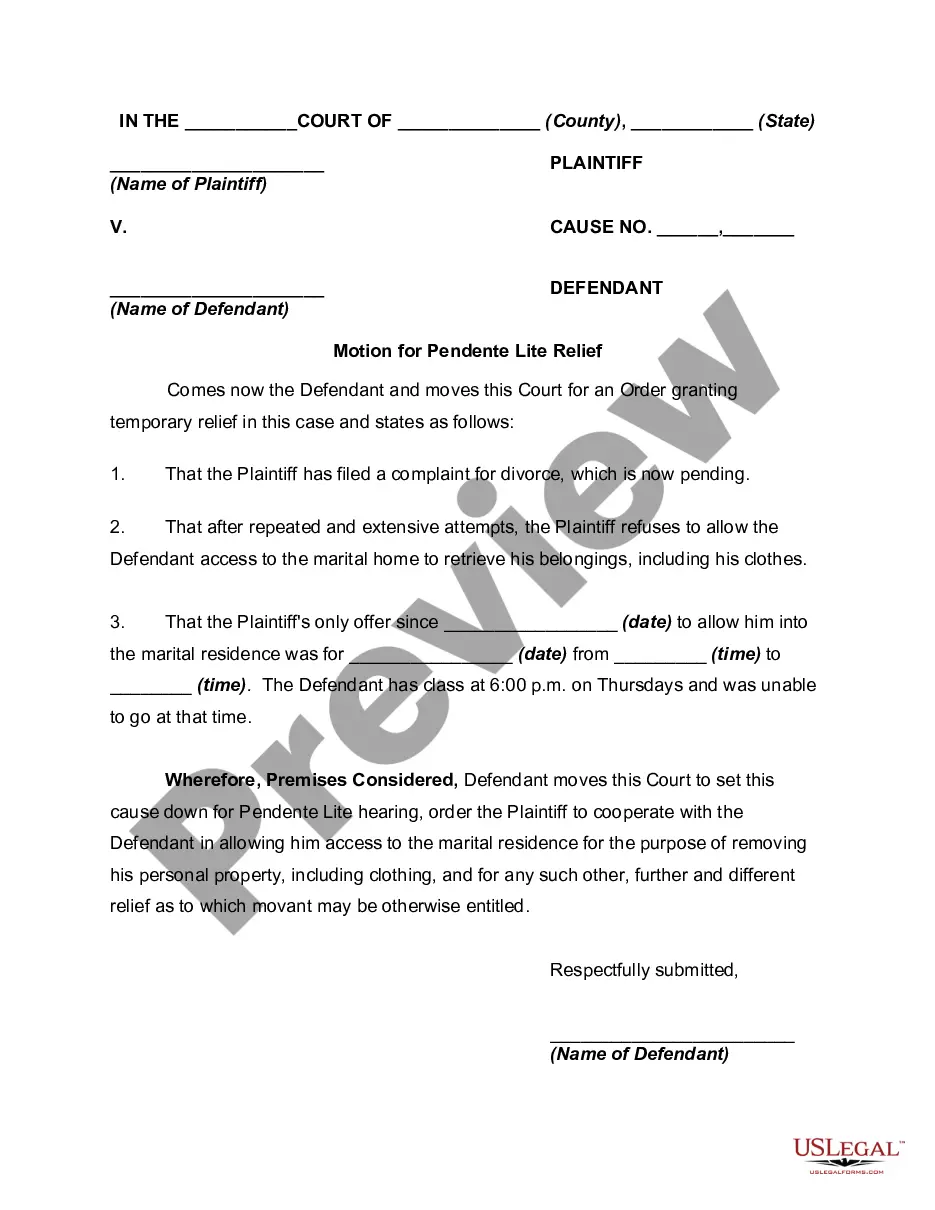
- Step 1. Be sure you have selected the shape for the right metropolis/country.
- Step 2. Take advantage of the Review choice to examine the form`s information. Don`t neglect to read the explanation.
- Step 3. When you are unsatisfied using the develop, utilize the Research industry towards the top of the display screen to find other types from the lawful develop template.
- Step 4. Upon having identified the shape you require, click the Get now option. Choose the costs plan you like and add your accreditations to sign up to have an account.
- Step 5. Process the financial transaction. You may use your Мisa or Ьastercard or PayPal account to complete the financial transaction.
- Step 6. Pick the formatting from the lawful develop and acquire it on your product.
- Step 7. Full, change and printing or signal the Kentucky Notice of Special Enrollment Rights.
Every single lawful file template you buy is your own for a long time. You have acces to every develop you saved with your acccount. Click on the My Forms portion and decide on a develop to printing or acquire yet again.
Contend and acquire, and printing the Kentucky Notice of Special Enrollment Rights with US Legal Forms. There are many specialist and condition-distinct forms you can use for your personal enterprise or personal needs.