In response to growing concerns about keeping health information private, Congress passed the Health Insurance Portability and Accountability Act of 1996 (HIPAA). The legislation includes a privacy rule that creates national standards to protect individuals' personal health information.
HIPAA, requires health care professionals to protect privacy and create standards for electronic transfers of health data. HIPAA came about because of the public's concern about how health care information is used. HIPAA gives patients more control over their own health information. HIPAA requires health care providers to follow certain rules to protect the privacy of patients' health information. For instance, employees are not allowed to access information on patients unless they need the information to perform their jobs.
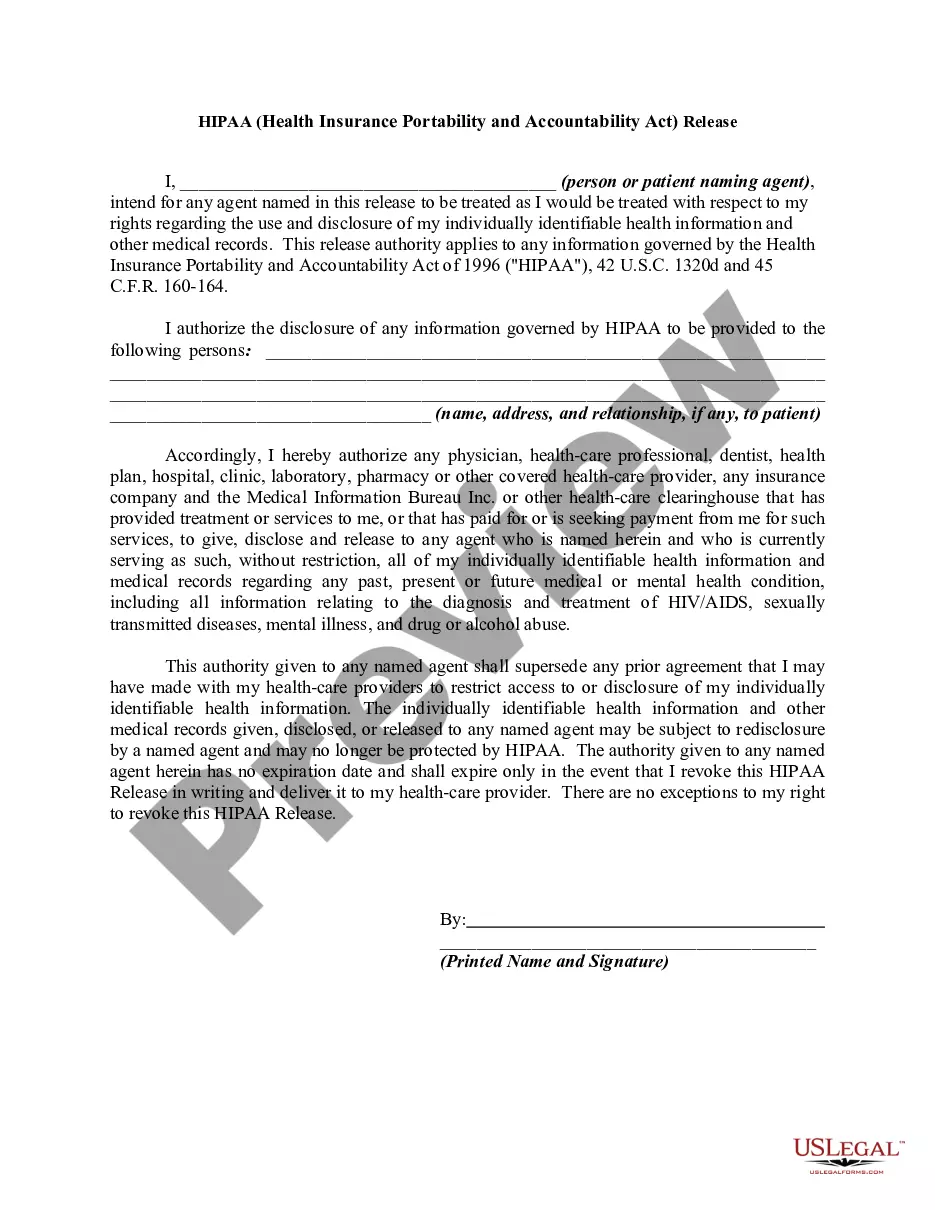
The Massachusetts HIPAA, which stands for Health Insurance Portability and Accountability Act, includes specific guidelines and regulations regarding the release of personal health information to third parties. This act is designed to ensure the privacy and security of individuals' medical records and to protect their confidential information. The Authorization to Release Information to a Third Party is an essential aspect of HIPAA compliance in Massachusetts. It grants consent for healthcare providers, insurers, or other covered entities to disclose an individual's protected health information (PHI) to a third party. This authorization is necessary when sharing medical records, test results, treatment plans, or any other PHI with individuals or organizations not directly involved in the person's healthcare. Keywords related to the Massachusetts HIPAA — Health Insurance Portability and Accountability Act Releaseas— - Authorization to Release Information to a Third Party include: 1. HIPAA Compliance: The adherence to the regulations and requirements outlined in HIPAA to protect the privacy and security of an individual's health information. 2. Protected Health Information (PHI): Any individually identifiable health information that is created or received by a healthcare provider, insurer, or other covered entity. It includes medical records, billing information, and other personal health details. 3. Authorization: A written permission signed by an individual that allows a covered entity to disclose their PHI to a third party. 4. Release of Information: The process of sharing an individual's PHI with a third party, as permitted under the HIPAA regulations. 5. Third Party: An individual or organization that is not directly involved in the provision of healthcare but may require access to an individual's PHI for valid reasons, such as insurance companies, legal representatives, or researchers. In Massachusetts, there are no specific types of Release- Authorization forms under the state HIPAA regulations. However, HIPAA compliance requires that any authorization to release PHI must contain specific elements, including a clear description of the information being released, the purpose of the disclosure, the names of the entities involved, and an expiration date if applicable. It is important for healthcare providers, insurers, and covered entities in Massachusetts to familiarize themselves with the state-specific HIPAA regulations and ensure they have proper procedures and documentation in place for authorizing the release of information to a third party. This helps to maintain patient privacy, protect sensitive health information, and comply with HIPAA rules and guidelines.