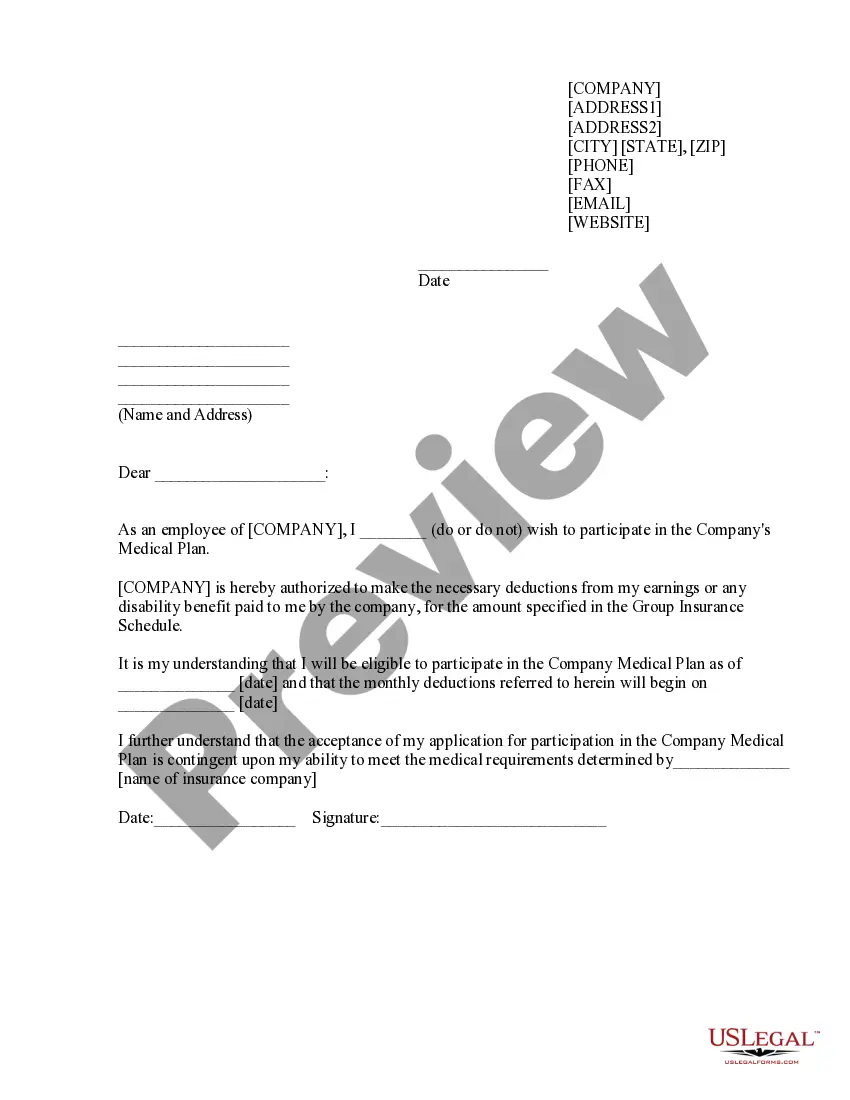
Massachusetts Sample COBRA Enrollment and / or Waiver Letter
Description
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
US Legal Forms - one of the largest repositories of legal documents in the United States - offers a variety of legal form templates that you can download or print.
By utilizing the site, you can discover countless forms for business and personal purposes, organized by categories, states, or keywords.
You can find the latest forms such as the Massachusetts Sample COBRA Enrollment and/or Waiver Letter in just a few minutes.
Examine the form details to confirm that you have selected the appropriate form.
If the form does not match your requirements, utilize the Search section at the top of the screen to find one that does.
- If you already possess a monthly subscription, Log In and acquire the Massachusetts Sample COBRA Enrollment and/or Waiver Letter from the US Legal Forms library.
- The Download button will be visible on each form you view.
- You have access to all previously downloaded forms in the My documents section of your account.
- To utilize US Legal Forms for the first time, here are straightforward instructions to assist you in getting started.
- Ensure you have selected the correct form for your locality/region.
- Click the Preview button to review the form's content.
Form popularity
FAQ
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.
If you waive COBRA coverage during the election period, you must be permitted later to revoke your waiver of coverage and to elect continuation coverage as long as you do so during the election period. Then, the plan need only provide continuation coverage beginning on the date you revoke the waiver.
Massachusetts Has Mini-COBRA COBRA applies to self-funded and group plans offered by employers with 20 or more employees. Mini-COBRA does not apply to self-funded plans.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
If you are an employee of the Commonwealth of Massachusetts, you have the right to choose COBRA coverage if you lose your group health coverage because your hours of employment are reduced or your employment ends for reasons other than gross misconduct.
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
Most state COBRA laws extend the qualifying employer definition to as low as 2 full-time employees....States with Mini-COBRA Expansions as of January 1, 2017:Arkansas.California.Colorado.Connecticut.District of Columbia.Florida.Georgia.Illinois.More items...
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive. You are now responsible for the entire insurance premium, whereas your previous employer subsidized a portion of that as a work benefit.
COBRA is a federal law and is not enforced by the Division of Insurance. Mini-COBRA is a state law and is enforced by the Division of Insurance. COBRA generally applies to group health plans offered by employers with 20 or more employees.