Massachusetts Notice of Qualifying Event from Employer to Plan Administrator is a legal document that serves as a formal notification from an employer to the plan administrator regarding a qualifying event that has occurred within a Massachusetts employee benefit plan. This notice is required under the Massachusetts Consolidated Omnibus Budget Reconciliation Act (COBRA) laws. When an employee experiences a qualifying event, such as termination of employment, reduction in hours, or divorce of a covered employee, they may be eligible to continue their health insurance coverage. The Massachusetts Notice of Qualifying Event from Employer to Plan Administrator is a crucial step in initiating the COBRA process and ensuring that the affected employee is provided with the necessary information and opportunities to maintain their health insurance coverage. The notice typically includes important details such as: 1. Employer Information: The name, address, and contact information of the employer providing the notice. 2. Plan Administrator Information: The name, address, and contact information of the plan administrator responsible for administering the employee benefit plan. 3. Employee Information: The name, address, and contact information of the employee who experienced the qualifying event. 4. Qualifying Event Details: A clear description of the qualifying event that occurred, such as termination of employment, reduction in hours, or divorce. 5. COBRA Coverage Information: Information regarding the employee's right to elect continuation of health insurance coverage under COBRA, including the duration of coverage, premium costs, and deadlines for enrollment. Massachusetts has specific guidelines and deadlines that employers must adhere to when providing the Notice of Qualifying Event from Employer to Plan Administrator. Failure to provide the notice in a timely and accurate manner can result in penalties and legal consequences. There may be different types of Massachusetts Notice of Qualifying Event from Employer to Plan Administrator based on the qualifying event that has occurred. Some common types of qualifying events include: 1. Termination of Employment: When an employee's employment is terminated by the employer, excluding termination due to gross misconduct. 2. Reduction in Hours: When an employee's hours are reduced below the minimum threshold required for health insurance eligibility. 3. Divorce or Legal Separation: When an employee's spouse or dependent loses coverage due to divorce or legal separation. 4. Death of Covered Employee: When the covered employee passes away, triggering a qualifying event for their dependents. Each type of qualifying event may require specific information and documentation to be included in the Massachusetts Notice of Qualifying Event from Employer to Plan Administrator. In conclusion, the Massachusetts Notice of Qualifying Event from Employer to Plan Administrator is a vital document that notifies the plan administrator about an eligible employee's qualifying event, triggering their rights to continue health insurance coverage under COBRA. Employers must understand the specific requirements and deadlines associated with this notice to ensure compliance with Massachusetts employer health insurance laws.
Massachusetts Notice of Qualifying Event from Employer to Plan Administrator
Description
How to fill out Massachusetts Notice Of Qualifying Event From Employer To Plan Administrator?
US Legal Forms - one of the greatest libraries of legal types in America - provides a wide array of legal file templates you can acquire or print out. Making use of the website, you can get a large number of types for enterprise and personal functions, categorized by groups, says, or keywords and phrases.You can find the most up-to-date models of types just like the Massachusetts Notice of Qualifying Event from Employer to Plan Administrator within minutes.
If you already have a membership, log in and acquire Massachusetts Notice of Qualifying Event from Employer to Plan Administrator through the US Legal Forms library. The Obtain button will appear on each kind you perspective. You gain access to all formerly downloaded types within the My Forms tab of your own profile.
If you wish to use US Legal Forms the first time, listed here are basic recommendations to help you began:
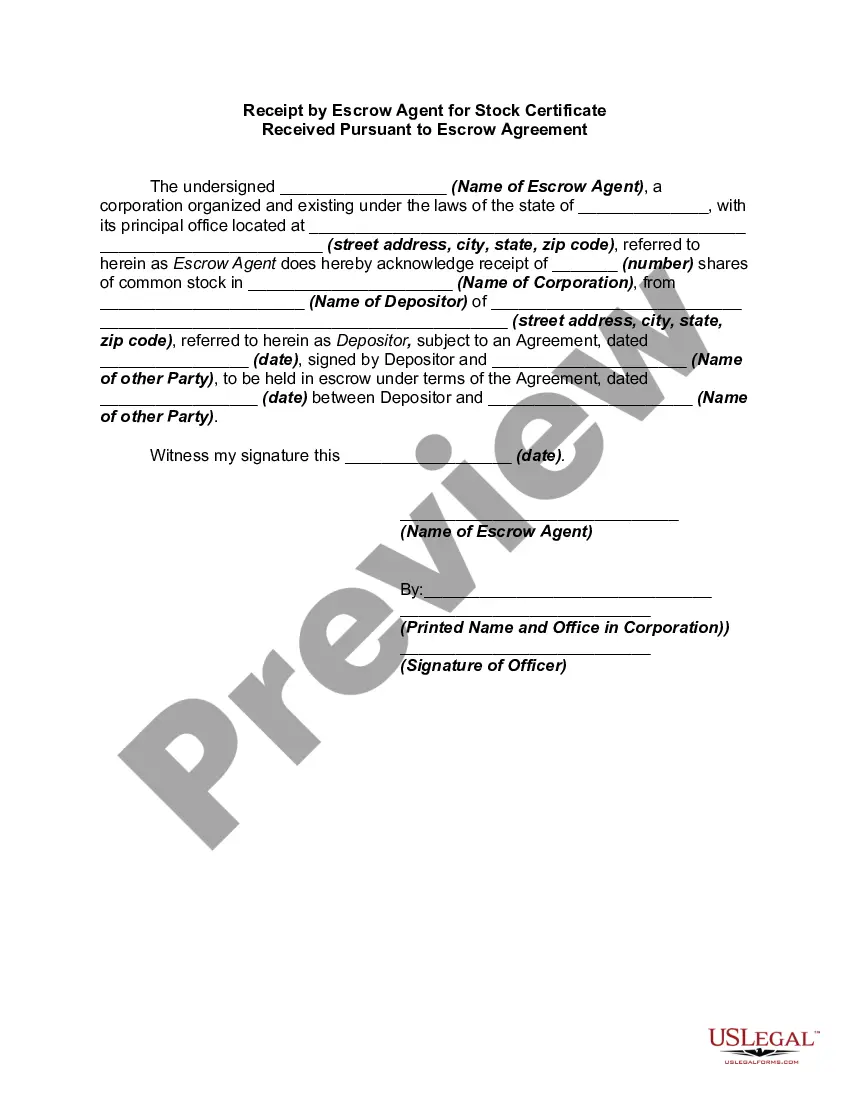
- Be sure you have selected the best kind for your personal metropolis/region. Go through the Review button to examine the form`s articles. Read the kind explanation to ensure that you have chosen the right kind.
- When the kind does not suit your requirements, make use of the Look for industry towards the top of the display screen to discover the the one that does.
- When you are happy with the form, affirm your decision by clicking on the Purchase now button. Then, select the costs prepare you prefer and supply your qualifications to sign up on an profile.
- Approach the financial transaction. Use your credit card or PayPal profile to accomplish the financial transaction.
- Select the format and acquire the form on your device.
- Make adjustments. Complete, revise and print out and indication the downloaded Massachusetts Notice of Qualifying Event from Employer to Plan Administrator.
Each and every format you included in your bank account lacks an expiration day and is your own property eternally. So, if you want to acquire or print out an additional version, just visit the My Forms section and then click about the kind you require.
Get access to the Massachusetts Notice of Qualifying Event from Employer to Plan Administrator with US Legal Forms, by far the most extensive library of legal file templates. Use a large number of specialist and condition-distinct templates that satisfy your company or personal demands and requirements.