The Massachusetts Individual Notice of Preexisting Condition Exclusion is a crucial aspect of health insurance within the state. This notice is designed to inform individuals about any potential exclusions or limitations that may apply to their coverage due to preexisting conditions. A preexisting condition refers to a health condition, illness, or injury that an individual already had before obtaining health insurance coverage. These conditions may include chronic illnesses, such as diabetes, asthma, heart disease, or any other ongoing medical issue. It is important to note that preexisting condition exclusions are prohibited under the Affordable Care Act (ACA) for most health insurance plans, including those in Massachusetts. However, in Massachusetts, individuals may still encounter limited situations where preexisting condition exclusions apply. These exclusions may typically arise when an individual enrolls in a new health plan outside of specific enrollment periods, such as during special enrollment or after losing existing coverage. Insurance companies in Massachusetts must comply with certain regulations when implementing preexisting condition exclusions. They are required to provide clear and detailed information through the Individual Notice of Preexisting Condition Exclusion. This notice serves to educate policyholders about what conditions, if any, are subject to exclusion and the duration of such exclusions. Some mandatory elements covered in the notice may include the name of the individual, the specific condition(s) subject to exclusion, the start and end dates of the exclusion period, and any additional limitations or waiting periods that may apply. The notice should be provided to policyholders in writing, ensuring they have ample time to review and understand the information before making important healthcare decisions. It is important to be aware that Massachusetts law strictly regulates the use of preexisting condition exclusions, ensuring transparency and fairness in health insurance practices. Different types of Individual Notice of Preexisting Condition Exclusion may exist, depending on the insurance carrier or specific plan. However, these notices must all comply with the state's regulations and provide accurate information for policyholders. In summary, the Massachusetts Individual Notice of Preexisting Condition Exclusion is a vital document that individuals receiving health insurance should review carefully. It outlines any potential exclusions or limitations based on preexisting conditions, ensuring that policyholders are well-informed about their coverage and any variations that may apply.
Massachusetts Individual Notice of Preexisting Condition Exclusion
Description
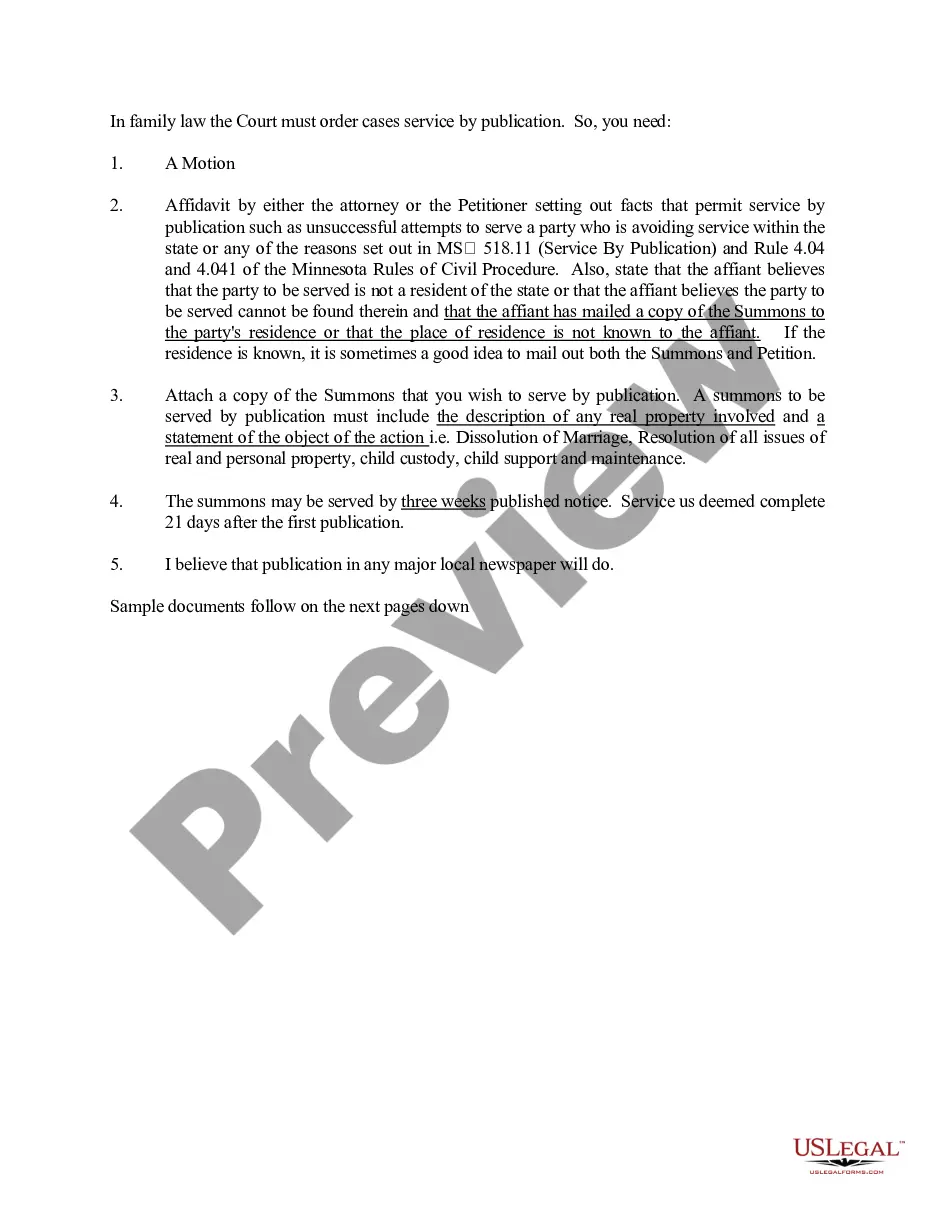
How to fill out Massachusetts Individual Notice Of Preexisting Condition Exclusion?
Are you in the situation the place you require files for sometimes company or individual purposes virtually every working day? There are a lot of authorized document themes available on the net, but finding ones you can depend on is not easy. US Legal Forms offers 1000s of develop themes, like the Massachusetts Individual Notice of Preexisting Condition Exclusion, which are written in order to meet state and federal needs.
If you are presently acquainted with US Legal Forms site and get an account, just log in. After that, you may download the Massachusetts Individual Notice of Preexisting Condition Exclusion design.
Unless you provide an bank account and want to start using US Legal Forms, abide by these steps:
- Get the develop you will need and make sure it is for the correct metropolis/area.
- Take advantage of the Preview button to review the form.
- Read the explanation to ensure that you have chosen the correct develop.
- In the event the develop is not what you are searching for, take advantage of the Research field to discover the develop that suits you and needs.
- Once you discover the correct develop, simply click Purchase now.
- Pick the prices program you desire, fill in the required information and facts to create your money, and buy the order with your PayPal or charge card.
- Decide on a hassle-free data file formatting and download your version.
Locate all of the document themes you might have purchased in the My Forms menus. You can aquire a more version of Massachusetts Individual Notice of Preexisting Condition Exclusion whenever, if required. Just select the essential develop to download or print out the document design.
Use US Legal Forms, the most substantial collection of authorized kinds, to save lots of efforts and stay away from mistakes. The assistance offers expertly produced authorized document themes which can be used for a range of purposes. Create an account on US Legal Forms and start producing your life a little easier.
Form popularity
FAQ
Yes. Under the Affordable Care Act, health insurance companies can't refuse to cover you or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
Some of the most common pre-existing conditions include thyroid, high blood pressure, diabetes, asthma, cholesterol, etc. Most health insurance companies have a waiting period that can last from a couple of months to a few years before you start covering pre-existing illnesses.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
If you had a pre-existing condition exclusion period, you didn't have coverage for any care or services related to your pre-existing condition for a predetermined amount of time, despite paying your monthly premiums.
In Massachusetts, health plans cannot deny health insurance coverage for an individual because that person has a pre-existing condition. However, health plans can limit coverage of that specific condition for up to six months, unless the person has had continuous health insurance coverage.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
What Is the Pre-existing Condition Exclusion Period? The pre-existing condition exclusion period is a health insurance provision that limits or excludes benefits for a period of time. The determination is based on the policyholder having a medical condition prior to enrolling in a health plan.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.