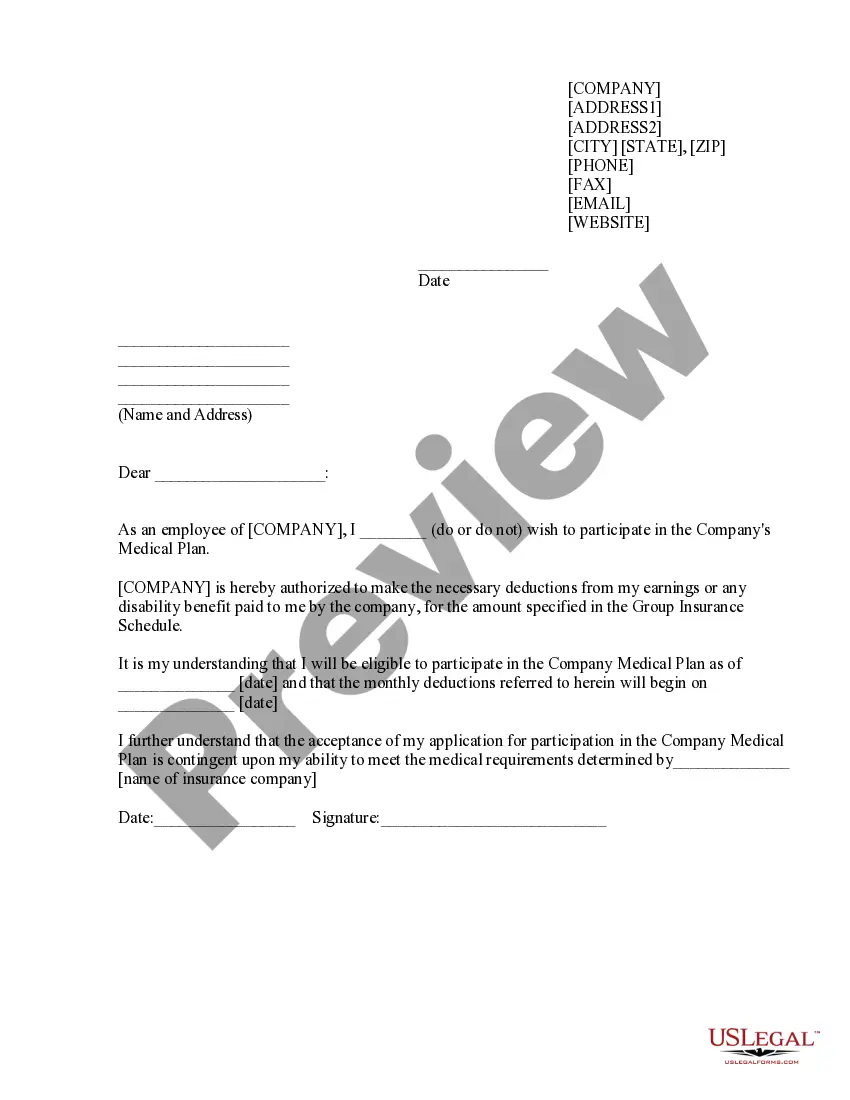
Maryland Sample COBRA Enrollment and / or Waiver Letter
Description
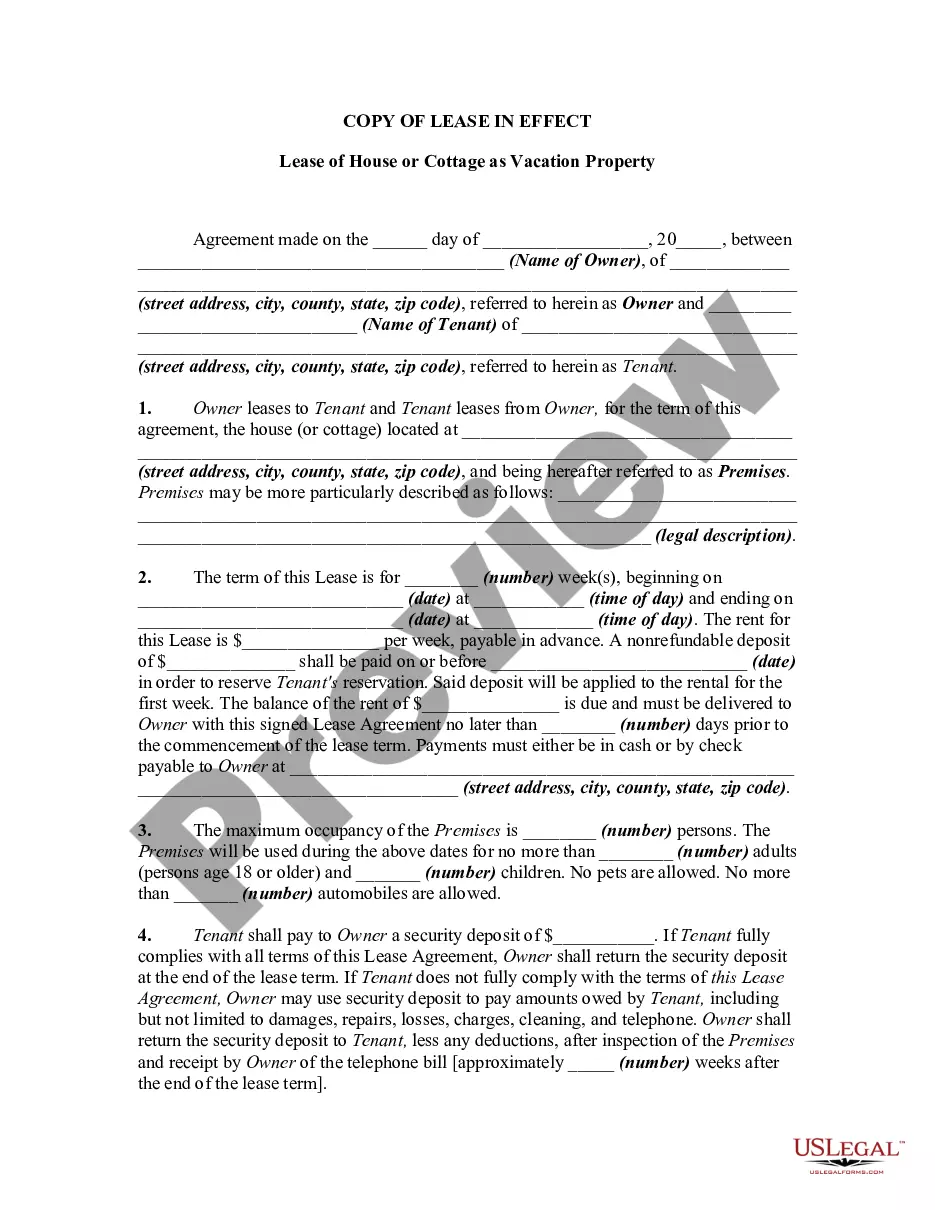
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
You can spend hours online attempting to locate the authentic document template that satisfies the state and federal stipulations you require.
US Legal Forms provides thousands of authentic varieties that can be examined by specialists.
You are able to download or print the Maryland Sample COBRA Enrollment and/or Waiver Letter from the services.
If available, use the Preview button to view the document template as well. If you wish to find another version of your form, utilize the Search field to find the template that meets your needs and preferences.
- If you already possess a US Legal Forms account, you can sign in and click the Obtain button.
- Subsequently, you can complete, modify, print, or sign the Maryland Sample COBRA Enrollment and/or Waiver Letter.
- Every authentic document template you purchase is yours indefinitely.
- To receive another copy of the acquired form, visit the My documents tab and click on the corresponding button.
- If you are accessing the US Legal Forms website for the first time, follow the simple instructions below.
- First, ensure you have selected the appropriate document template for the county/town of your choice.
- Review the form details to confirm you have chosen the correct form.
Form popularity
FAQ
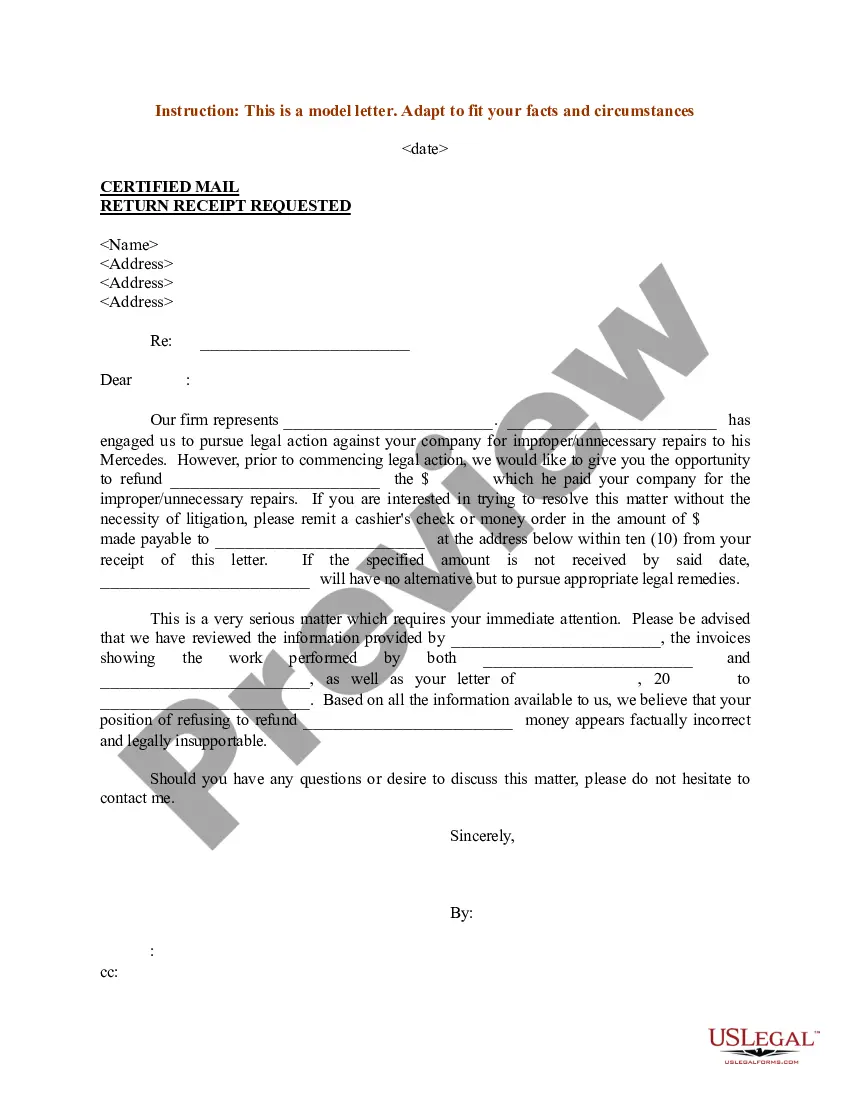
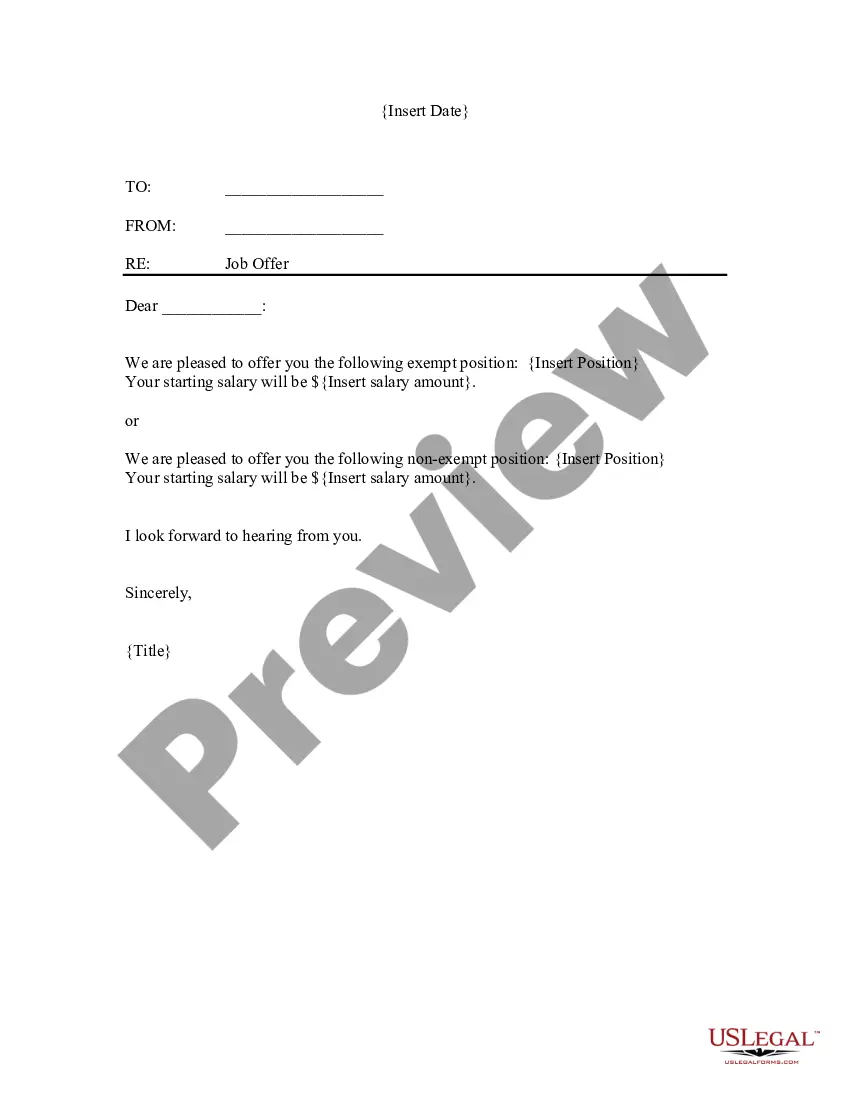
A COBRA letter is drafted by the plan administrator with a copy mailed to each qualified beneficiary before the coverage is terminated. The COBRA termination letter format must include the reason why the coverageis being terminated, the rights of the beneficiaries, and the specific date the coverage will end.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
You May Cancel COBRA At Any Time To cancel your your COBRA coverage you will need to notify your previous employer or the plan administrator in writing. After you stop your COBRA insurance, your former employer should send you a letter affirming termination of that health insurance.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.
The purpose of this letter is to inform you of your rights and responsibilities as a plan participant. Qualifying Event: At the end of your employment or because of reduction of hours (not maintain full-time status) you will receive this letter.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a landmark federal law, passed in 1985, that provides for continuing group health insurance coverage for some employees and their families after a job loss or other qualifying event.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.