Maine COBRA Continuation Coverage Election Notice
Description
How to fill out COBRA Continuation Coverage Election Notice?
Choosing the right legitimate document web template can be a battle. Of course, there are tons of layouts available on the Internet, but how can you obtain the legitimate type you want? Take advantage of the US Legal Forms internet site. The assistance provides thousands of layouts, like the Maine COBRA Continuation Coverage Election Notice, which can be used for organization and personal needs. Every one of the varieties are examined by experts and fulfill federal and state demands.
When you are currently authorized, log in to your profile and then click the Download switch to have the Maine COBRA Continuation Coverage Election Notice. Make use of your profile to search from the legitimate varieties you might have bought earlier. Check out the My Forms tab of the profile and get yet another version of your document you want.
When you are a fresh end user of US Legal Forms, allow me to share straightforward directions for you to adhere to:
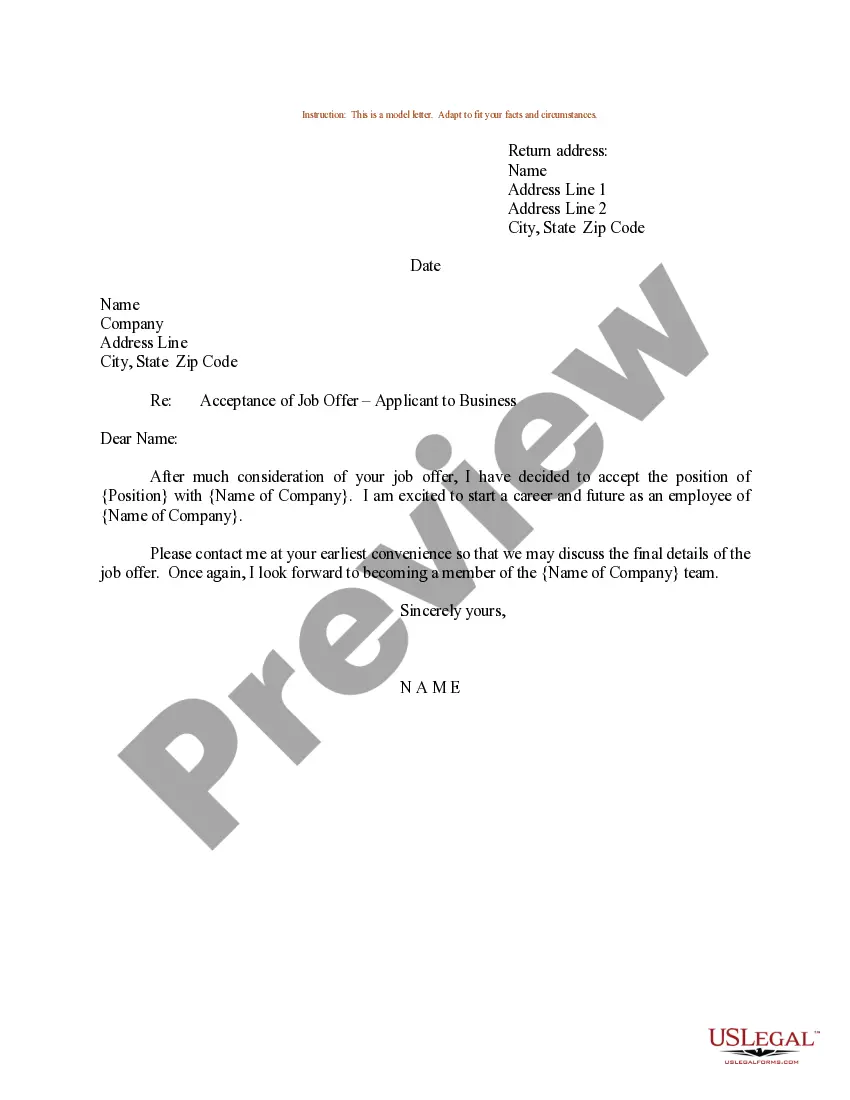
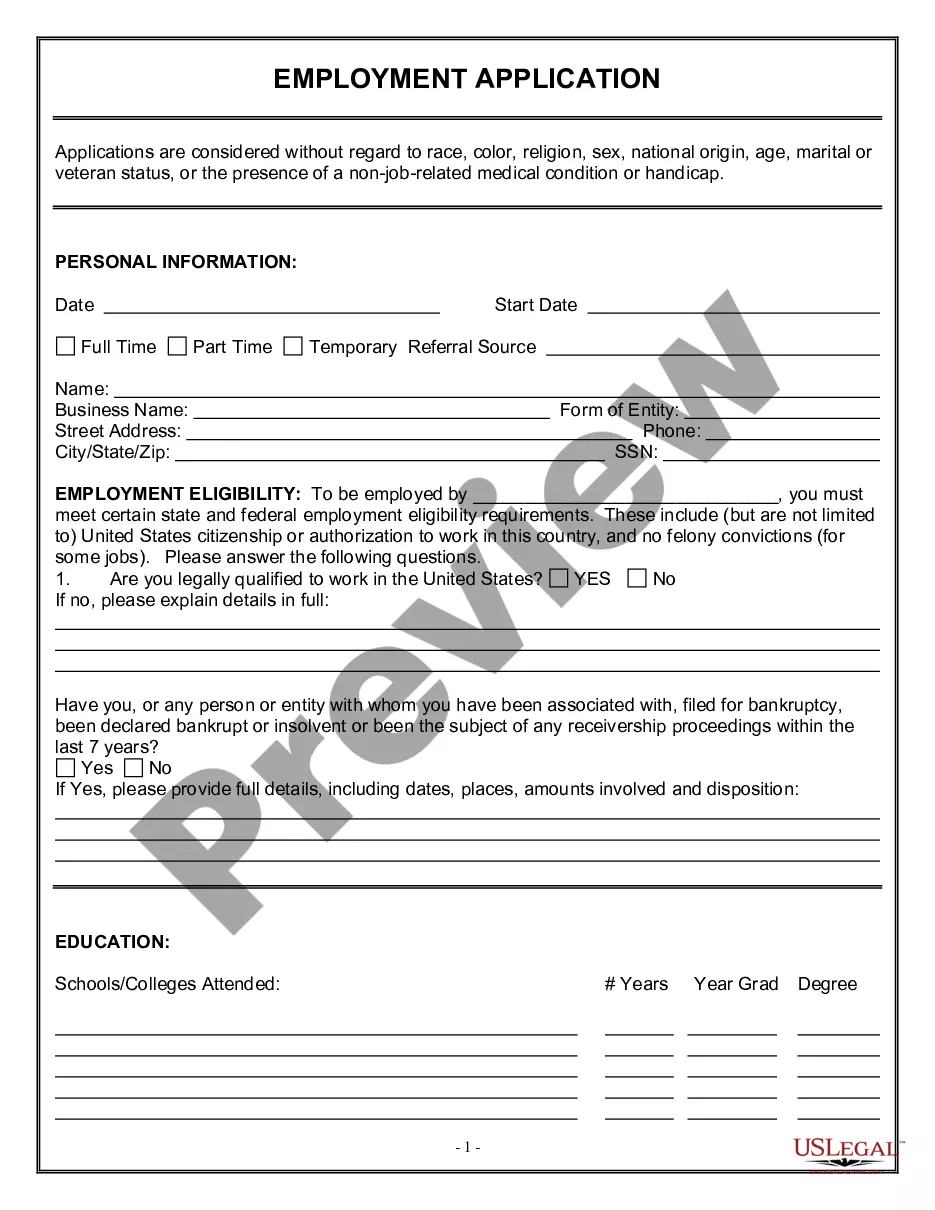
- Very first, make certain you have chosen the proper type for the area/region. You are able to check out the form using the Preview switch and look at the form outline to make sure this is basically the best for you.
- In the event the type does not fulfill your expectations, utilize the Seach discipline to find the appropriate type.
- When you are sure that the form is suitable, go through the Acquire now switch to have the type.
- Choose the pricing program you need and enter in the necessary info. Build your profile and pay for an order using your PayPal profile or credit card.
- Select the submit structure and download the legitimate document web template to your device.
- Total, modify and printing and signal the obtained Maine COBRA Continuation Coverage Election Notice.
US Legal Forms is definitely the largest catalogue of legitimate varieties where you can discover a variety of document layouts. Take advantage of the service to download skillfully-made documents that adhere to state demands.
Form popularity
FAQ
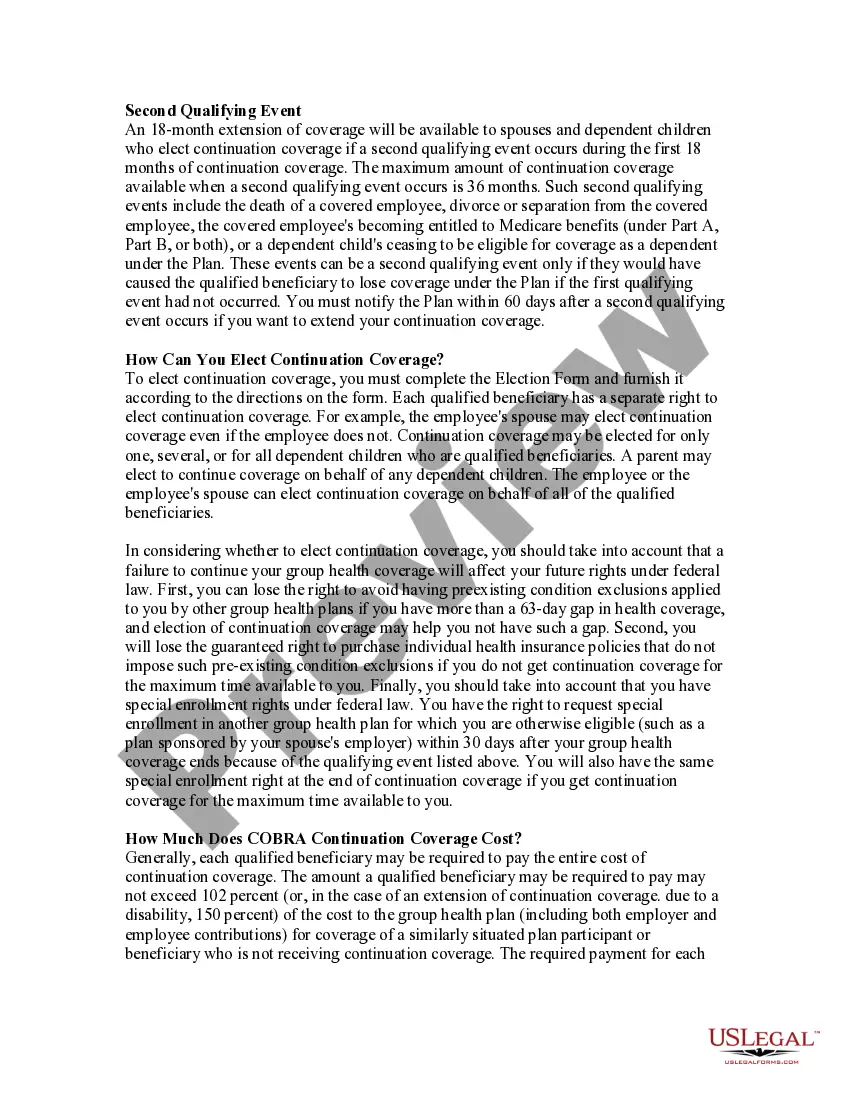
You may be able to keep your job-based health plan through COBRA continuation coverage. COBRA is a federal law that may let you pay to stay on your employee health insurance for a limited time after your job ends (usually 18 months). You pay the full premium yourself, plus a small administrative fee.
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
COBRA stands for Consolidated Omnibus Budget Reconciliation Act. Basically, it means that some families can keep their workplace coverage even after the family member is no longer at that workplace or if a divorce has occured.
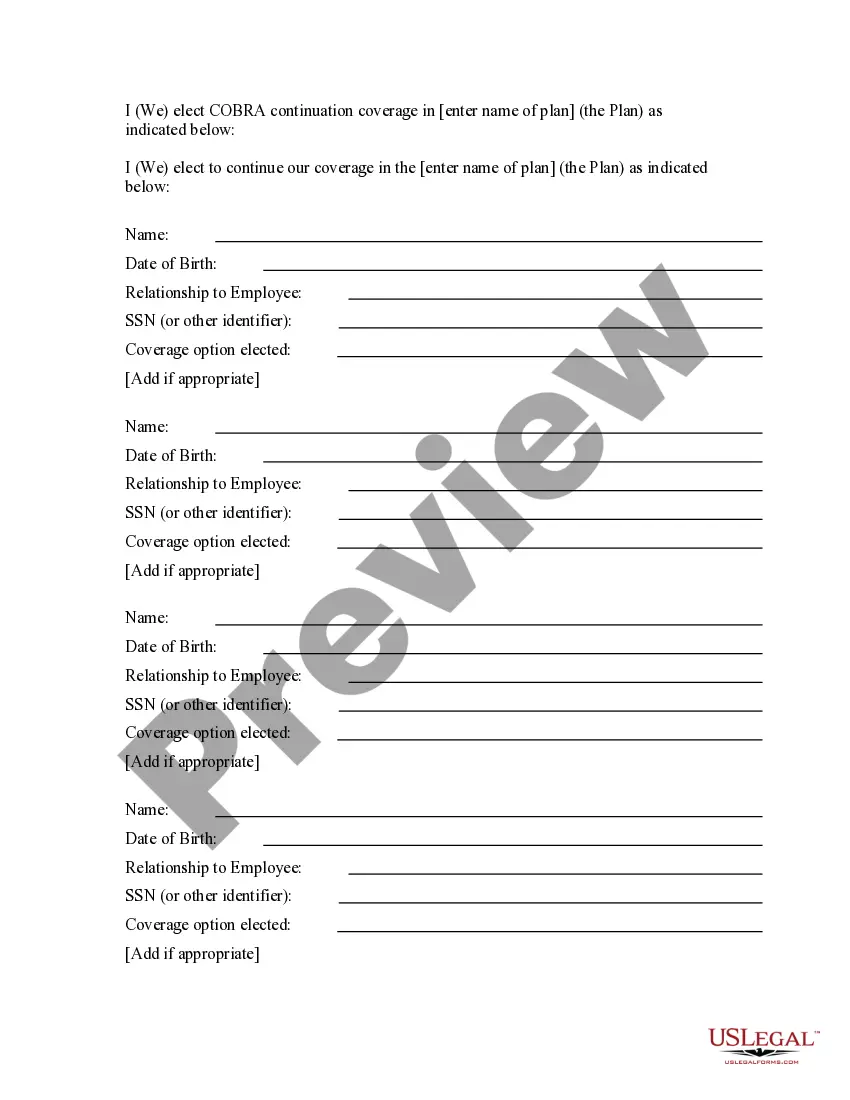
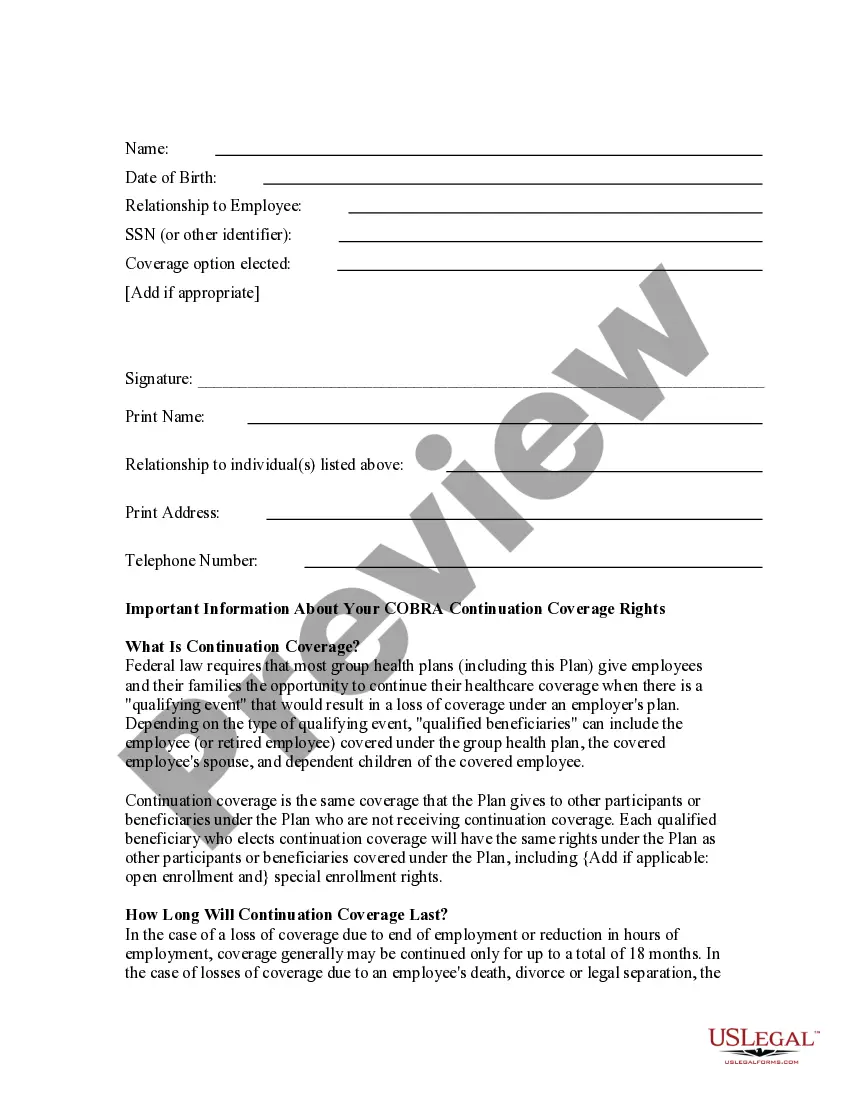
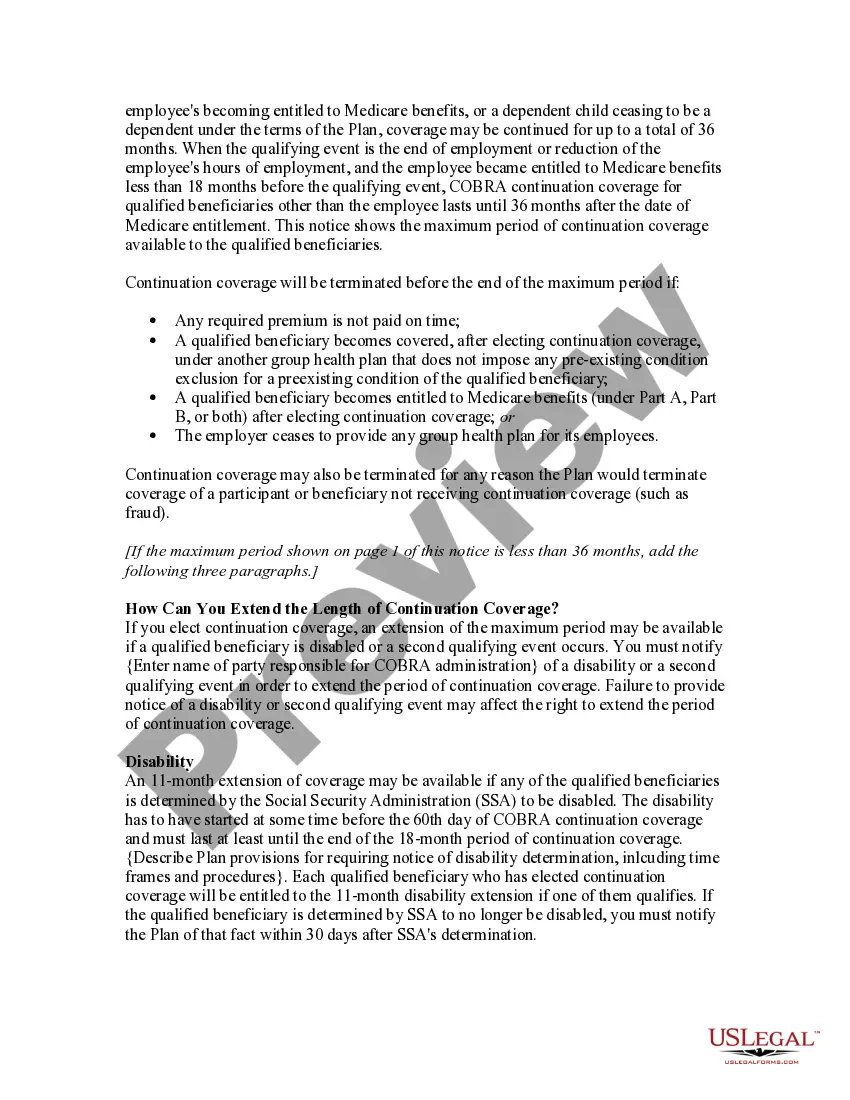
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.