Michigan Summary of Rights and Obligations under COBRA is a comprehensive document that outlines the rights and obligations of employees and their dependents regarding continuation of health coverage after a qualifying event. COBRA, or the Consolidated Omnibus Budget Reconciliation Act, is a federal law that applies to employers with 20 or more employees, including those in the state of Michigan. The Michigan Summary of Rights and Obligations under COBRA provides important information about the continuation coverage options available to individuals who would otherwise lose their health benefits due to certain circumstances such as job loss, reduction in working hours, or the death of an employee. The document explains the eligibility criteria for individuals to qualify for COBRA coverage, the duration of the coverage, and the premiums individuals may be required to pay to maintain this coverage. It also highlights the types of events that would make employees and their dependents eligible for COBRA, such as termination of employment, retirement, or divorce. In addition, the Michigan Summary of Rights and Obligations under COBRA clarifies the notification requirements for employers to inform individuals of their rights and provides guidance on the required timeline for such notifications. It emphasizes the importance of timely communication to ensure that eligible individuals are aware of the available options and can make informed decisions regarding their healthcare coverage. Furthermore, the document addresses the rights and obligations of both the employer and the qualified beneficiaries under COBRA. It covers topics such as the temporary extension of coverage, the right to choose alternative coverage, the responsibilities of making premium payments, and the consequences of failing to meet these obligations. It is crucial for both employers and employees to understand the Michigan Summary of Rights and Obligations under COBRA to ensure compliance with the law and to safeguard the healthcare coverage of eligible individuals and their dependents. Failure to comply with COBRA regulations can lead to legal and financial consequences for employers, while employees may risk losing access to healthcare services in critical times. Different types of Michigan Summary of Rights and Obligations under COBRA may include: 1. Regular COBRA: This type refers to the standard continuation coverage provided to eligible individuals who experience a qualifying event. 2. Extended COBRA: This category encompasses situations where additional coverage beyond the standard COBRA period may be applicable, typically due to disability or other specific circumstances. 3. Mini-COBRA: While not specific to Michigan, Mini-COBRA refers to state-specific continuation coverage laws that apply to employers with fewer than 20 employees. Michigan has its own Mini-COBRA law, providing similar coverage options for qualifying individuals employed by smaller businesses. By understanding and complying with the Michigan Summary of Rights and Obligations under COBRA, both employers and employees can ensure the smooth and appropriate continuation of health coverage during challenging times.
Michigan Summary of Rights and Obligations under COBRA
Description
How to fill out Michigan Summary Of Rights And Obligations Under COBRA?
US Legal Forms - one of several most significant libraries of lawful types in the States - offers a variety of lawful document themes you can acquire or print. While using internet site, you may get a huge number of types for organization and specific functions, sorted by groups, states, or keywords.You will find the latest models of types just like the Michigan Summary of Rights and Obligations under COBRA in seconds.
If you currently have a membership, log in and acquire Michigan Summary of Rights and Obligations under COBRA from the US Legal Forms catalogue. The Obtain button can look on each kind you view. You gain access to all in the past saved types within the My Forms tab of the account.
If you would like use US Legal Forms the very first time, listed here are straightforward guidelines to help you began:
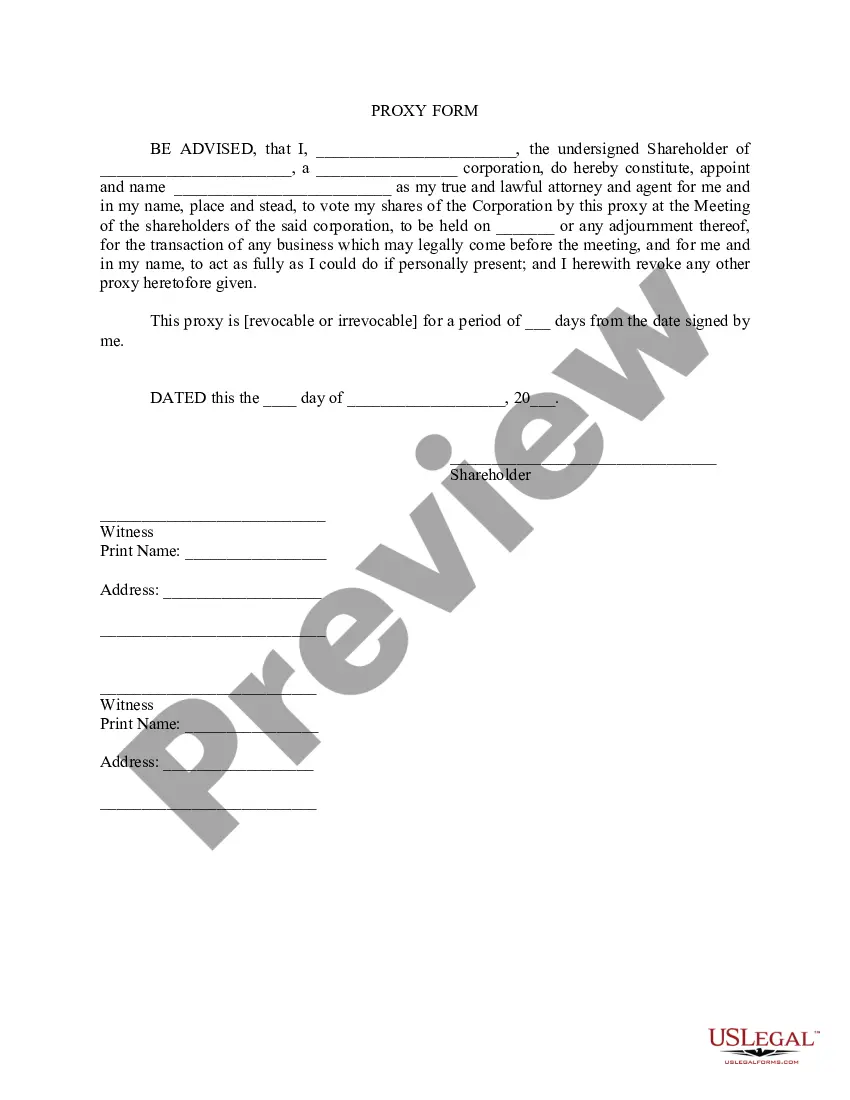
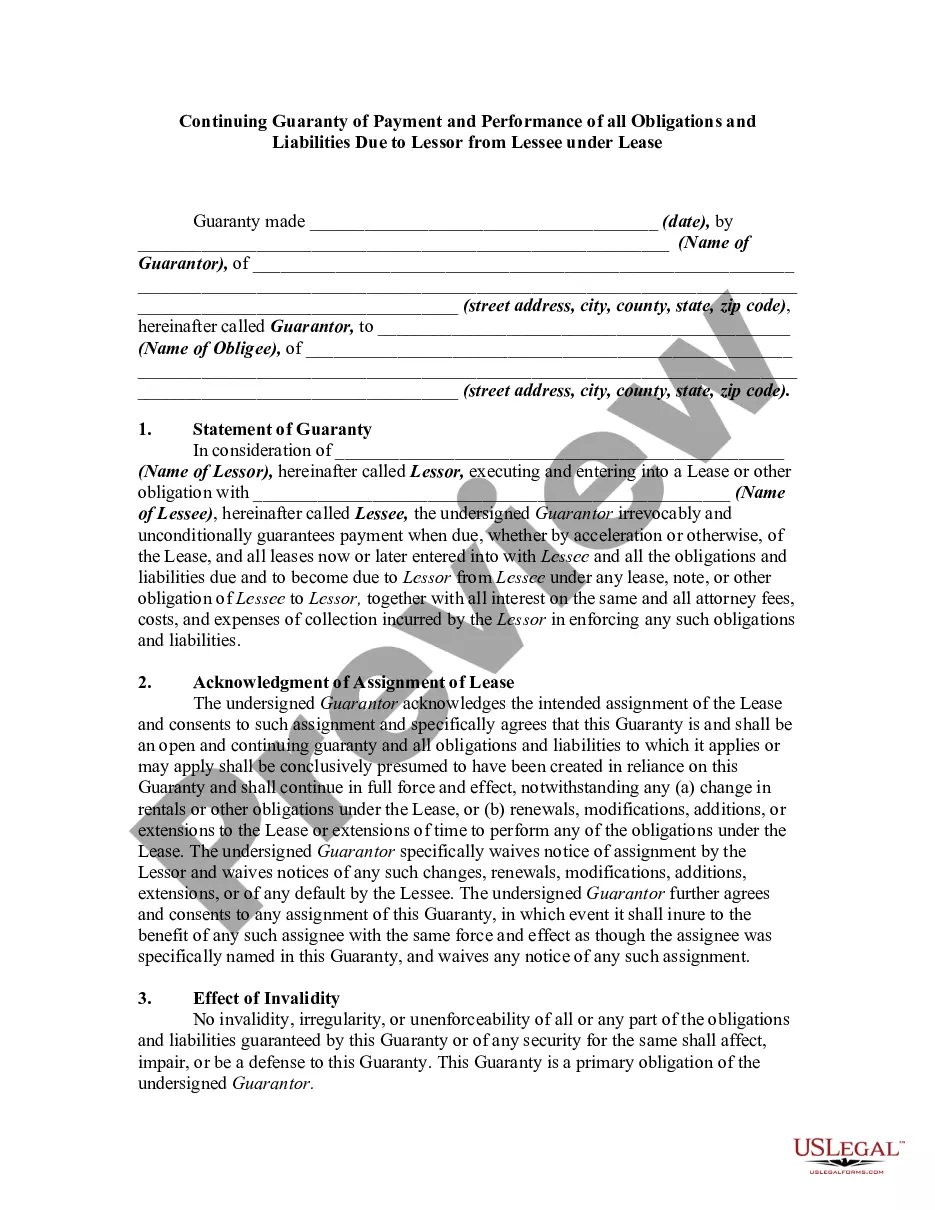
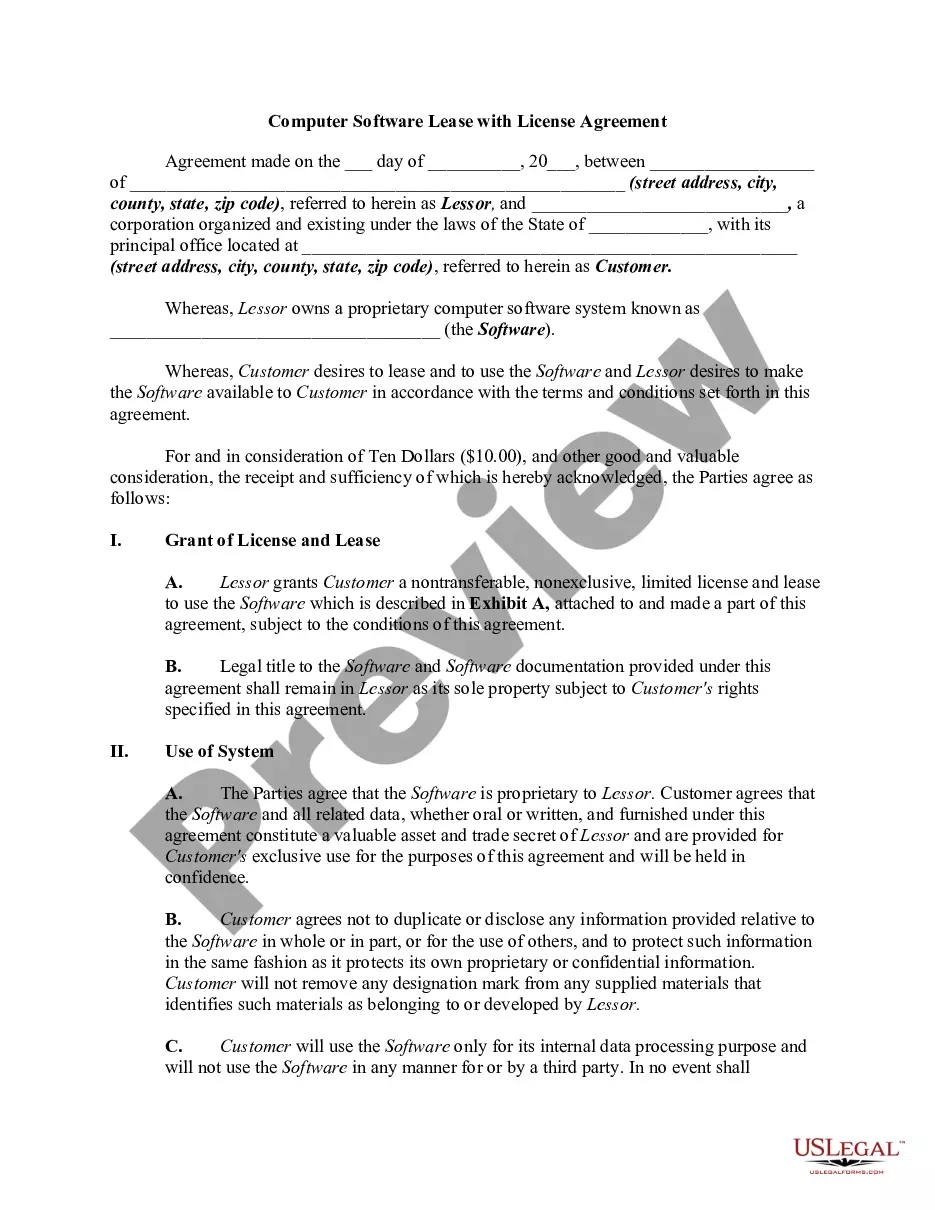
- Be sure you have picked out the right kind for your metropolis/region. Click on the Preview button to review the form`s content material. See the kind information to actually have selected the right kind.
- If the kind does not match your requirements, take advantage of the Lookup area near the top of the display screen to find the one that does.
- In case you are satisfied with the shape, confirm your choice by simply clicking the Acquire now button. Then, select the prices plan you favor and provide your accreditations to register for an account.
- Process the purchase. Use your charge card or PayPal account to complete the purchase.
- Pick the format and acquire the shape on your system.
- Make modifications. Load, change and print and sign the saved Michigan Summary of Rights and Obligations under COBRA.
Every web template you included in your bank account lacks an expiration date and is also the one you have forever. So, if you want to acquire or print another duplicate, just check out the My Forms portion and then click in the kind you will need.
Get access to the Michigan Summary of Rights and Obligations under COBRA with US Legal Forms, one of the most comprehensive catalogue of lawful document themes. Use a huge number of professional and state-specific themes that meet up with your business or specific needs and requirements.
Form popularity
FAQ
COBRA, known in full as the Consolidated Omnibus Budget Reconciliation Act, allows qualified workers to continue employer-sponsored health care coverage most commonly for 18 months after they leave their job.
The federal COBRA law requires Michigan companies who employee 20 or more workers to offer a continuation of their group health plan benefits if that insurance would end due to voluntarily quitting your job, getting fired or laid off, retire before eligible for Medicare and if there are changes in the immediate family.
How long does it take for COBRA to kick in? With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive.
Who pays for COBRA coverage? The employee generally pays the full cost of the insurance premiums. In fact, the law allows the employer to charge 102 percent of the premium, and to keep the 2 percent to cover your administrative costs.
As an employer, you are responsible for notifying your former employee of the right to elect COBRA continuing health care coverage under your group plan. Most employers will include COBRA coverage information in the business employee handbook and as part of an employee's exit paperwork.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.