Michigan Notice of Special Enrollment Rules
Description
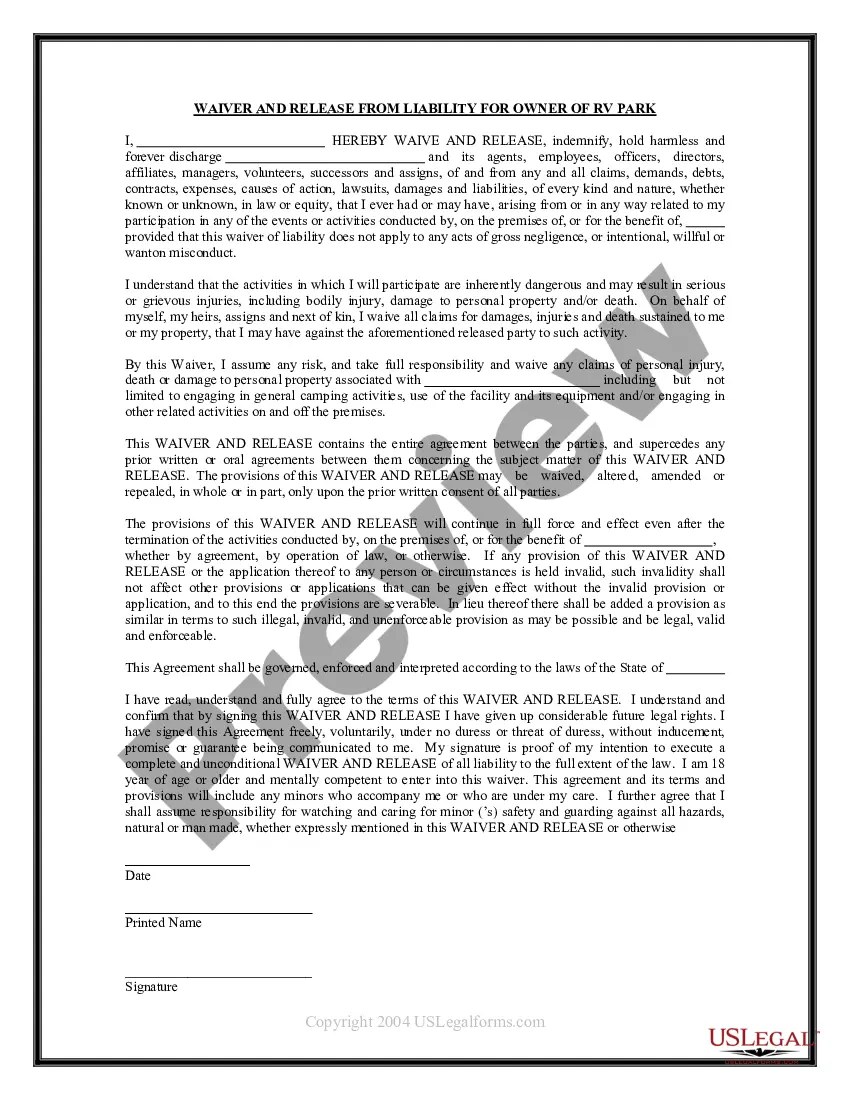
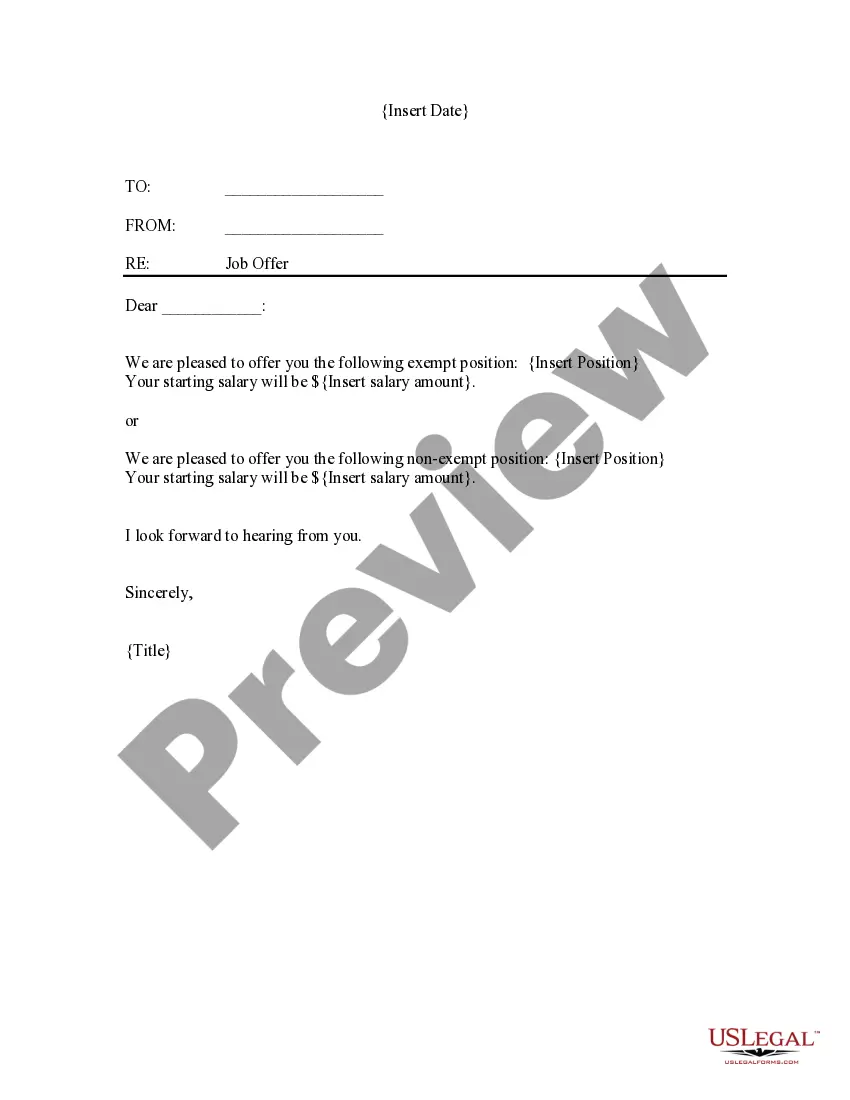
How to fill out Notice Of Special Enrollment Rules?
US Legal Forms - one of many largest libraries of legitimate kinds in the States - delivers a wide array of legitimate file web templates it is possible to acquire or printing. Utilizing the website, you can find a large number of kinds for business and personal functions, categorized by groups, suggests, or key phrases.You can find the most recent versions of kinds just like the Michigan Notice of Special Enrollment Rules in seconds.
If you already possess a subscription, log in and acquire Michigan Notice of Special Enrollment Rules from your US Legal Forms local library. The Acquire button can look on every single form you view. You have access to all formerly delivered electronically kinds within the My Forms tab of your bank account.
In order to use US Legal Forms for the first time, allow me to share easy recommendations to get you started:
- Be sure you have chosen the right form for the area/state. Go through the Review button to analyze the form`s content. Look at the form information to actually have selected the proper form.
- In the event the form does not suit your specifications, use the Search field at the top of the display to discover the one that does.
- In case you are happy with the form, verify your selection by clicking on the Acquire now button. Then, select the pricing program you want and offer your accreditations to sign up for an bank account.
- Procedure the deal. Make use of charge card or PayPal bank account to accomplish the deal.
- Select the structure and acquire the form on your own product.
- Make adjustments. Load, revise and printing and sign the delivered electronically Michigan Notice of Special Enrollment Rules.
Every format you included in your bank account lacks an expiry day and it is yours eternally. So, if you would like acquire or printing one more copy, just go to the My Forms section and then click around the form you will need.
Get access to the Michigan Notice of Special Enrollment Rules with US Legal Forms, probably the most extensive local library of legitimate file web templates. Use a large number of skilled and state-particular web templates that meet your organization or personal requires and specifications.
Form popularity
FAQ
In the case of a qualified individual or enrollee who is eligible for a special enrollment period as described in paragraphs (d)(4), (5), or (9) of this section, the Exchange may define the length of the special enrollment period as appropriate based on the circumstances of the special enrollment period, but in no
Why do we have an open enrollment period? The open enrollment period was put into place to discourage adverse selection which happens when sick people sign up for health insurance and healthy people don't. It greatly skews the amount of financial risk a health plan takes when insuring customers.
You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
If you get married, you're eligible to get coverage effective the first of the following month, regardless of how late in the month you enroll. If you have a baby, adopt a child, or receive a court order for medical child support, the coverage can be backdated to the date of the birth, adoption, or court order.
Normally, coverage is only available for purchase during the annual open enrollment period, but a special enrollment period allows people to sign up for coverage outside of that annual window, as long as they have a qualifying event.
A change in your situation like getting married, having a baby, or losing health coverage that can make you eligible for a Special Enrollment Period, allowing you to enroll in health insurance outside the yearly Open Enrollment Period.
You qualify for a Special Enrollment Period if you've had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.
Period of enrollment means the period that the title IV institution has established for which institutional charges are generally assessed (i.e., length of the student's course, program, or academic year.)