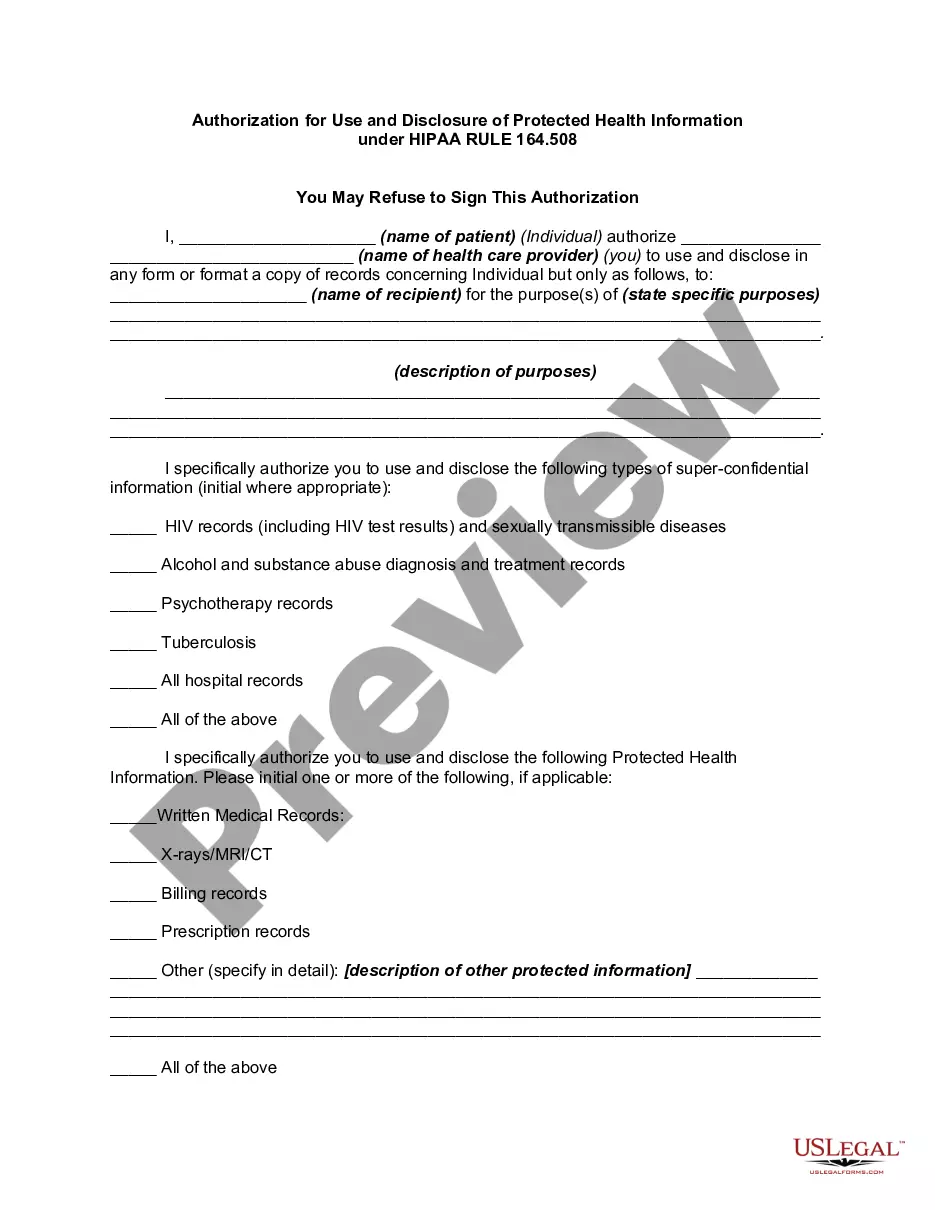
Under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the Privacy Regulations written pursuant to the Act, the general rule is that covered entities may not use or disclose an individual's protected health information for purposes unrelated to treatment, payment, healthcare operations, or certain defined exceptions without first obtaining the individual's prior written authorization.
The Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 is a legal document that grants permission for the release and sharing of an individual's protected health information (PHI) in accordance with the Health Insurance Portability and Accountability Act (HIPAA). This authorization is essential for healthcare providers, insurance companies, and other covered entities to ensure compliance with privacy regulations and maintain confidentiality while facilitating the exchange of necessary information. Abiding by HIPAA RULE 164.508, the Minnesota Authorization for Use and Disclosure outlines specific circumstances under which PHI can be accessed, used, or disclosed. It provides a comprehensive framework for individuals to give informed consent regarding the release of their sensitive health data. The authorization includes specifics about the purpose, scope, and duration of the permitted information sharing. Some relevant keywords associated with the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 are: 1. Protected Health Information (PHI): Refers to individually identifiable health information related to an individual's health status, healthcare provision, or payment for healthcare that is protected under HIPAA. 2. Authorization: Legal consent obtained from an individual to disclose their PHI for specific purposes, given voluntarily and with understanding of the consequences. 3. Use: The utilization of PHI within a covered entity or organization for purposes such as treatment, payment, or healthcare operations. 4. Disclosure: The sharing or release of PHI to outside entities or individuals, including healthcare providers, insurance companies, researchers, or legal authorities. 5. Health Insurance Portability and Accountability Act (HIPAA): Federal legislation enacted to safeguard sensitive healthcare information and establish standards for the electronic exchange, privacy, and security of PHI. Different types of Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 may include: 1. General Authorization for Use and Disclosure: This is the standard form used for most routine healthcare situations where the individual is giving broad consent for the use and disclosure of their PHI. 2. Specific Authorization for Use and Disclosure: In cases where more specific or sensitive information needs to be shared, a specialized authorization form may be used. This can involve sharing mental health records, substance abuse treatment information, or HIV/AIDS-related data, which require additional confidentiality measures. 3. Research Authorization: When conducting medical research, a separate research authorization may be necessary, providing consent for the use and disclosure of PHI for research purposes while maintaining individual privacy. It is important for individuals to carefully review the content of any Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 before signing, ensuring they understand the extent of information being shared and the purpose for which it will be used or disclosed. This authorization serves as a vital tool to protect patient privacy and maintain the integrity of healthcare information exchange.