Minnesota Affidavit of No Coverage by Another Group Health Plan
Description
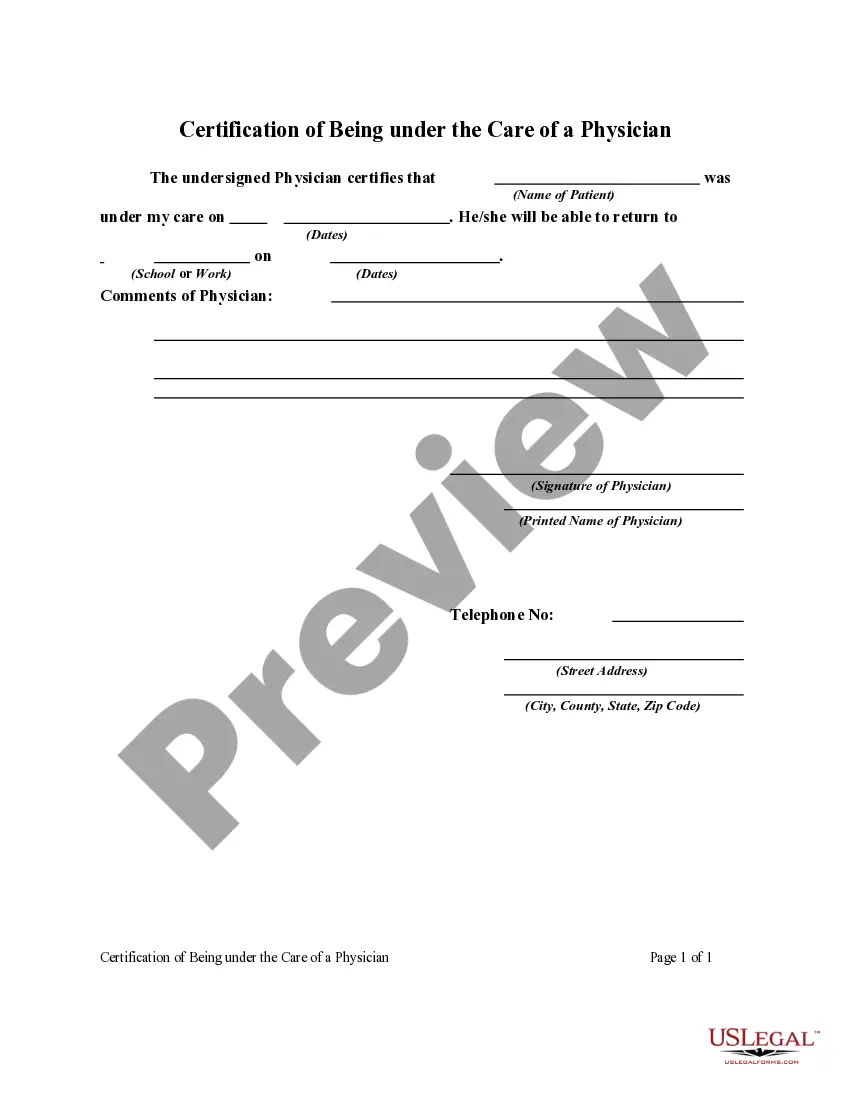
How to fill out Affidavit Of No Coverage By Another Group Health Plan?
US Legal Forms - one of the largest collections of legal documents in the United States - offers a variety of legal document templates that you can purchase or print. While using the website, you will find a vast array of forms for business and personal use, sorted by categories, states, or keywords.
You can access the latest versions of forms such as the Minnesota Affidavit of No Coverage by Another Group Health Plan within seconds. If you already hold a monthly subscription, Log In and obtain the Minnesota Affidavit of No Coverage by Another Group Health Plan from the US Legal Forms library. The Download button will appear on every form you view. You can access all previously saved forms in the My documents tab of your account.
If you wish to use US Legal Forms for the first time, here are simple steps to help you begin: Make sure you have selected the correct form for your city/state. Click the Review button to examine the content of the form. Read the form description to ensure you have selected the right one. If the form does not meet your needs, utilize the Search field at the top of the screen to find one that does.
Gain access to the Minnesota Affidavit of No Coverage by Another Group Health Plan through US Legal Forms, the most comprehensive library of legal document templates. Utilize a vast selection of professional and state-specific templates that fulfill your business or personal requirements and needs.
- If you are satisfied with the form, confirm your choice by clicking the Purchase now button.
- Then, select the pricing plan you prefer and provide your information to register for an account.
- Process the transaction. Use your credit card or PayPal account to complete the purchase.
- Choose the format and download the form to your device.
- Make modifications. Complete, edit, and print and sign the saved Minnesota Affidavit of No Coverage by Another Group Health Plan.
- Each template you added to your account does not have an expiration date and is yours forever. So, if you need to acquire or print another copy, simply head to the My documents section and click on the form you need.
Form popularity
FAQ
If you have multiple health insurance policies, you'll have to pay any applicable premiums and deductibles for both plans. Your secondary insurance won't pay toward your primary's deductible. You may also owe other cost sharing or out-of-pocket costs, such as copayments or coinsurance.
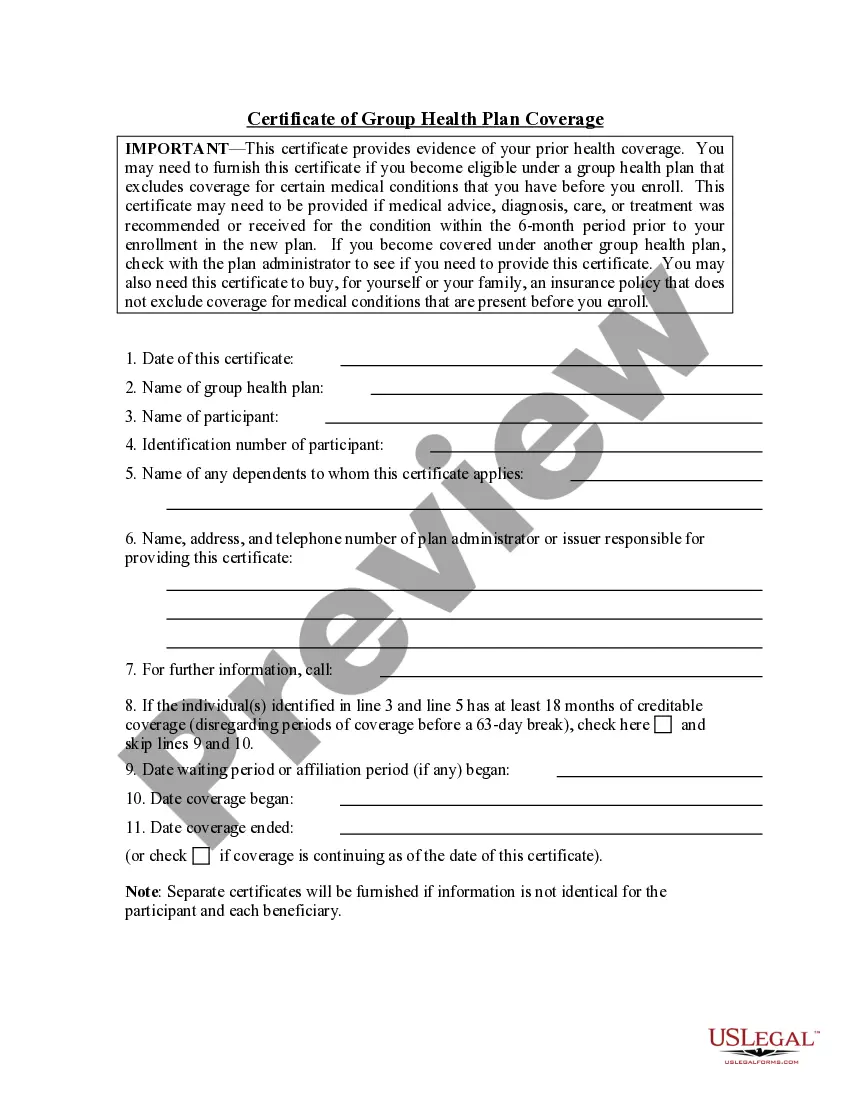
The primary purpose of the certificate is to show the amount of creditable coverage that you had under a group health plan or other health insurance coverage, because this can reduce or eliminate the length of time that any pre-existing condition clause in a new plan otherwise might apply to you.
A contributory pension plan requires the employees to pay into the plan from their salary (the employees' pay stub would show the money was taken out of their pay to go into the pension plan). In a non-contributory pension plan only the employer contributes.
This document explains the health benefits you and your dependents have under the plan. It details the services that will and will not be covered. Services that are not covered are called exclusions.
Continuation coverage allows someone who recently lost their employer-based health coverage to continue their current insurance policy as long as they pay the full monthly premiums.
Who is issued a certificate of insurance with a group insurance policy? The participant is issued a certificate of insurance with a group insurance policy.
Noncontributory - Group life insurance plans are those in which the employer pays the entire premium and the employee supplies no portion of the premium costs. Employers have the option of contributing to the employees' premium payments in part or in full.
Definition of noncontributory : making or involving no contribution: such as. a : involving, relating to, or being an employee benefit (such as a pension plan) which is entirely funded by the employer with no contribution from the employee a noncontributory pension noncontributory life insurance plans.
A certificate of Creditable Coverage (COCC) is a document provided by your previous insurance carrier that proves that your insurance has ended. This includes the name of the member to whom it applies as well as the coverage effective date and cancelation date.
If a Social Security agreement assigns coverage of the employee's work to the United States, the Social Security Administration issues a U.S. Certificate of Coverage. The certificate serves as proof that the employee and employer are exempt from the payment of Social Security taxes to the foreign country.