Title: Understanding the Minnesota Acknowledgment of Receipt of COBRA Notice: Types and Key Information Introduction: The Minnesota Acknowledgment of Receipt of COBRA Notice is a crucial document that ensures employees are well-informed about their rights and options regarding their health insurance coverage when leaving their job. This detailed description aims to provide an overview of the acknowledgment's purpose, its various types, and highlight relevant keywords for a comprehensive understanding. 1. The Purpose of Minnesota Acknowledgment of Receipt of COBRA Notice: This acknowledgment serves as proof that an employee has received essential information about their rights under the Consolidated Omnibus Budget Reconciliation Act (COBRA), specifically in the context of Minnesota state law. It confirms that the employee is aware of the continuation coverage options available to them if they experience a qualifying event, such as termination, reduction in work hours, or other qualifying factors. 2. Key Elements of the Minnesota Acknowledgment of Receipt of COBRA Notice: The acknowledgment typically includes the following information: a. Employee Details: Full name, address, contact information, and employee identification number. b. Employer Details: Name, address, and contact information of the employer. c. Qualifying Event: Clearly specifying the qualifying event that triggers COBRA coverage. d. Notice provided by: Name of the entity responsible for providing the COBRA notice (often the employer or its designated administrator). e. Coverage Explanation: A comprehensive explanation of the available continuation coverage options, duration, and associated costs. f. Deadline and Process: Instructions for the employee to confirm receipt of the notice within the designated timeframe, usually through returning a signed copy. 3. Types of Minnesota Acknowledgment of Receipt of COBRA Notice: Although the acknowledgment largely follows a standardized format, it can have variations based on specific circumstances. Some notable types include: a. Minnesota Acknowledgment of Receipt of COBRA Notice — Termination: Used when an employee's termination triggers COBRA eligibility. b. Minnesota Acknowledgment of Receipt of COBRA Notice — Reduction in Work Hours: Applied when an employee experiences a significant reduction in work hours, leading to eligibility for COBRA. c. Minnesota Acknowledgment of Receipt of COBRA Notice — Qualifying Event: Covers diverse qualifying events (e.g., divorce, death of the covered employee) that may render dependents eligible. Conclusion: The Minnesota Acknowledgment of Receipt of COBRA Notice plays a vital role in ensuring employees are aware of their COBRA continuation coverage rights. Understanding the purpose, key elements, and different types of this notice is crucial for employees and employers to protect themselves during transitional healthcare periods. Compliance with the acknowledgment's requirements helps ensure a smooth and informed transition for employees seeking continued health insurance coverage.
Minnesota Acknowledgment of Receipt of COBRA Notice
Description
How to fill out Minnesota Acknowledgment Of Receipt Of COBRA Notice?
You can spend several hours on the web attempting to find the lawful document web template that fits the federal and state demands you will need. US Legal Forms supplies a large number of lawful kinds that are analyzed by professionals. You can actually down load or print out the Minnesota Acknowledgment of Receipt of COBRA Notice from our assistance.
If you have a US Legal Forms bank account, you can log in and then click the Acquire button. Afterward, you can total, modify, print out, or indicator the Minnesota Acknowledgment of Receipt of COBRA Notice. Each and every lawful document web template you purchase is yours for a long time. To have one more backup associated with a acquired form, visit the My Forms tab and then click the corresponding button.
If you use the US Legal Forms site initially, follow the basic directions under:
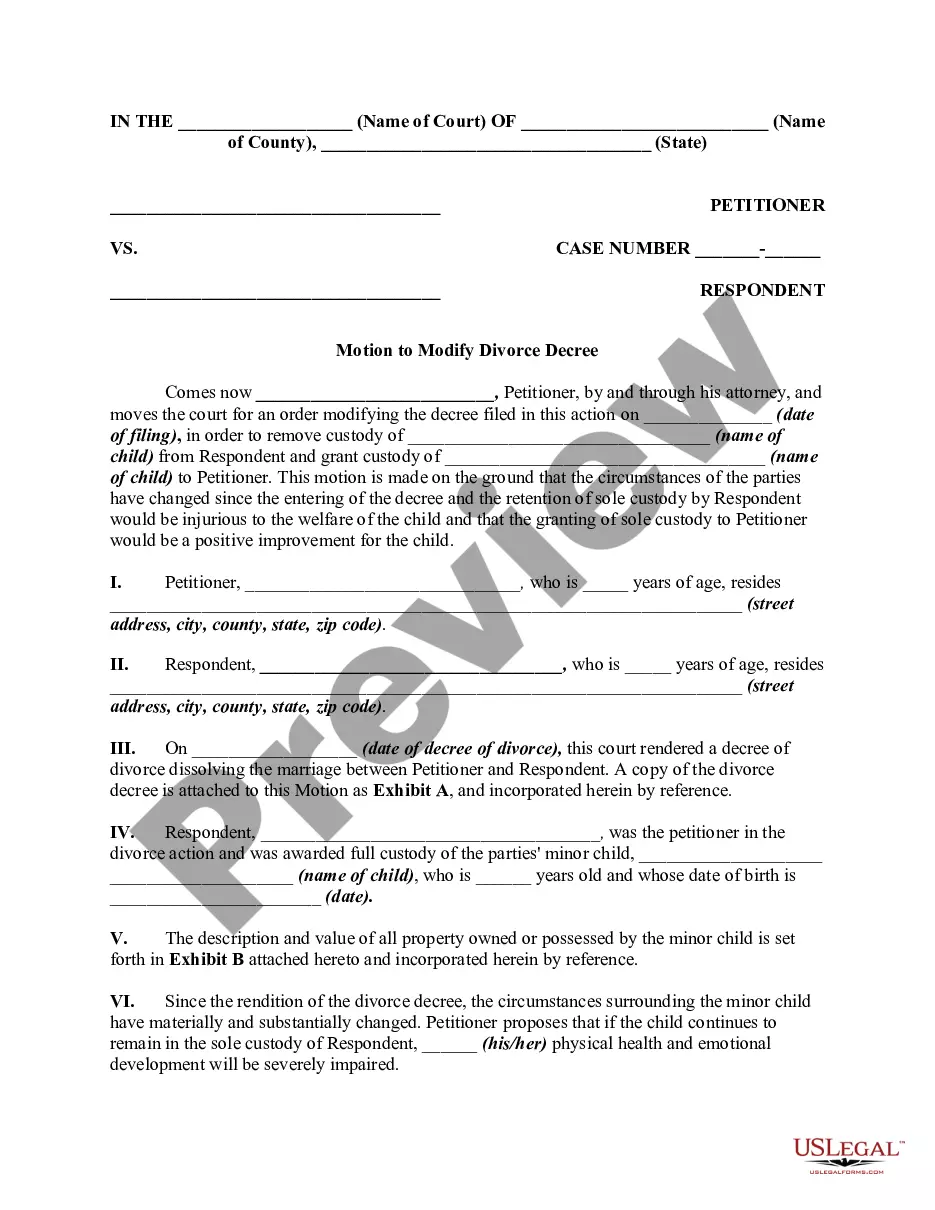
- Initially, make sure that you have selected the correct document web template to the county/area of your choice. Look at the form information to make sure you have picked out the right form. If accessible, take advantage of the Review button to search from the document web template at the same time.
- If you wish to find one more variation from the form, take advantage of the Research industry to find the web template that meets your requirements and demands.
- When you have located the web template you want, click Buy now to continue.
- Find the prices plan you want, enter your references, and sign up for a free account on US Legal Forms.
- Comprehensive the deal. You can utilize your charge card or PayPal bank account to purchase the lawful form.
- Find the structure from the document and down load it to the device.
- Make alterations to the document if required. You can total, modify and indicator and print out Minnesota Acknowledgment of Receipt of COBRA Notice.
Acquire and print out a large number of document web templates while using US Legal Forms site, that offers the most important assortment of lawful kinds. Use professional and status-specific web templates to handle your company or individual requirements.