Minnesota Individual Notice of Preexisting Condition Exclusion
Instant download
Description
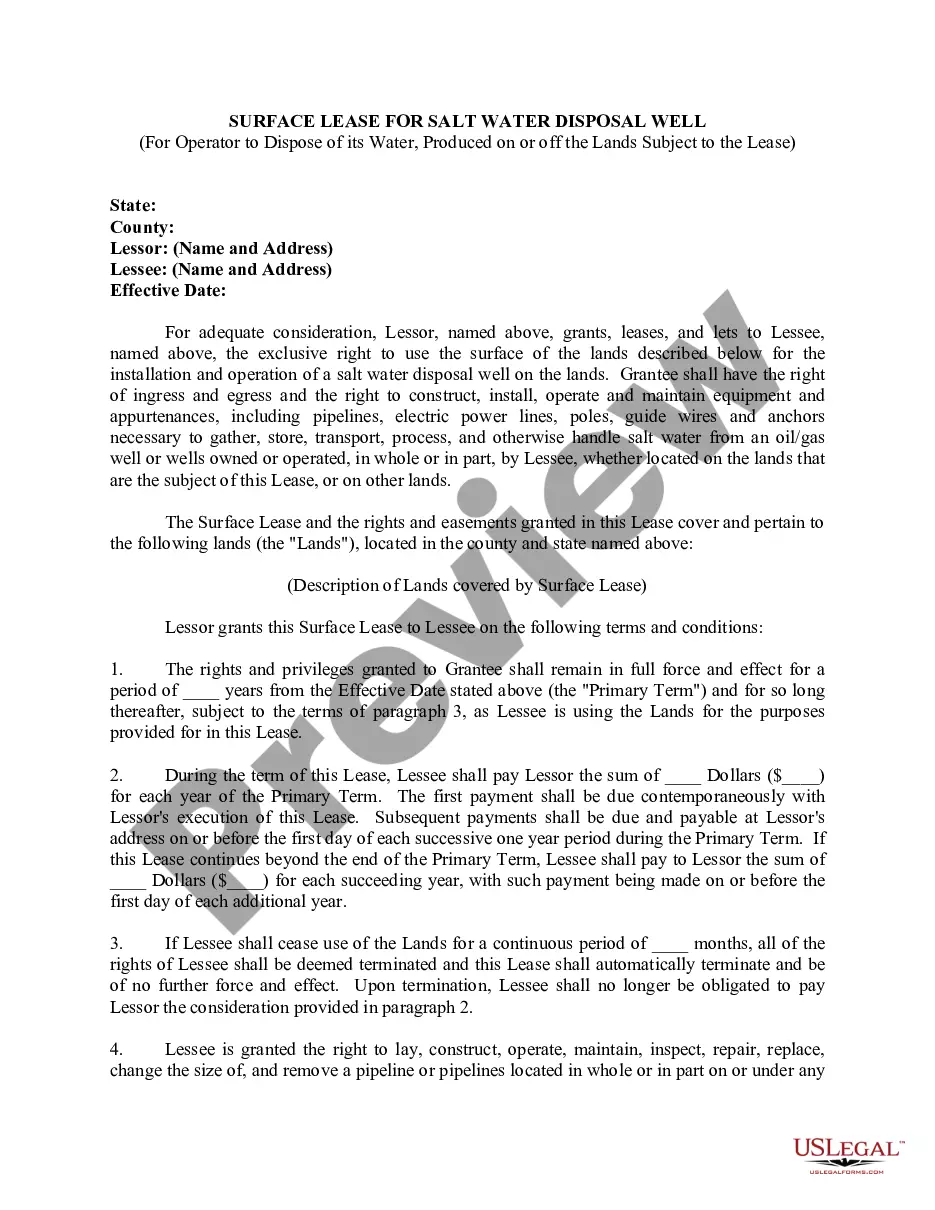
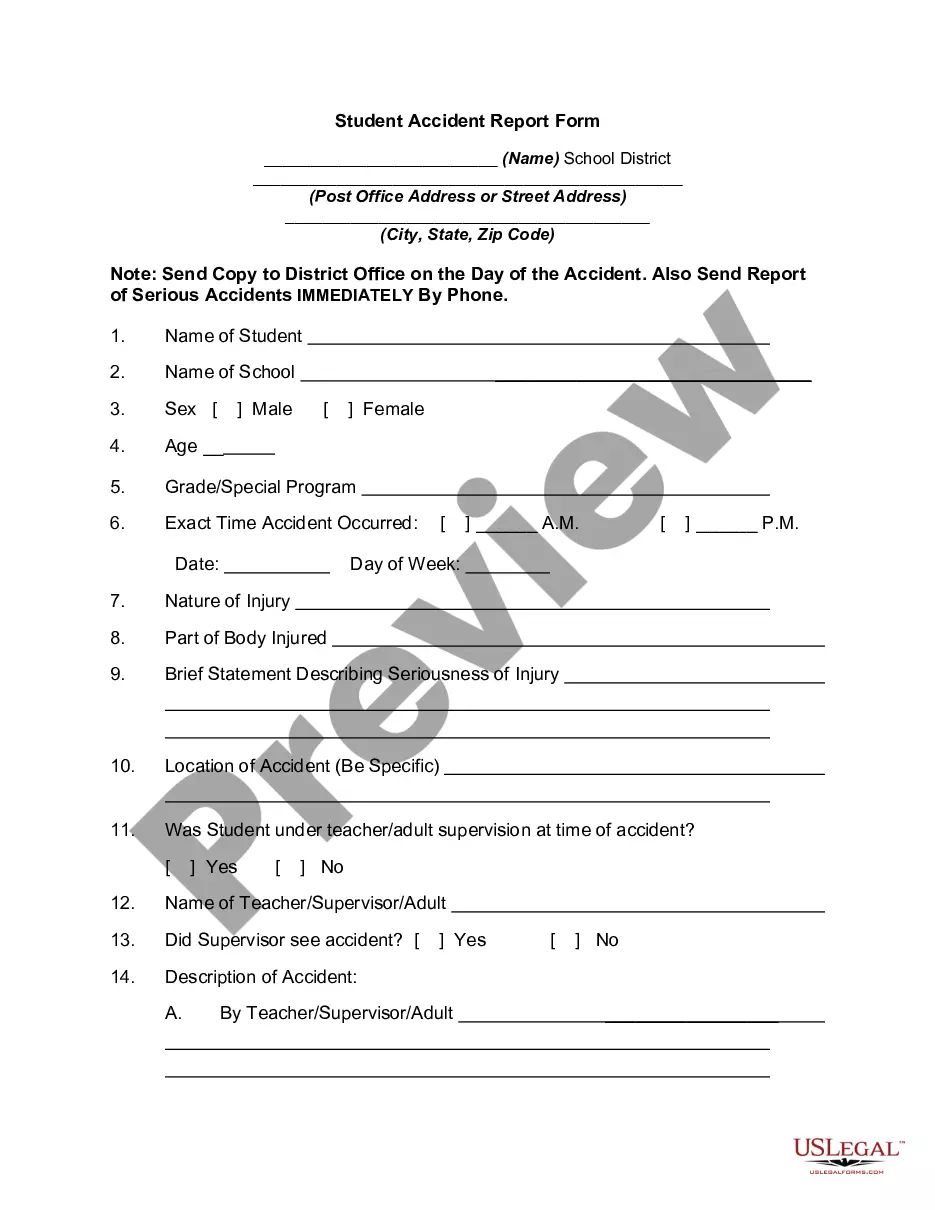
This AHI form is an individual notice regarding preexisting condition exclusions under the group health plan.
How to fill out Individual Notice Of Preexisting Condition Exclusion?
If you aim to be thorough, acquire, or print authentic document templates, make use of US Legal Forms, the largest assortment of legal documents accessible online.
Take advantage of the site's easy and user-friendly search function to find the documents you require.
Numerous templates for business and personal purposes are organized by categories and states, or by keywords.
Step 3. If you are not satisfied with the form, use the Search box at the top of the page to find other templates in the legal form layout.
Step 4. Once you’ve located the form you need, click the Get Now button. Choose the payment plan you prefer and enter your details to create an account.
- Utilize US Legal Forms to obtain the Minnesota Individual Notice of Preexisting Condition Exclusion in just a few clicks.
- If you are already a US Legal Forms user, Log In to your account and then click the Download button to obtain the Minnesota Individual Notice of Preexisting Condition Exclusion.
- You can also access forms you previously downloaded in the My documents section of your account.
- If this is your first time using US Legal Forms, follow the instructions below.
- Step 1. Ensure you have selected the form for the correct city/state.
- Step 2. Utilize the Preview option to review the content of the form. Don’t forget to read the description.