Missouri Authorization for Use and / or Disclosure of Protected Health Information
Description
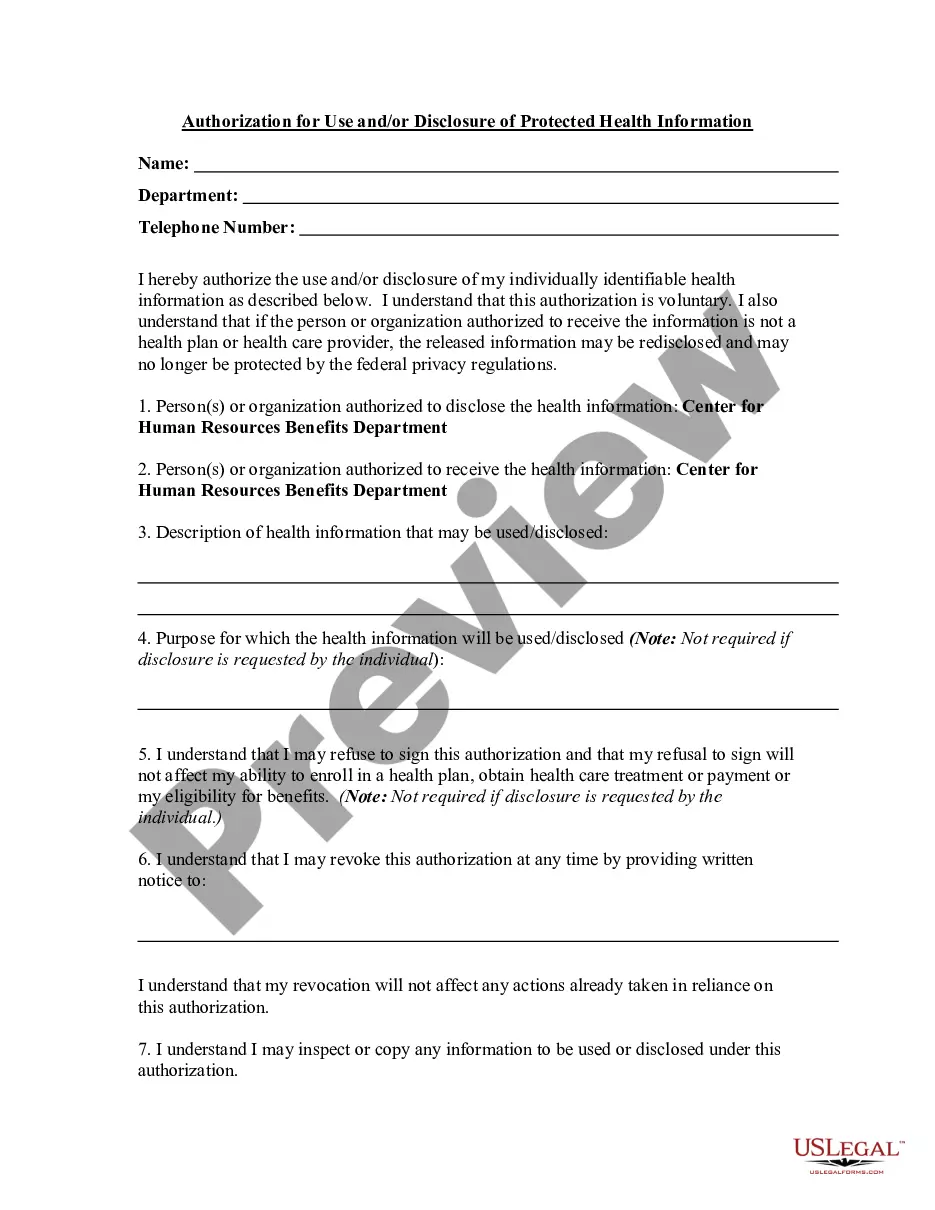
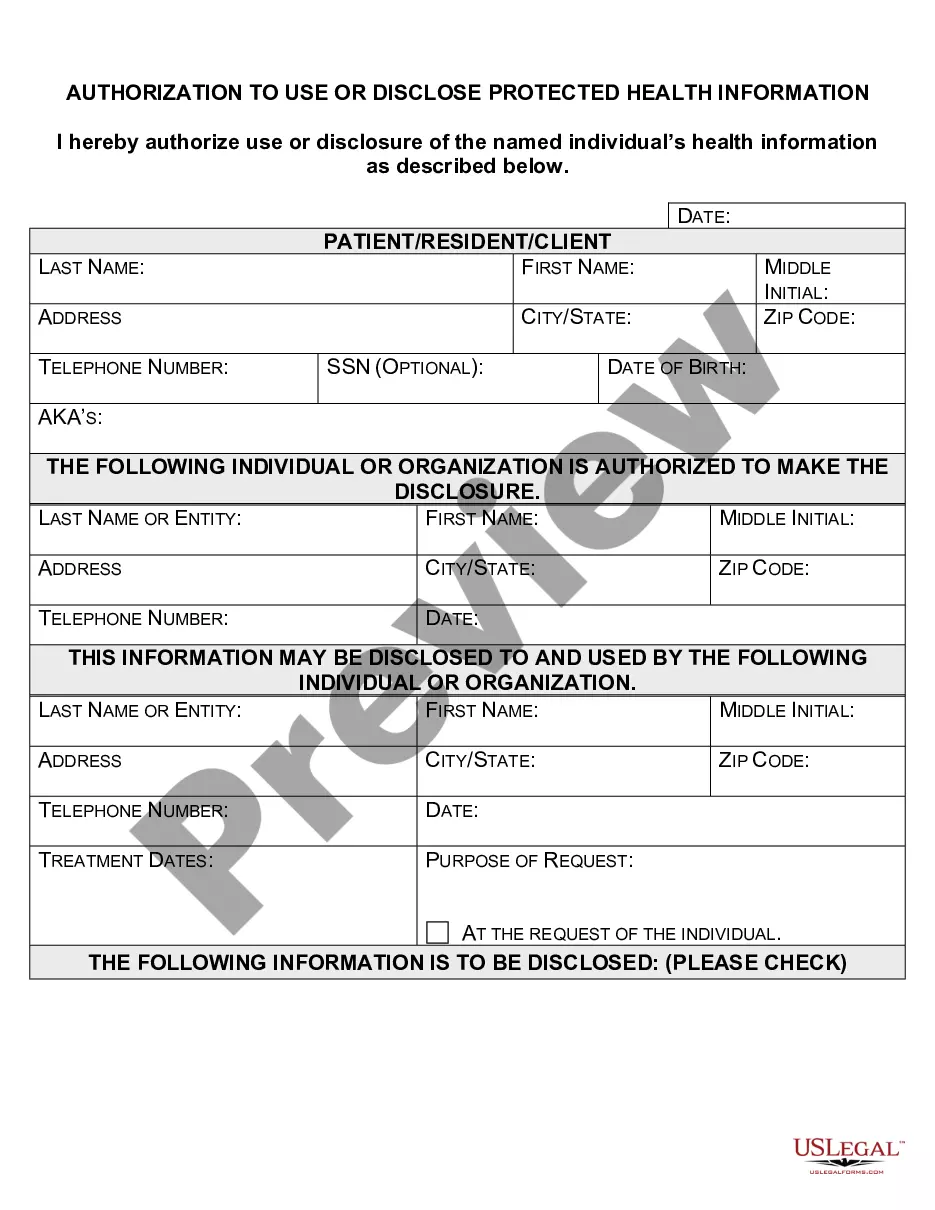
How to fill out Authorization For Use And / Or Disclosure Of Protected Health Information?
Are you presently in a circumstance that necessitates documentation for either organizational or personal purposes almost every day.
There are numerous legal document templates available online, but locating reliable versions can be challenging.
US Legal Forms provides thousands of form templates, such as the Missouri Authorization for Use and/or Disclosure of Protected Health Information, designed to comply with federal and state regulations.
You can obtain another copy of the Missouri Authorization for Use and/or Disclosure of Protected Health Information at any time if needed. Simply select the required document to download or print the form.
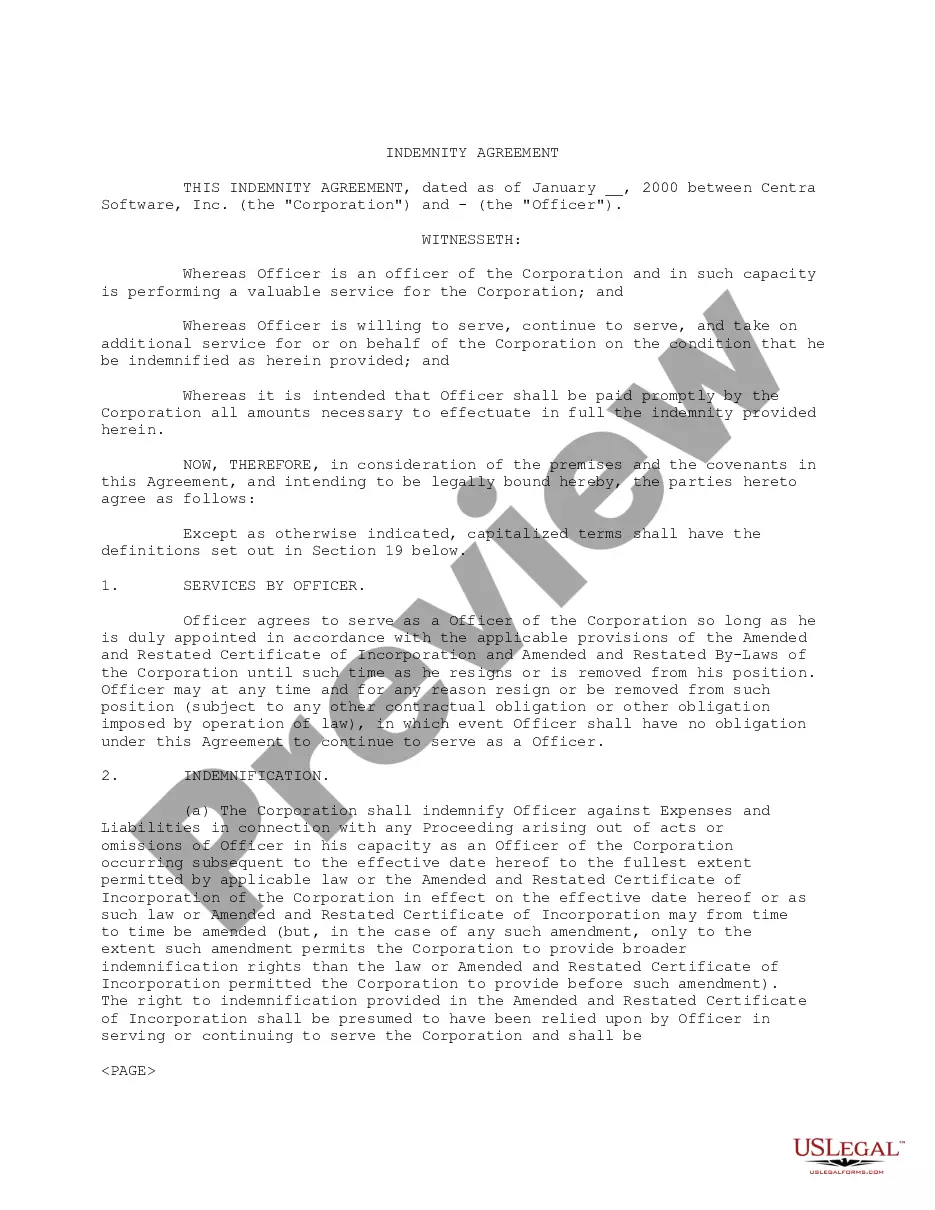
Use US Legal Forms, one of the largest collections of legal documents, to save time and avoid errors. The service offers properly crafted legal document templates that you can use for various purposes. Create an account on US Legal Forms and start simplifying your life.
- If you are familiar with the US Legal Forms website and possess an account, simply Log In.
- Afterward, you can download the Missouri Authorization for Use and/or Disclosure of Protected Health Information template.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
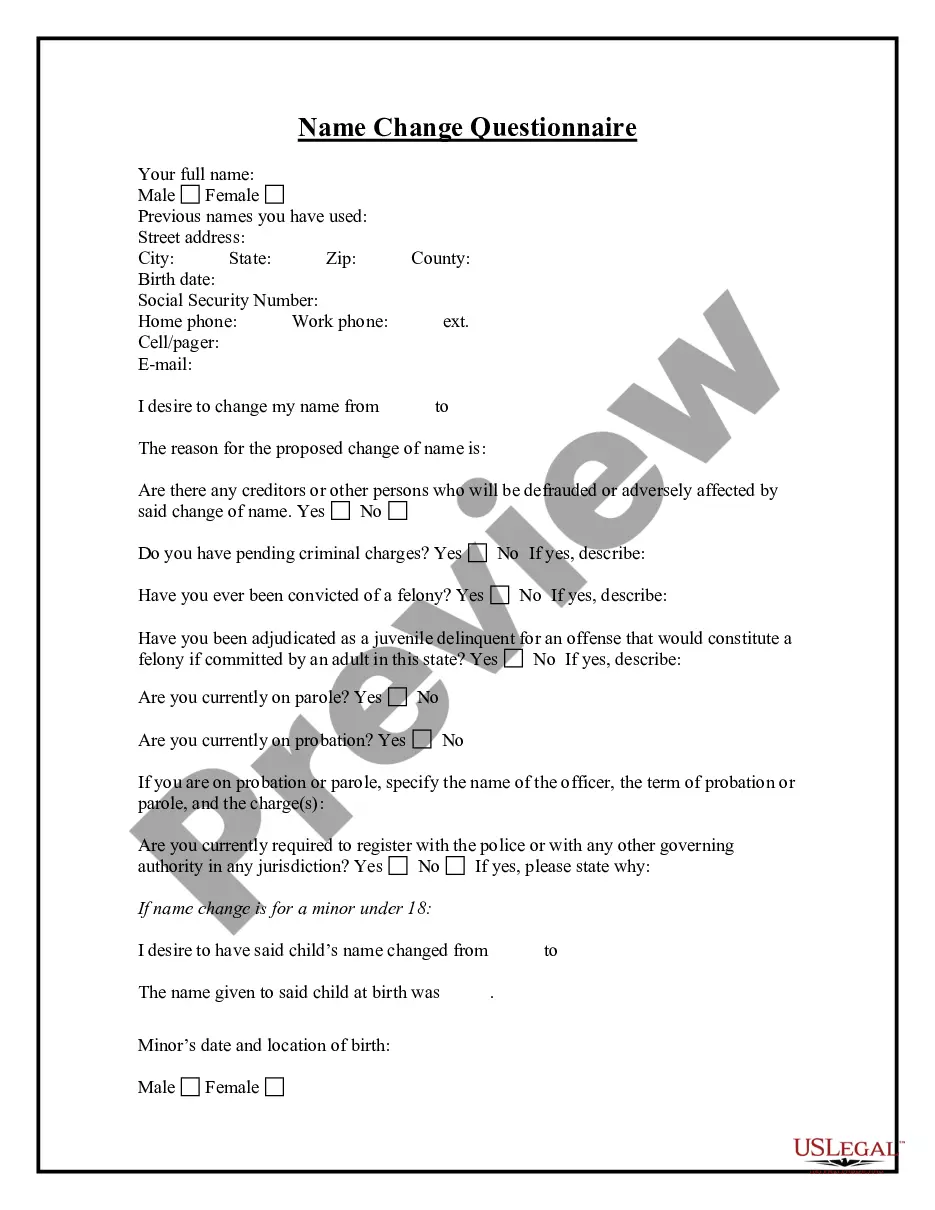
- Select the document you need and ensure it is for the appropriate city/county.
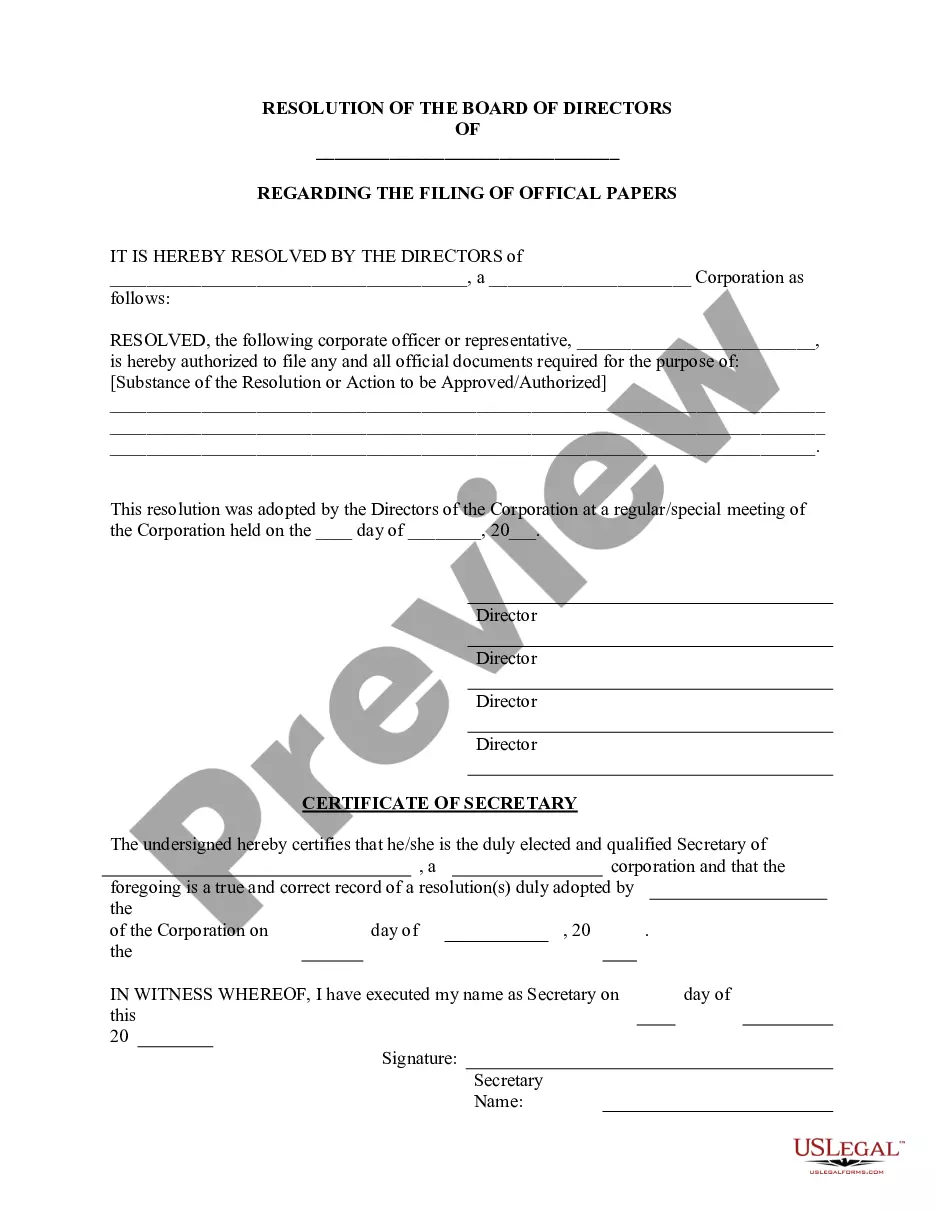
- Utilize the Review option to assess the form.
- Examine the summary to confirm you have chosen the correct document.
- If the document is not what you’re looking for, use the Search field to find the form that meets your needs.
- When you identify the correct document, click Purchase now.
- Choose the pricing plan you prefer, fill in the necessary information to create your account, and complete the payment using your PayPal or credit card.
- Select a convenient file format and download your version.
- Find all the document templates you have purchased in the My documents menu.
Form popularity
FAQ
HIPAA laws require organizations to implement safeguards to protect patient data from unauthorized access. This includes establishing policies for the use and sharing of protected health information. Utilizing the Missouri Authorization for Use and / or Disclosure of Protected Health Information can streamline these processes and enhance your compliance efforts.
Disclosure of Protected Health Information (PHI) is permitted under HIPAA in several scenarios, as highlighted in the Missouri Authorization for Use and/or Disclosure of Protected Health Information. This includes instances where a patient provides consent, the disclosure is required by law, or when needed for public health activities. Understanding these guidelines can greatly aid compliance and ensure that respects patient confidentiality.
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).
Under the HIPAA Privacy Rule, a covered entity must disclose protected health information in only two situations: (a) to individuals (or their personal representatives) specifically when they request access to, or an accounting of disclosures of, their protected health information; and (b) to the Department of Health
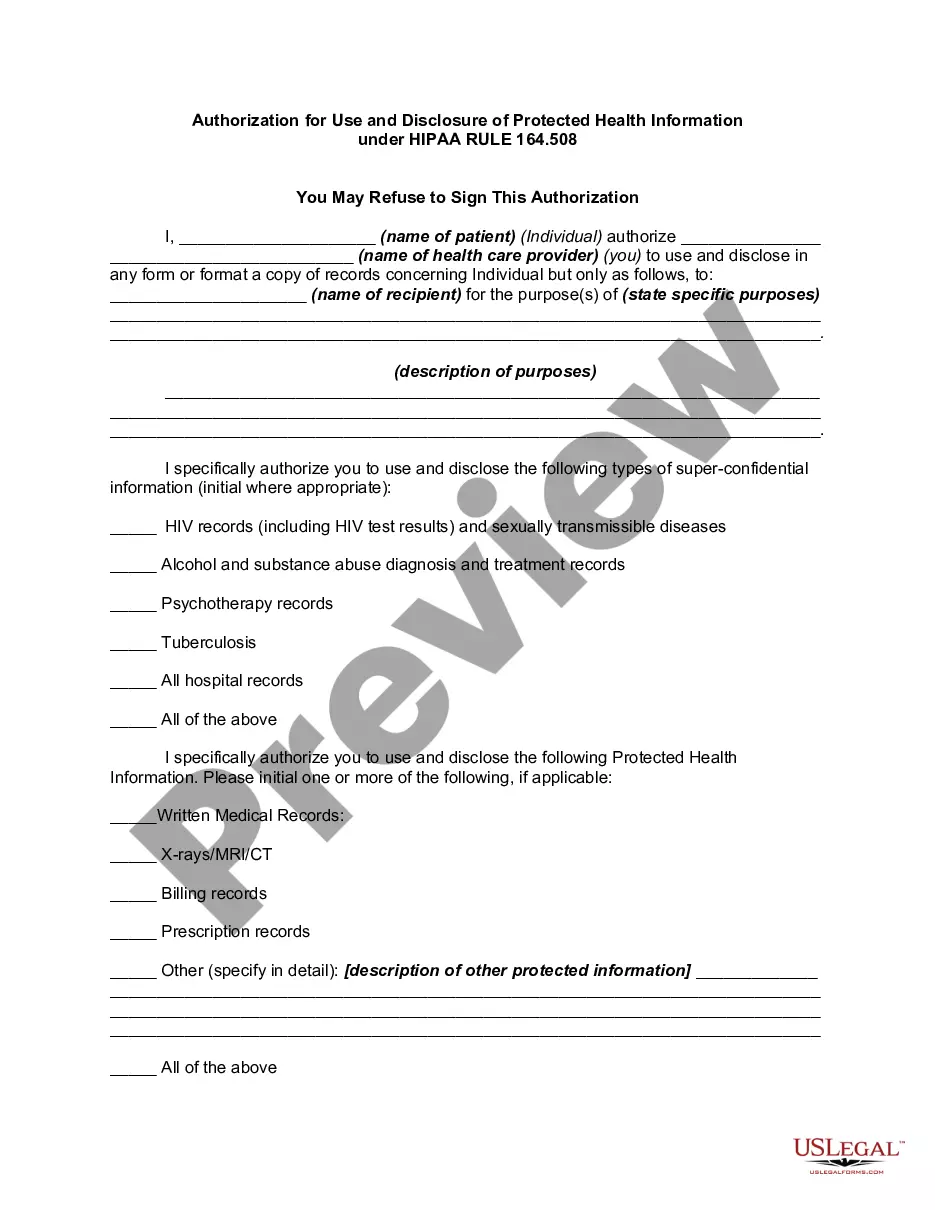
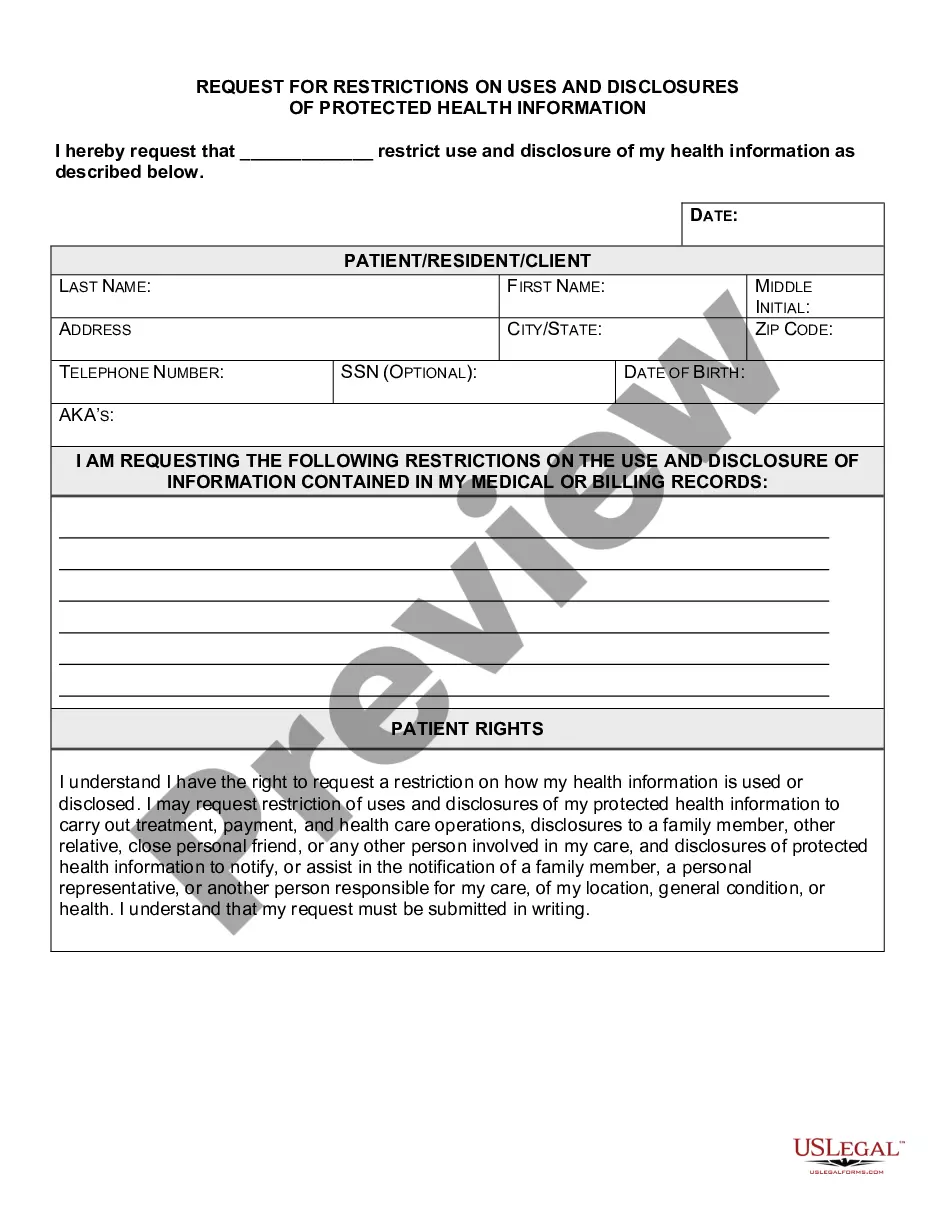
Valid HIPAA Authorizations: A ChecklistNo Compound Authorizations. The authorization may not be combined with any other document such as a consent for treatment.Core Elements.Required Statements.Marketing or Sale of PHI.Completed in Full.Written in Plain Language.Give the Patient a Copy.Retain the Authorization.
Marketing Activities: A covered entity must obtain an individual's authorization prior to using or disclosing PHI for marketing activities. Marketing is considered any message or statement to the public in an effort to get them to use or seek more information about a product or service.
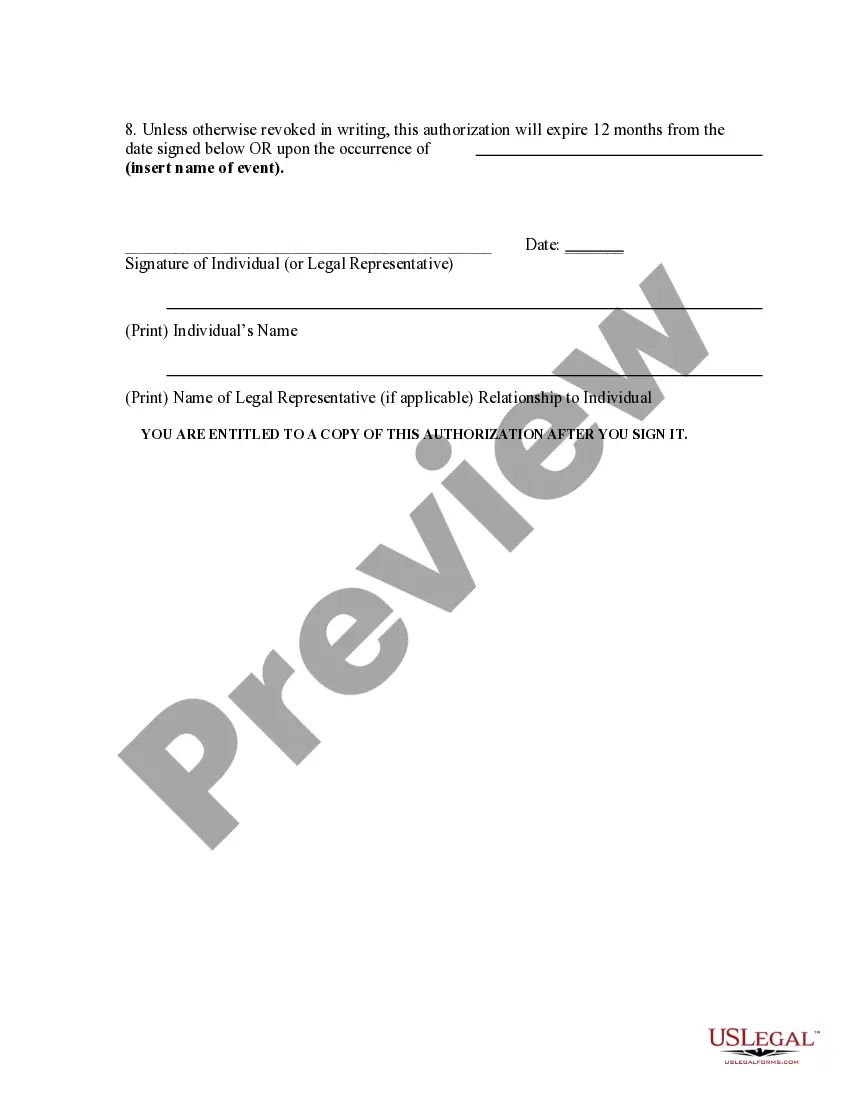
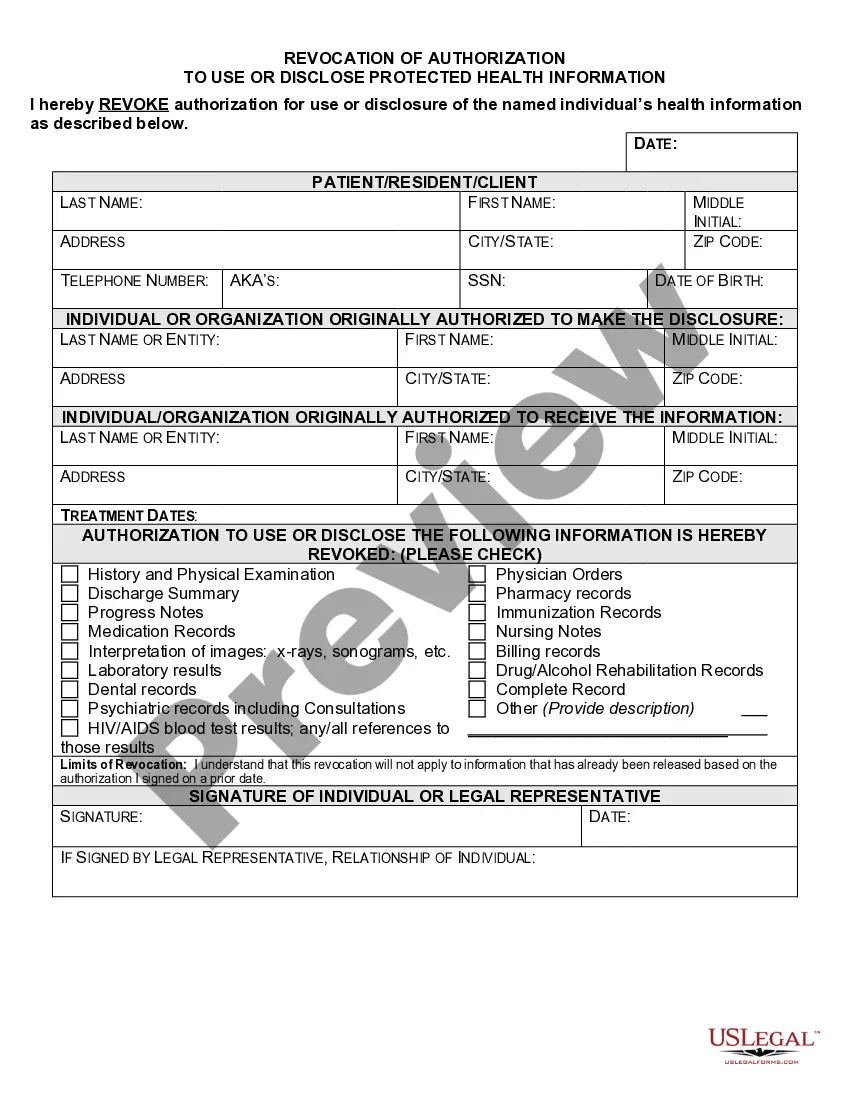
What are two required elements of an authorization needed to disclose PHI? Response Feedback: All authorizations to disclose PHI must have an expiration date and provide an avenue for the patient to revoke his or her authorization. What does the term "Disclosure" mean?
An authorization must specify a number of elements, including a description of the protected health information to be used and disclosed, the person authorized to make the use or disclosure, the person to whom the covered entity may make the disclosure, an expiration date, and, in some cases, the purpose for which the
A patient authorization is not required for disclosure of PHI between Covered Entities if the disclosure is needed for purposes of treatment or payment or for healthcare operations. You may disclose the PHI as long as you receive a request in writing.