Missouri Affidavit of No Coverage by Another Group Health Plan
Instant download
Description
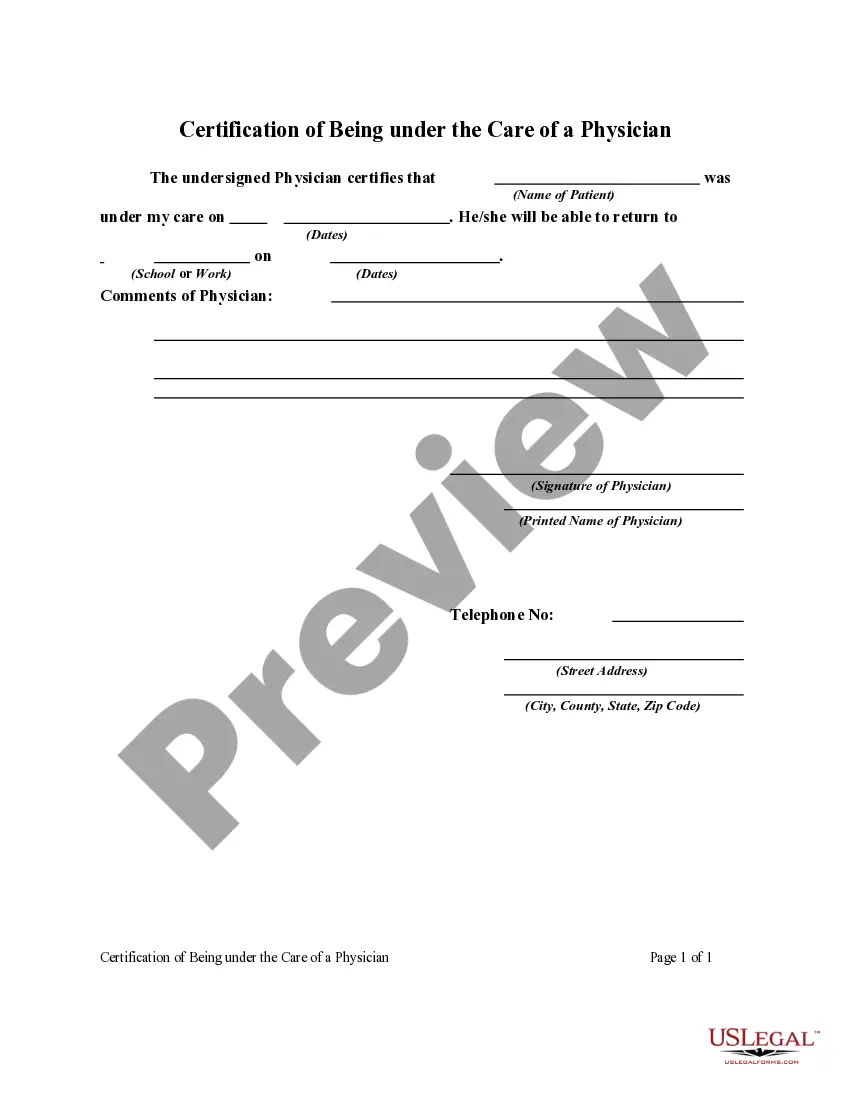
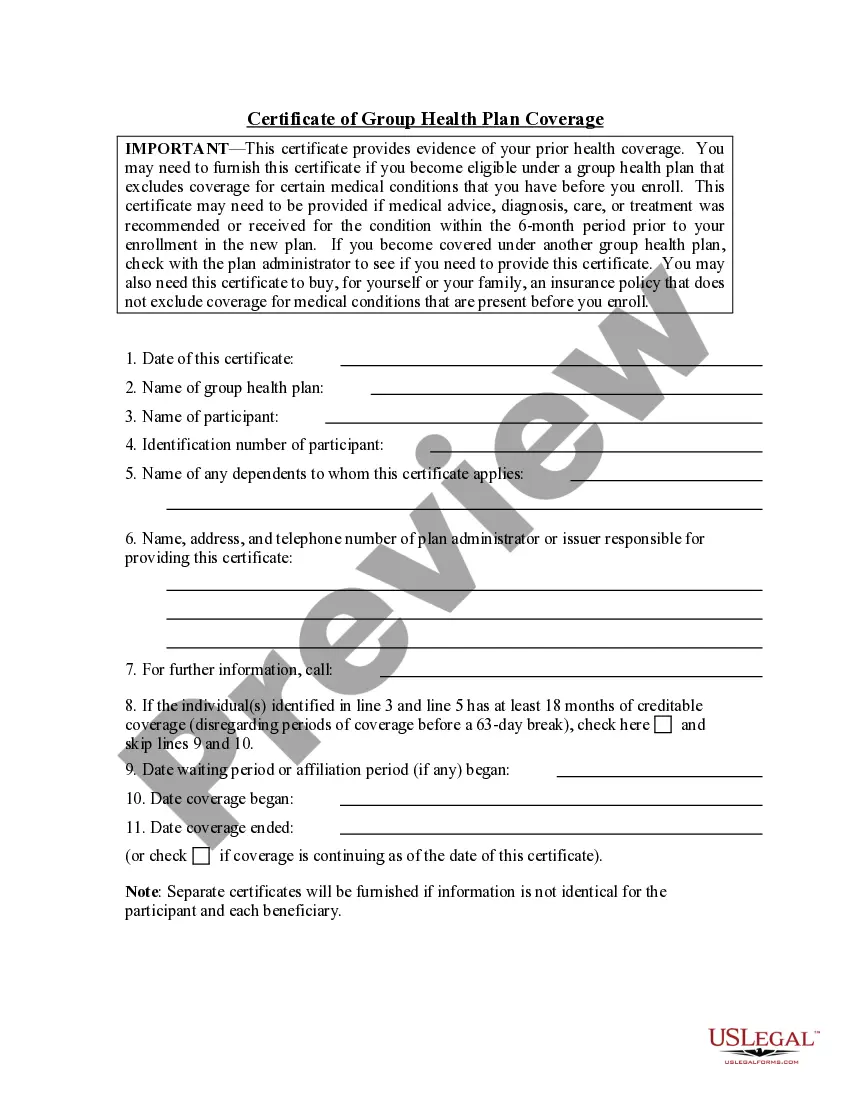
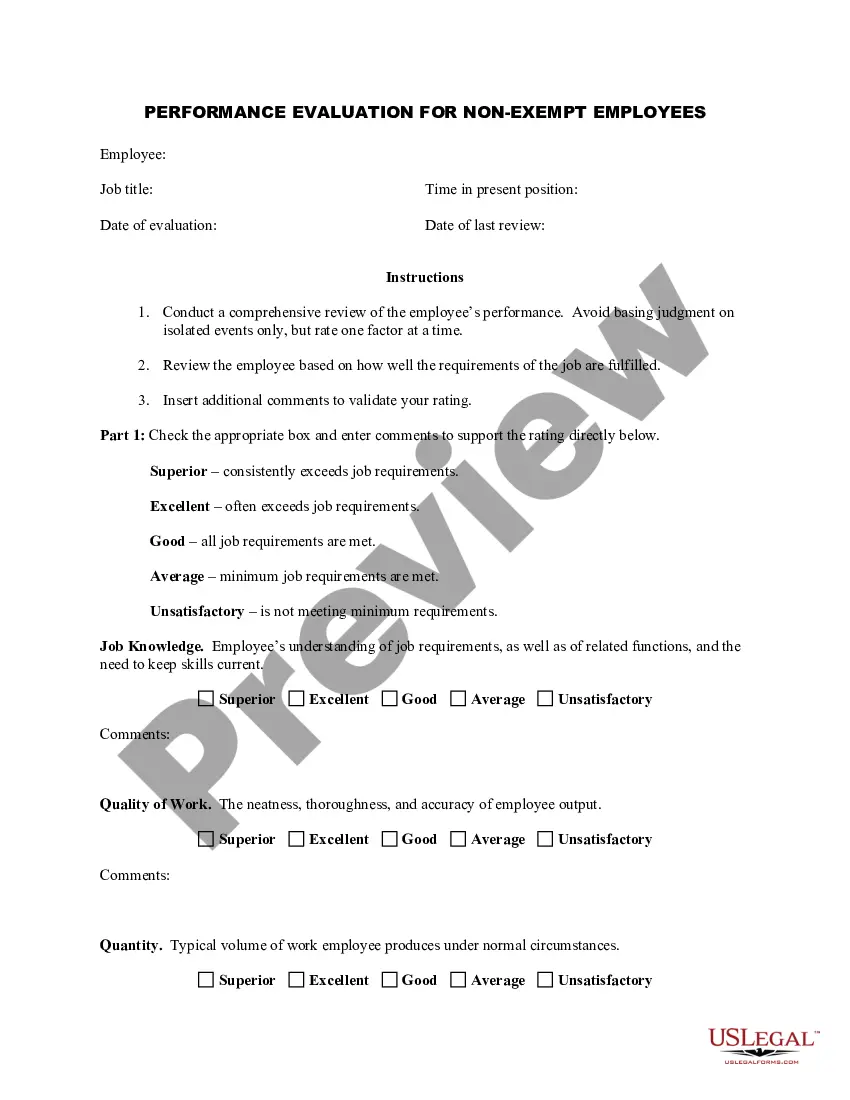
The employee named in this affidavit attests to the fact that he or she is not covered by any other group health plan.
How to fill out Affidavit Of No Coverage By Another Group Health Plan?
You can spend countless hours online searching for the valid document template that meets the federal and state guidelines you need.
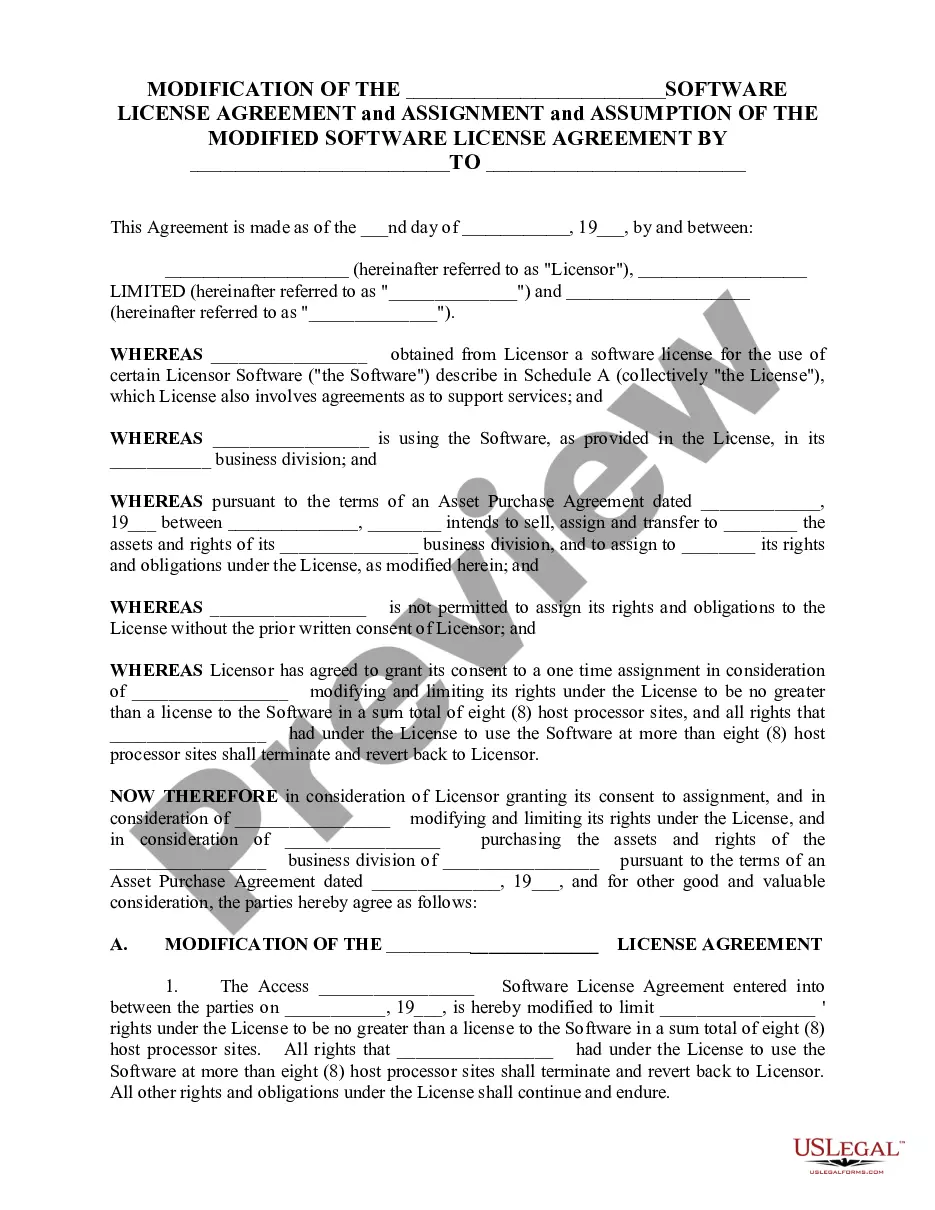
US Legal Forms provides thousands of valid templates that are reviewed by experts.
It is easy to download or print the Missouri Affidavit of No Coverage by Another Group Health Plan from the service.
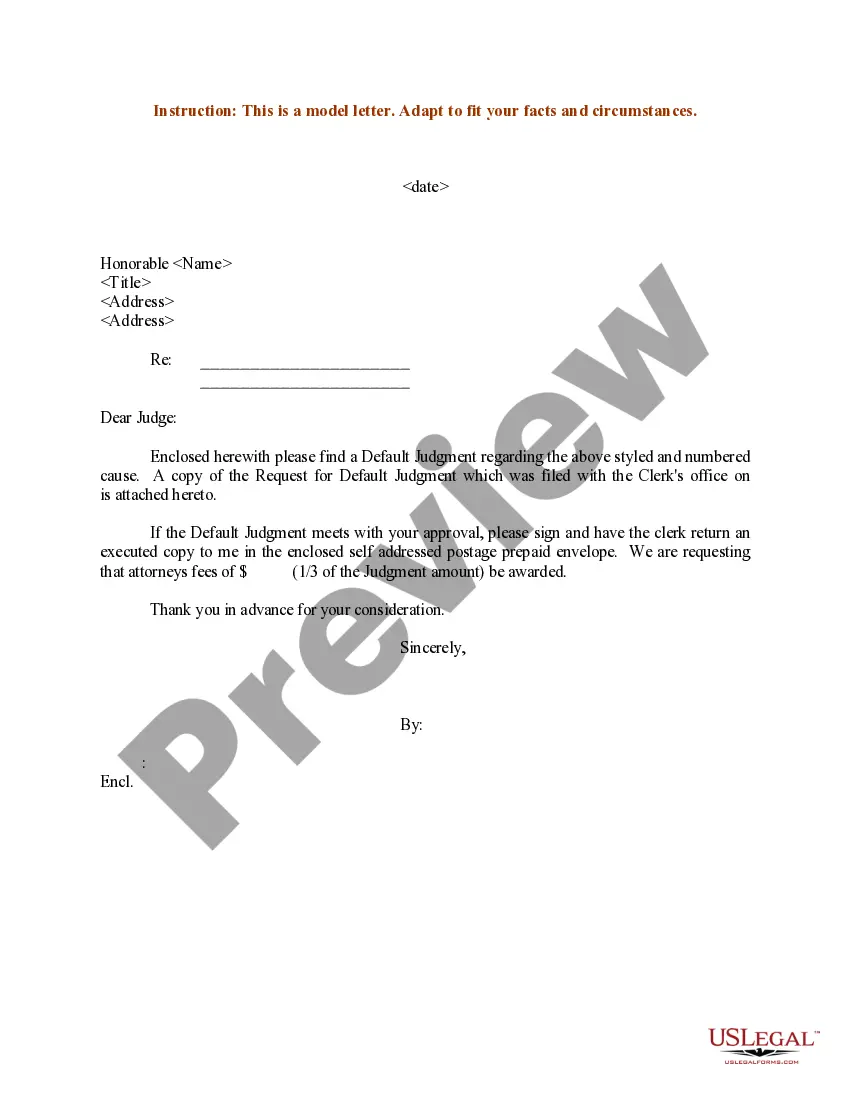
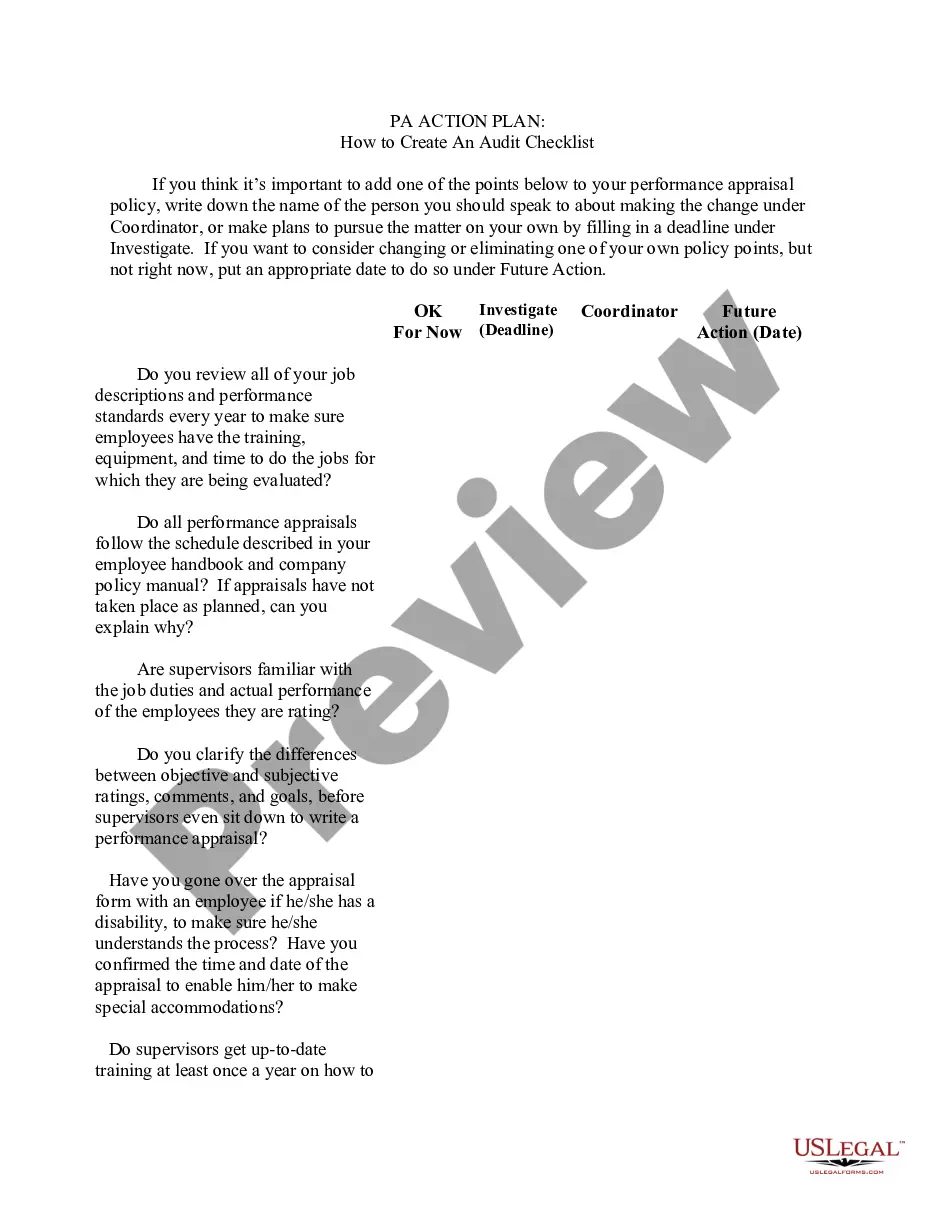
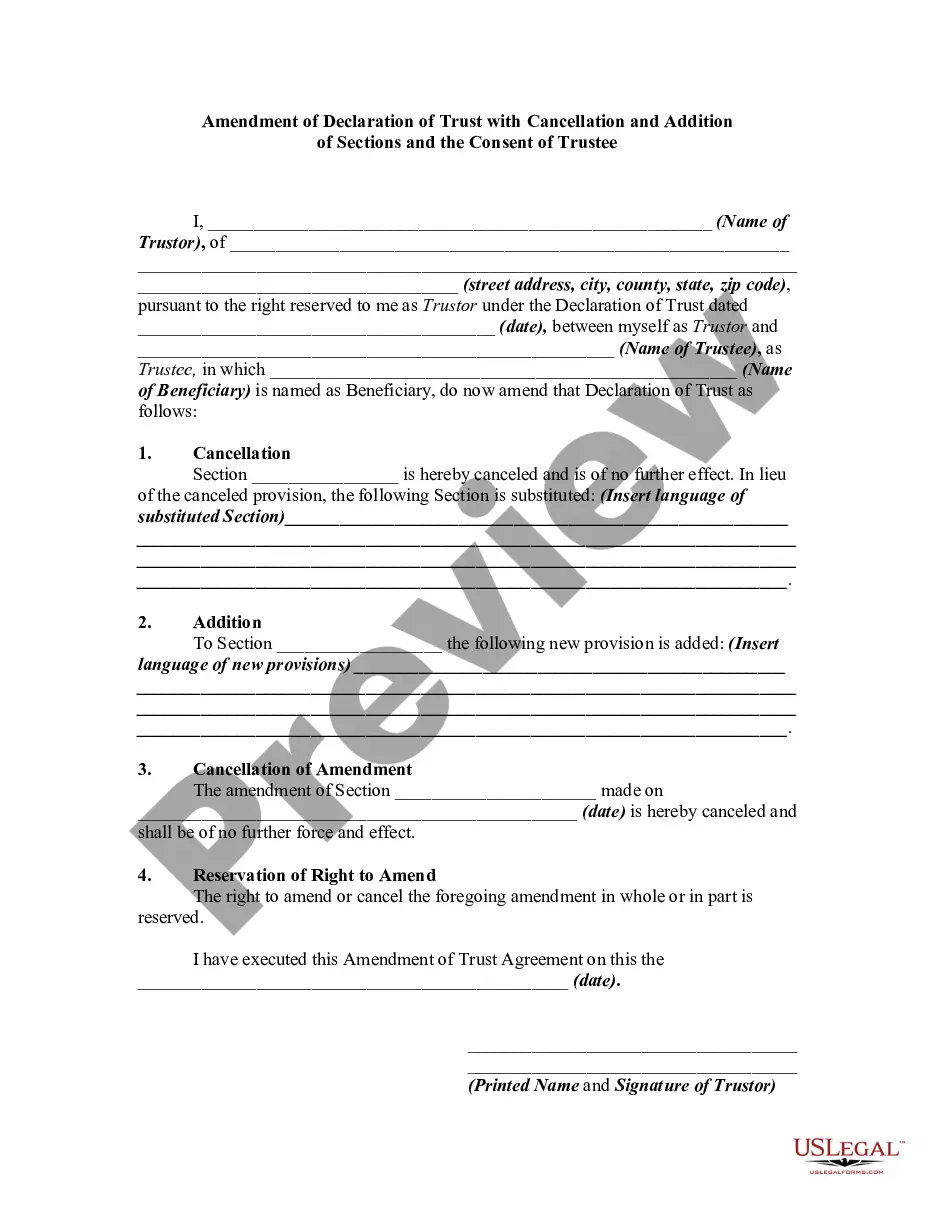
First, ensure you have selected the correct document template for the region/area you choose. Review the form outline to confirm you have selected the right form. If available, use the Review option to browse the document template as well.
- If you possess a US Legal Forms account, you can Log In and select the Download option.
- Then, you can complete, modify, print, or sign the Missouri Affidavit of No Coverage by Another Group Health Plan.
- Every valid document template you obtain is yours permanently.
- To get an additional copy of the downloaded form, go to the My documents tab and select the corresponding option.
- If you are using the US Legal Forms website for the first time, follow the simple instructions below.