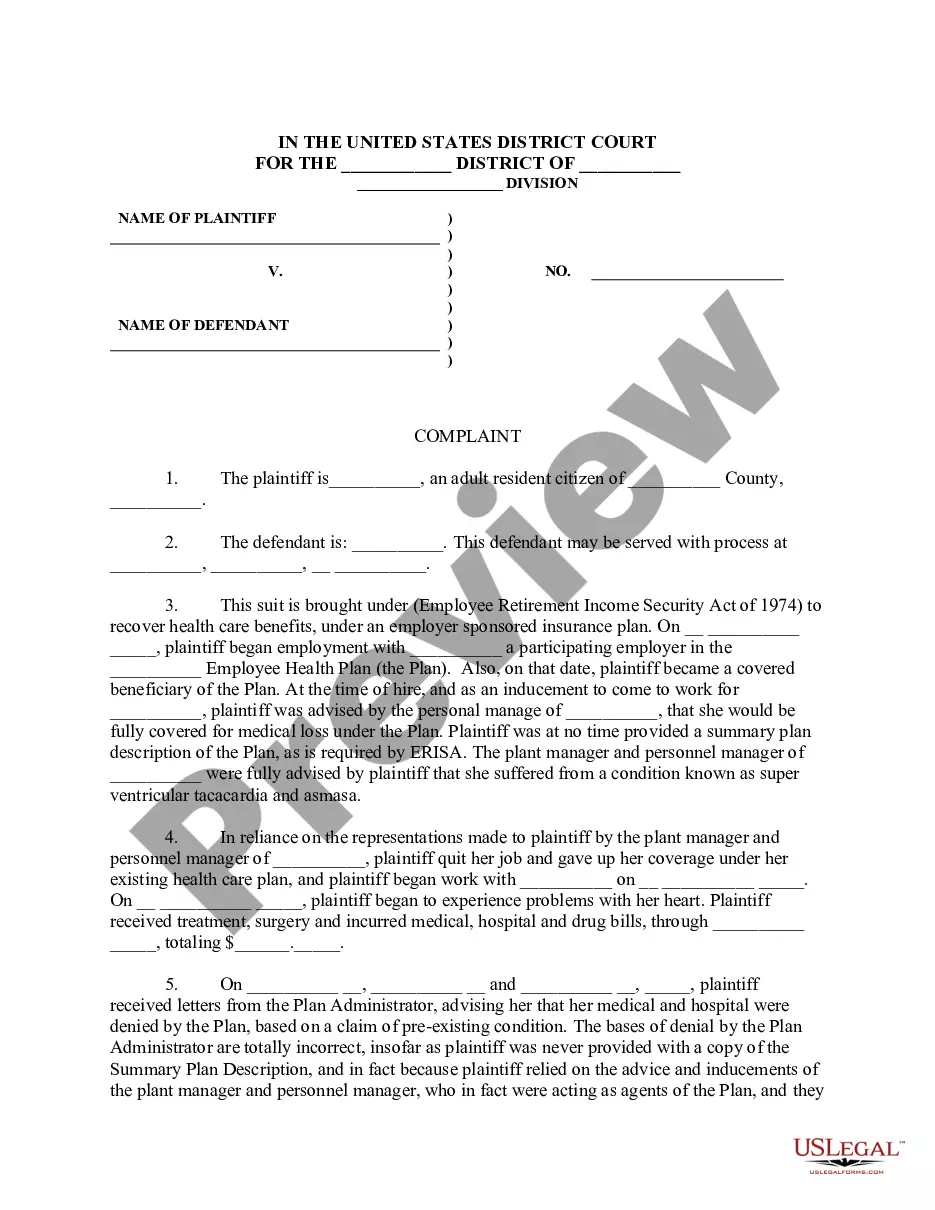
This form is a Complaint For Declaratory Judgment To Determine ERISA Coverage. Adapt to your specific circumstances. Don't reinvent the wheel, save time and money.
Montana Complaint for Declaratory Judgment to Determine ERICA Coverage is a legal document filed in the state of Montana to seek clarification on whether a particular employee benefit plan or program falls under the jurisdiction of the Employee Retirement Income Security Act (ERICA). In Montana, there are various types of Complaints for Declaratory Judgment to Determine ERICA Coverage, which may include: 1. Group Health Plan Coverage: This type of complaint is filed when there is uncertainty about whether a group health plan provided by an employer qualifies as an ERICA plan. 2. Pension Plan Coverage: When an employer provides a retirement or pension plan, there may be a question whether it qualifies as an ERICA plan. This complaint is filed to seek a declaratory judgment on ERICA coverage in such cases. 3. Disability Plan Coverage: Employers often provide short-term or long-term disability plans to their employees. This complaint may be filed when there is ambiguity about whether a specific disability plan is subject to ERICA regulations. 4. Life Insurance Plan Coverage: If there is a dispute regarding whether a life insurance plan offered by an employer falls under ERICA provisions, a complaint for declaratory judgment may be filed to determine the ERICA coverage. 5. Severance Plan Coverage: Employers sometimes provide severance plans to their employees. This type of complaint is filed to clarify whether a particular severance plan is governed by ERICA. 6. Employee Benefit Program Coverage: This category encompasses other employee benefit programs, such as dental or vision plans, wellness programs, or employee assistance programs. If there is uncertainty about ERICA coverage for these programs, a complaint for declaratory judgment may be filed. In a Complaint for Declaratory Judgment to Determine ERICA Coverage, the party filing the complaint (the Plaintiff) will typically outline the facts of the case, describe the employee benefit plan or program in question, and provide reasons supporting their belief that the plan falls under ERICA. The Plaintiff may also name defendants, such as the employer, plan administrator, or insurance company, who may have opposing views on ERICA coverage. The complaint will generally include relevant keywords such as ERICA, employee benefits, coverage determination, clarification, plan administrator, pension, disability, life insurance, group health plan, severance plan, and other applicable terms to ensure it is easily discoverable for legal professionals and researchers investigating ERICA coverage disputes in Montana.