Montana General Notice of Preexisting Condition Exclusion serves as an essential informational document that outlines the specifics of preexisting condition exclusions in relation to health insurance coverage in the state of Montana. This notice provides individuals with crucial details regarding the circumstances under which their preexisting conditions may not be covered by the insurance plan. Preexisting condition exclusions typically refer to any health condition, injury, or illness that existed prior to the effective date of a new insurance policy. This notice aims to educate individuals on the potential limitations and restrictions related to such conditions when seeking coverage. By understanding these exclusions, individuals can make informed decisions about their healthcare and insurance needs. Montana mandates that insurance providers clearly communicate preexisting condition exclusions to policyholders through the General Notice of Preexisting Condition Exclusion. It ensures transparency in the insurance process and enables individuals to comprehend the scope of coverage available for their preexisting medical conditions. The Montana General Notice of Preexisting Condition Exclusion may vary depending on the type of health insurance plan. For instance, individuals covered under employer-sponsored group health plans may receive a specific notice outlining the terms and duration of preexisting condition exclusions. On the other hand, individuals purchasing individual health insurance policies will receive a notice tailored to their specific situation. When receiving the notice, it is crucial to carefully review its contents. Key information mentioned in the Montana General Notice of Preexisting Condition Exclusion may include the length of the exclusionary period, which is the duration during which coverage for preexisting conditions is limited or denied. The notice may also describe circumstances under which the exclusionary period can be reduced or eliminated, such as continuous prior coverage. Other keywords related to the Montana General Notice of Preexisting Condition Exclusion include health insurance regulations, coverage limitations, preexisting condition waiting periods, prior health coverage, effective dates, health plan exclusions, essential health benefits, and insurance benefits. Understanding the Montana General Notice of Preexisting Condition Exclusion is imperative for individuals seeking health insurance coverage in Montana. By familiarizing themselves with the specific terms and conditions, individuals can manage their healthcare expectations, make informed decisions about policy selection, and ensure they have appropriate coverage for their preexisting medical conditions.
Montana General Notice of Preexisting Condition Exclusion
Description
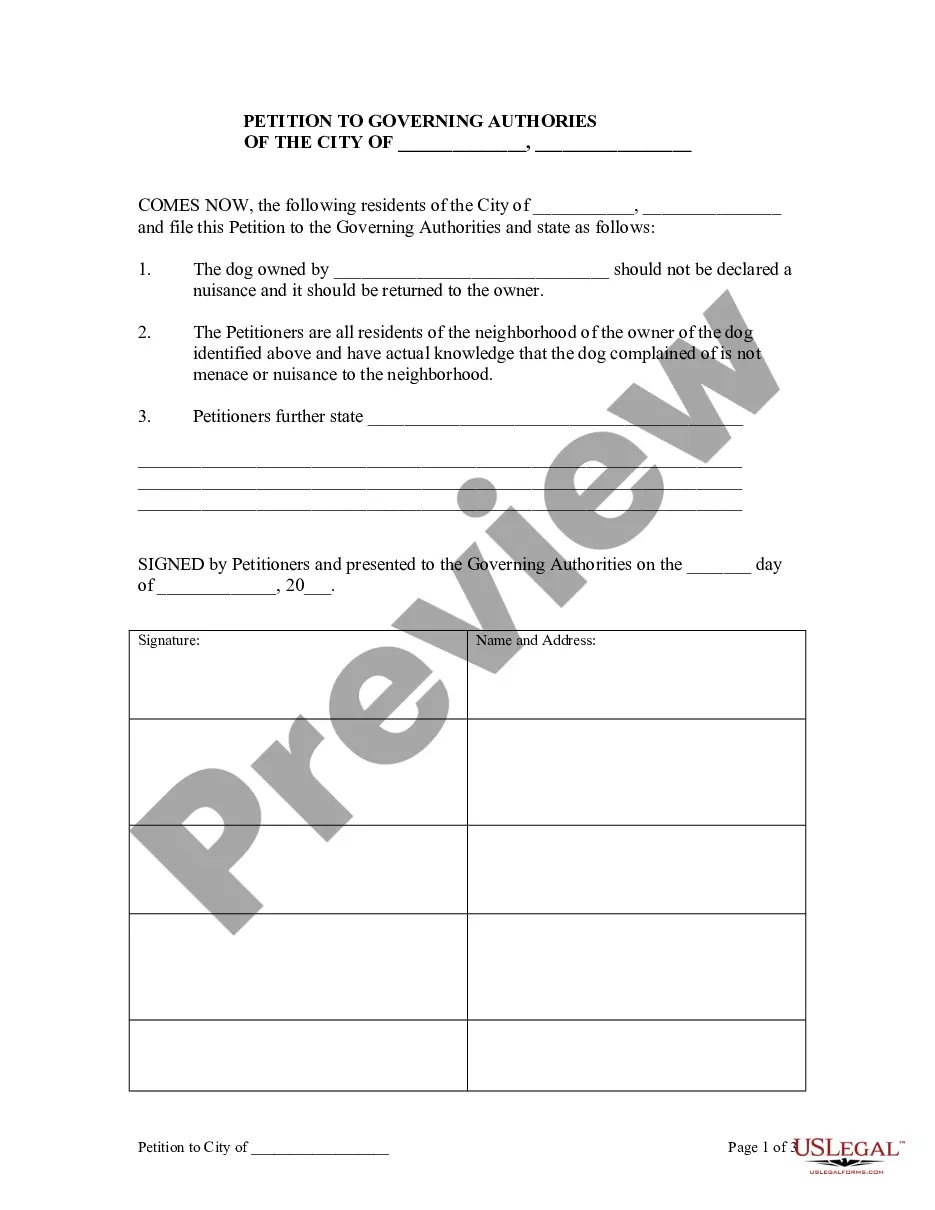
How to fill out Montana General Notice Of Preexisting Condition Exclusion?
You may invest hours on-line looking for the lawful papers format which fits the state and federal specifications you want. US Legal Forms supplies 1000s of lawful types that are examined by experts. You can actually download or print the Montana General Notice of Preexisting Condition Exclusion from my support.
If you already have a US Legal Forms bank account, you can log in and click the Acquire key. Afterward, you can comprehensive, edit, print, or indication the Montana General Notice of Preexisting Condition Exclusion. Every lawful papers format you get is the one you have for a long time. To have one more version of the obtained form, go to the My Forms tab and click the related key.
Should you use the US Legal Forms site initially, keep to the simple directions listed below:
- Initially, be sure that you have chosen the correct papers format for the state/metropolis of your choice. Browse the form description to make sure you have picked the appropriate form. If readily available, make use of the Preview key to search through the papers format also.
- If you want to discover one more version from the form, make use of the Lookup field to get the format that fits your needs and specifications.
- Upon having discovered the format you would like, click Buy now to carry on.
- Find the pricing plan you would like, type in your references, and sign up for a merchant account on US Legal Forms.
- Total the deal. You can utilize your charge card or PayPal bank account to pay for the lawful form.
- Find the structure from the papers and download it in your gadget.
- Make adjustments in your papers if necessary. You may comprehensive, edit and indication and print Montana General Notice of Preexisting Condition Exclusion.
Acquire and print 1000s of papers templates utilizing the US Legal Forms web site, which provides the largest selection of lawful types. Use professional and status-particular templates to take on your business or person demands.