North Carolina Medical Release
Description
How to fill out Medical Release?
Selecting the most suitable legitimate document template can be a challenge.
Of course, there are numerous designs accessible online, but how do you find the genuine form you require.
Utilize the US Legal Forms website.
If you are a first-time user of US Legal Forms, here are simple instructions you should follow: First, ensure you have selected the correct form for your city/state. You can review the form using the Review button and examine the form outline to confirm it is suitable for you. If the form does not satisfy your needs, use the Search box to find the correct document. When you are confident that the form is appropriate, click on the Get now button to download the form. Choose the pricing plan you desire and provide the required information. Create your account and pay for your order using your PayPal account or credit card. Select the file format and download the legitimate document template to your device. Complete, modify, print, and sign the received North Carolina Medical Release. US Legal Forms is the largest repository of legitimate documents where you can find numerous paperwork templates. Use the service to download professionally crafted files that adhere to state requirements.
- The service provides an extensive range of templates, such as the North Carolina Medical Release, which can be used for both business and personal purposes.
- All documents are verified by experts and comply with state and federal regulations.
- If you are already registered, Log In to your account and then click the Obtain button to download the North Carolina Medical Release.
- Use your account to browse the legitimate forms you have acquired previously.
- Visit the My documents tab in your account to retrieve another copy of the documents you require.
Form popularity
FAQ
Medical release means a program enabling the Commission to release inmates who are permanently and totally disabled, terminally ill, or geriatric.
Medical records are the document that explains all detail about the patient's history, clinical findings, diagnostic test results, pre and postoperative care, patient's progress and medication. If written correctly, notes will support the doctor about the correctness of treatment.
Can I view my medical records? Yes. You have a legal right to see your own records. You do not have to explain why you want to see them.
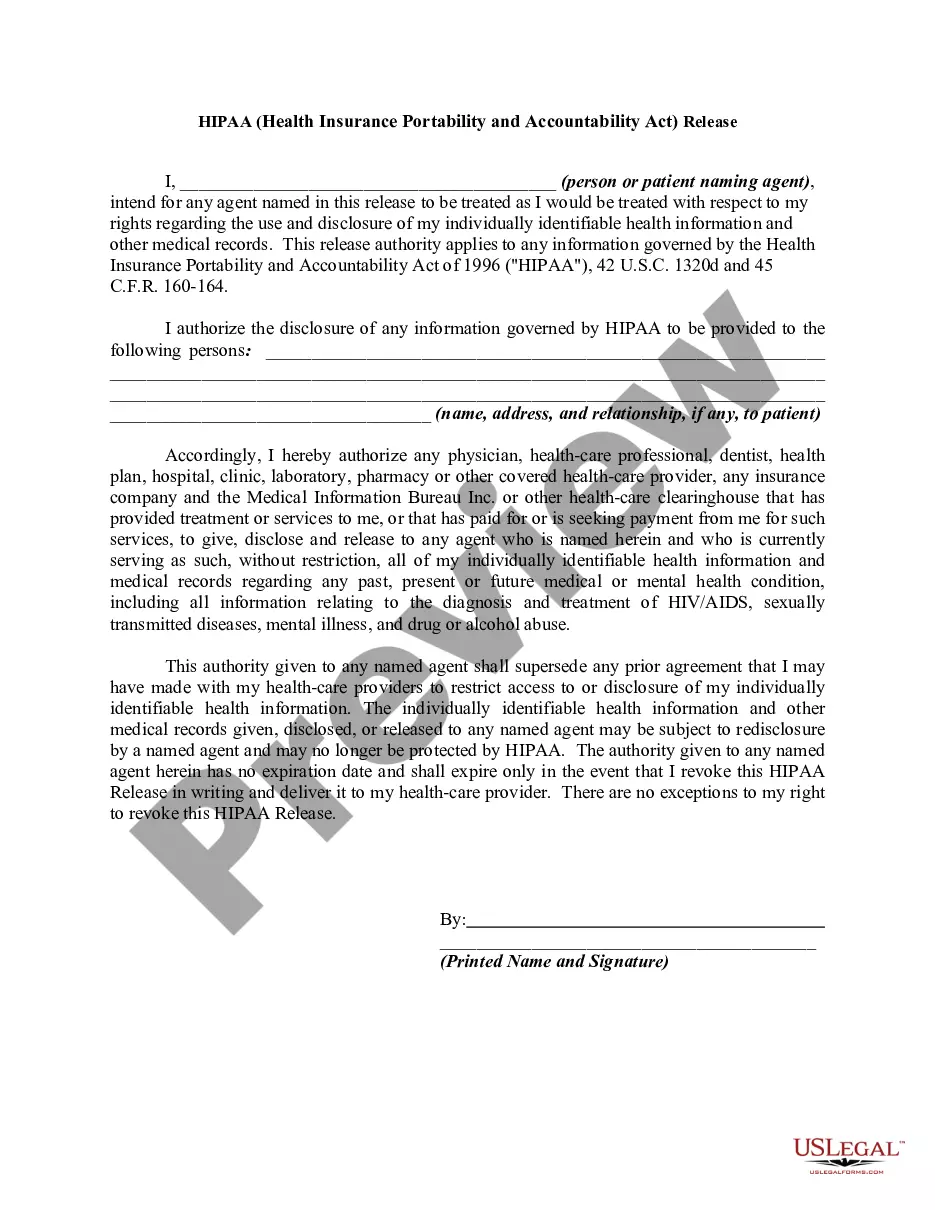
Elements of a release formPatient information. Naturally, the release should require the patient's information so it's clear who the form refers to.Receiving party's information.Information to be shared.Purpose of the release.Expiration of authorization.Disclaimers.Date and signature.
3903 North Carolina Department of Health and Human Services is charged with creating policy regarding "health care facilities", and is written primarily for hospitals. According to the DHHS medical records of a facility must be maintained for at least 11 years after an adult patient's discharge.
To obtain a copy of the medical records you must request the records from the medical care provider. To provide these medical records to you, your health care provider must follow government privacy laws called HIPAA. HIPAA is the Health Insurance Portability and Accountability Act of 1996.
North Carolina General Statutes §90-411$0.75 for first 25 pages. $0.50 for pages 26-100. $0.25 for pages over 100. Minimum fee of $10.00 permitted.
NOTE: Records must be retained 11 years after last encounter at hospital. NOTE: Records must be retained 11 years after last encounter. NOTE: Records must be retained until the patient reaches 19 years of age in addition to this minimum time requirement.
The patient's legal name, date of birth, gender, Social Security number, address, telephone number, guarantor, subscriber, or next-of-kin are key identifying elements that assist in establishing the proper individual.
A medical liability waiver form is completed by medical professionals. It is used to get consent to treat a patient while also protecting themselves from liability if the patient is hurt or dies while in their care. This waiver generally also provides the patient of their privacy and legal rights.