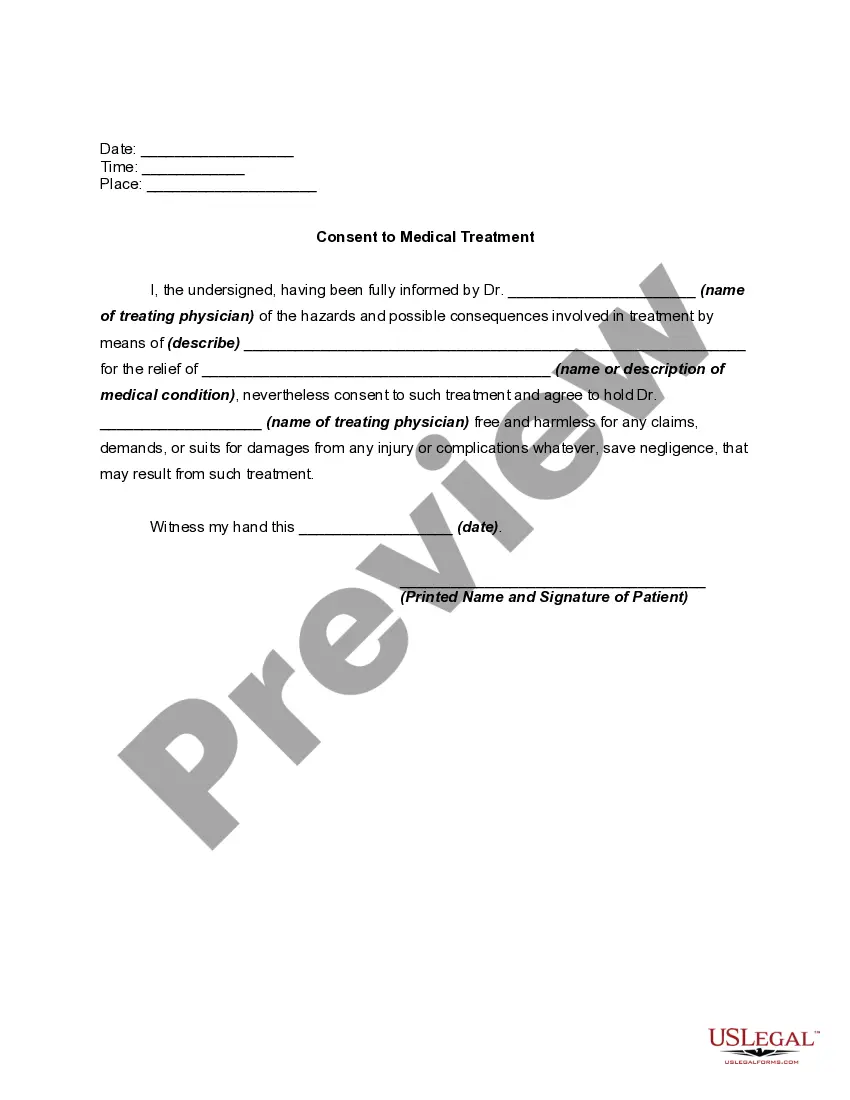
North Carolina Medical Consent for Unconscious Patient
Description
How to fill out Medical Consent For Unconscious Patient?
Selecting the appropriate authorized form template can be challenging.
Clearly, there are numerous templates accessible online, but how can you find the legal document you require.
Utilize the US Legal Forms website. The platform provides thousands of templates, including the North Carolina Medical Consent for Unconscious Patient, suitable for both business and personal use.
If the form does not meet your needs, utilize the Search field to find the appropriate form. Once you are sure the form is appropriate, click the Buy now button to acquire the form. Select your payment method and provide the necessary information. Create your account and complete the purchase using your PayPal account or credit card. Choose the file format and download the legal document template to your device. Complete, modify, print, and sign the acquired North Carolina Medical Consent for Unconscious Patient. US Legal Forms is the largest repository of legal documents where you can find various record templates. Use the service to download professionally crafted files that adhere to state requirements.
- All documents are reviewed by experts and comply with state and federal regulations.
- If you are already registered, Log In to your account and click the Download button to obtain the North Carolina Medical Consent for Unconscious Patient.
- Use your account to browse through the legal forms you have previously acquired.
- Go to the My documents tab in your account to retrieve another copy of the document you need.
- If you are a new user of US Legal Forms, here are some simple steps you can follow.
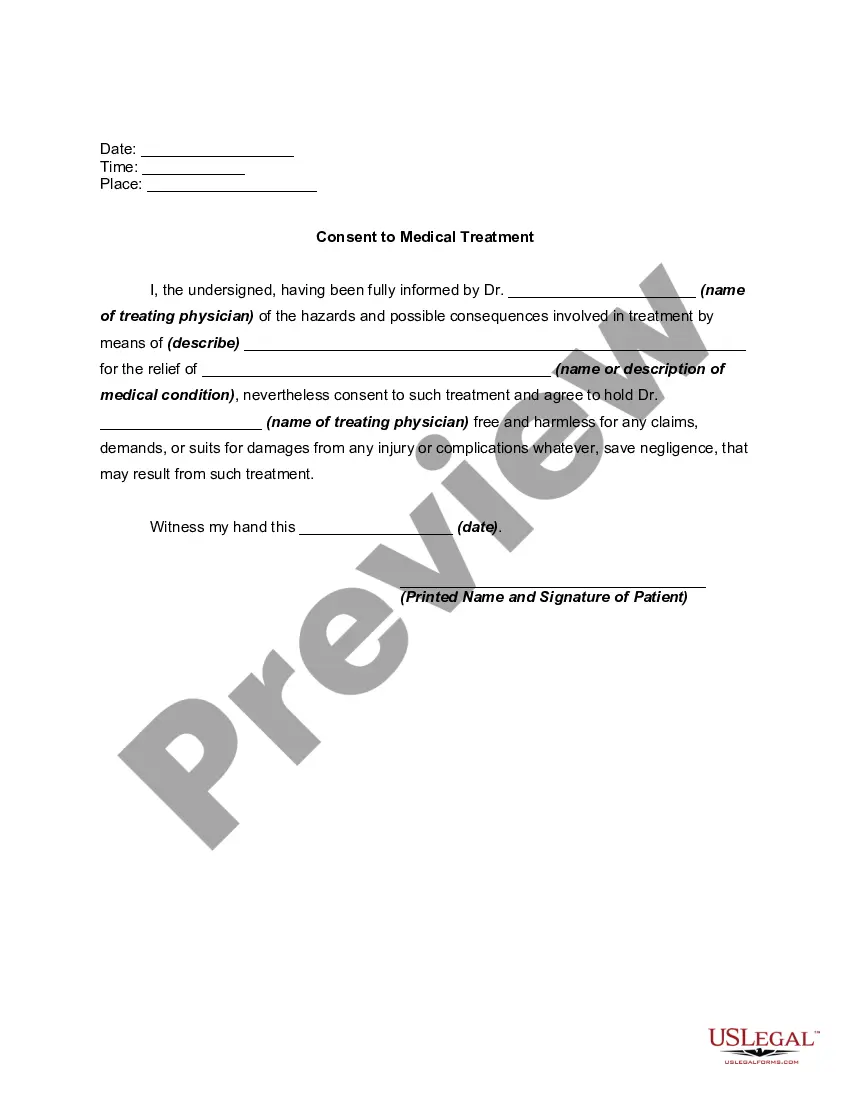
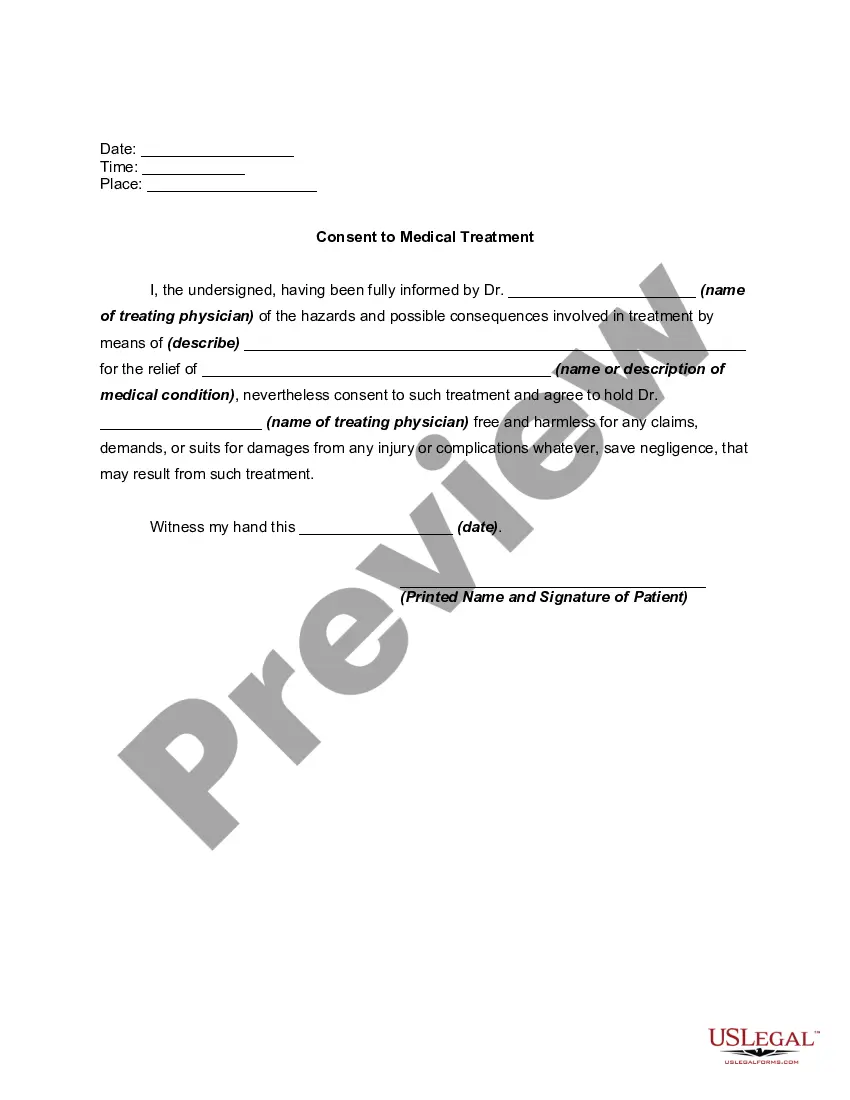
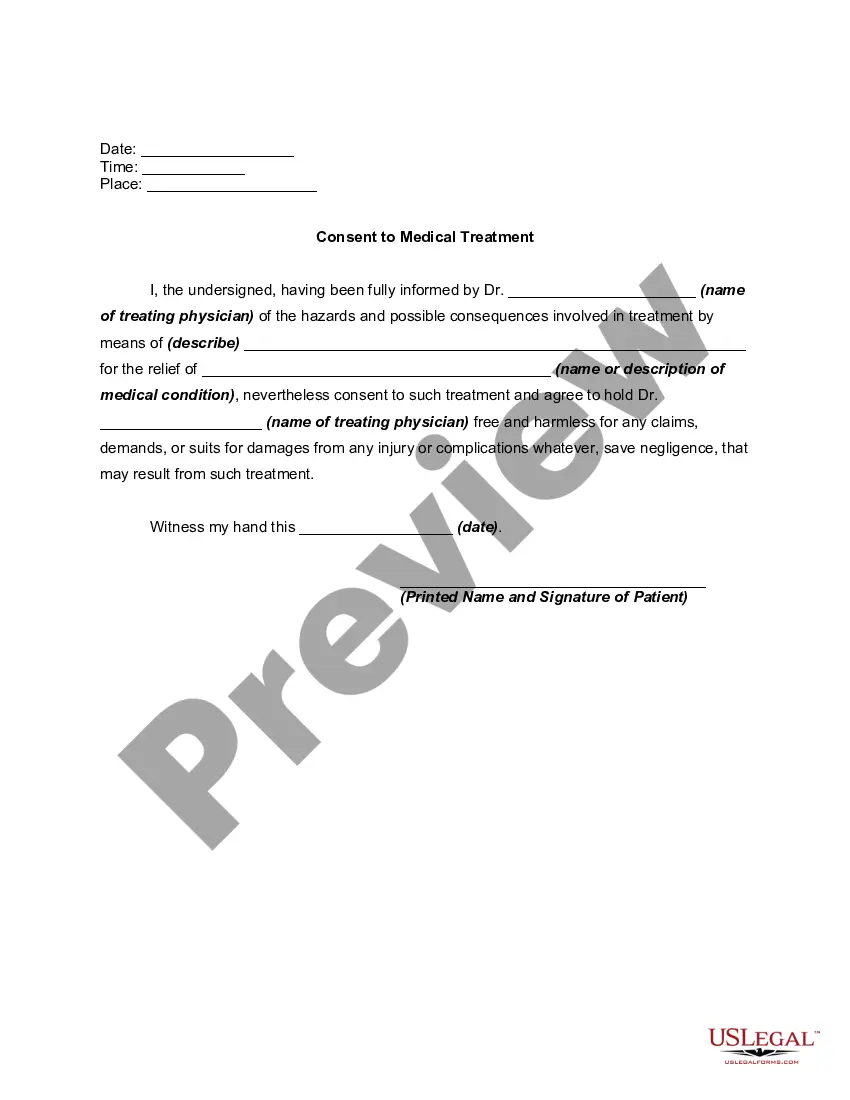
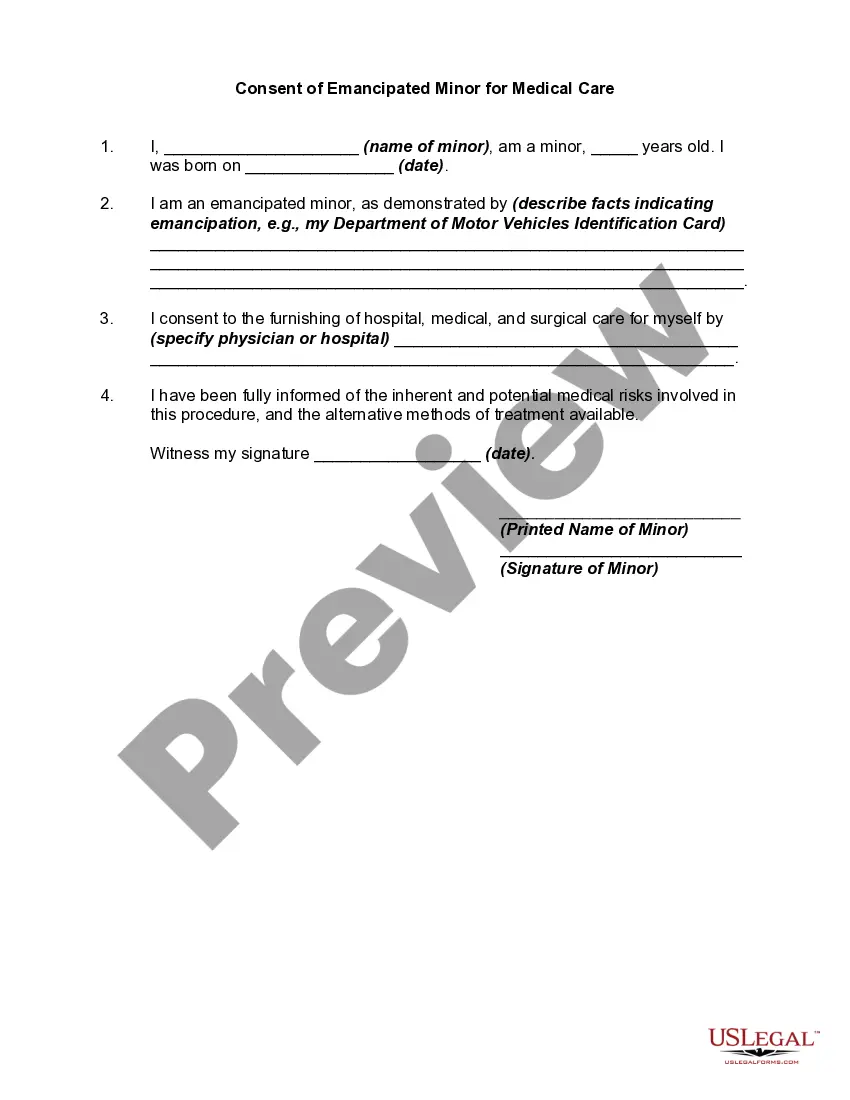
- First, ensure you have selected the correct form for your area/region. You can preview the form using the Review button and read the form description to confirm it is suitable for you.
Form popularity
FAQ
For an unconscious patient, implied consent is used, allowing medical providers to act without explicit agreement. This type of consent is vital in urgent situations where delays could harm the patient. Familiarizing yourself with North Carolina Medical Consent for Unconscious Patient guidelines can help in delivering timely and appropriate care.
When a person is unconscious, the type of consent applied is often termed implied consent. This is based on the understanding that a patient would agree to necessary medical treatment if they were able to communicate. Knowing how to navigate North Carolina Medical Consent for Unconscious Patient can help healthcare professionals make informed decisions swiftly.
Obtaining informed consent from an unconscious patient can be challenging, as the patient cannot communicate their wishes. In these situations, healthcare professionals rely on implied consent, allowing them to proceed with emergency care. It is important to follow local laws and regulations regarding North Carolina Medical Consent for Unconscious Patient to safeguard both the patient and provider.
In North Carolina, when a patient is unconscious, implied consent typically applies. This means that consent is assumed based on the situation, where immediate medical attention is necessary. Healthcare providers act in the best interest of the patient to provide essential treatment. Understanding North Carolina Medical Consent for Unconscious Patient ensures you comply with legal guidelines.
Handling informed consent for a North Carolina medical consent for an unconscious patient involves following established legal guidelines. Medical professionals typically assess the situation to determine if immediate treatment is necessary. If so, they may proceed under the assumption that consent would be granted if the patient were able to give it. For specific protocols and legal documentation, platforms like US Legal Forms can provide valuable resources to ensure compliance with North Carolina regulations.
Informed consent law in North Carolina requires healthcare providers to give patients relevant information about treatments, risks, and benefits before they agree to proceed. This law aims to protect patient autonomy while ensuring they make knowledgeable decisions. However, with unconscious patients, implied consent applies instead. For clarity on these legal requirements, you can explore resources like uslegalforms, which can help clarify North Carolina Medical Consent for Unconscious Patient.
When a patient is unresponsive, implied consent is utilized. Health professionals are legally allowed to administer emergency care without explicit permission because they operate under the assumption that the patient would consent to necessary treatment. This principle ensures that critical medical help can be given without delay. Understanding North Carolina Medical Consent for Unconscious Patient ensures you are well-prepared to respond effectively in such situations.
For a conscious casualty, you should ask for their explicit consent before providing any treatment. Explain what you plan to do and ensure they understand the procedure. Conversely, for an unconscious casualty, consent is presumed, allowing you to act in their best interest. Knowledge of North Carolina Medical Consent for Unconscious Patient reinforces the importance of understanding these consent dynamics.
To treat a patient who is unconscious, implied consent applies. This means that when a patient cannot communicate their wishes, approval for necessary medical treatment is assumed. Medical professionals can provide life-saving care under the premise that a reasonable person would consent if they were able to. Familiarizing yourself with North Carolina Medical Consent for Unconscious Patient will help clarify these legal aspects.
If a victim is unconscious, your priority is to ensure their safety and well-being. You should assess their condition and call for emergency medical assistance immediately. While waiting for help, it is essential to monitor their airway and breathing. Understanding North Carolina Medical Consent for Unconscious Patient can guide you on the legal duties surrounding treatment.