North Carolina Medical Consent for Treatment
Description
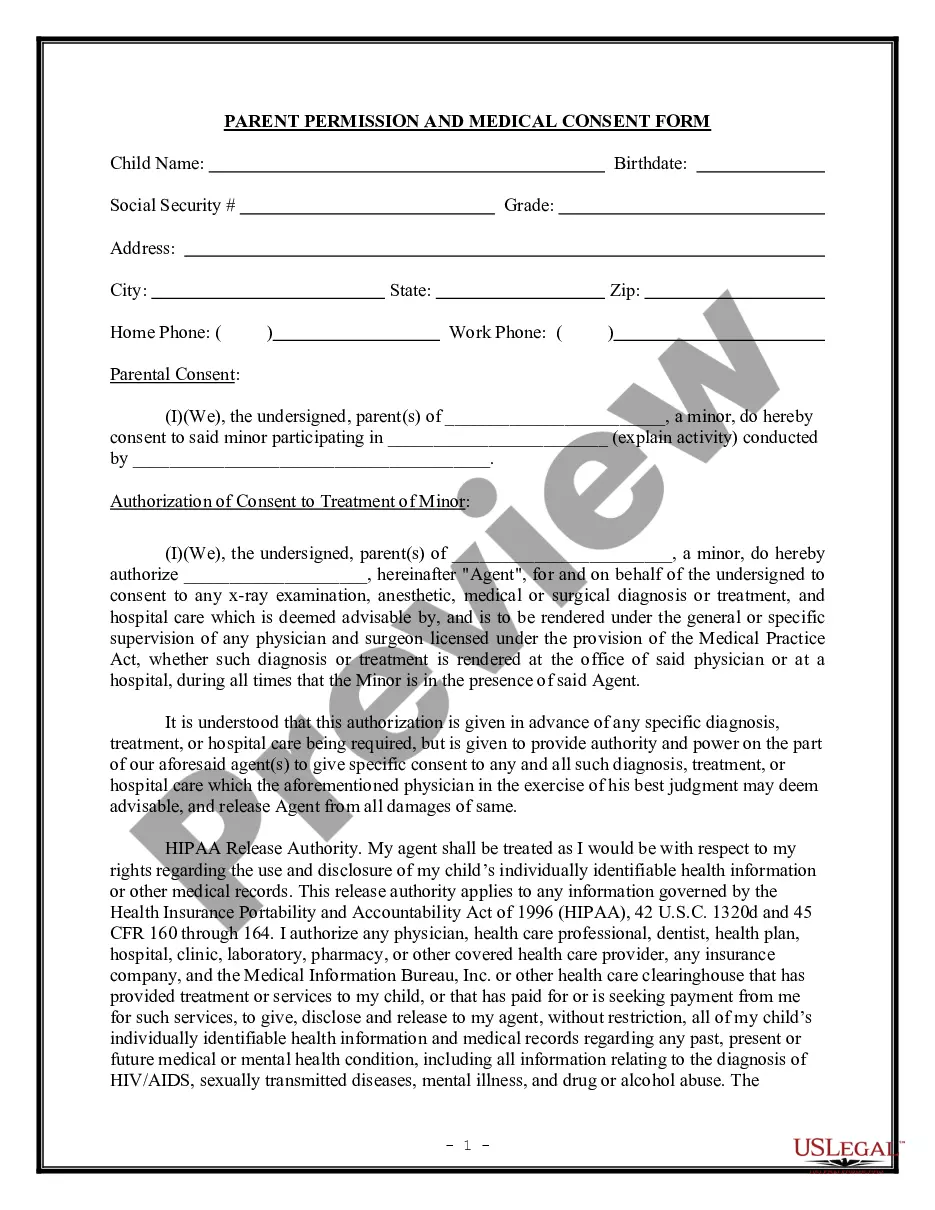
How to fill out Medical Consent For Treatment?
Identifying the appropriate lawful document format can be quite a challenge. Obviously, there are numerous templates accessible online, but how can you obtain the official design you need? Utilize the US Legal Forms website. The service offers a multitude of templates, including the North Carolina Medical Consent for Treatment, which can be used for professional and personal purposes.
All the forms are verified by professionals and comply with state and federal regulations.
If you are already registered, Log In to your account and click the Acquire button to locate the North Carolina Medical Consent for Treatment. Use your account to search for the legal forms you have previously acquired. Go to the My documents section of your account to obtain another copy of the document you require.
Select the document format and download the legal document template to your system. Finally, complete, modify, print, and sign the acquired North Carolina Medical Consent for Treatment. US Legal Forms is the largest repository of legal documents where you can find various document templates. Utilize the service to obtain properly crafted paperwork that adheres to state guidelines.
- First, ensure that you have selected the correct document for your city/state.
- You can review the form using the Review option and read the form details to verify it is the right one for you.
- If the document does not meet your needs, use the Search function to find the appropriate form.
- Once you are confident that the form is accurate, click the Purchase now button to obtain the document.
- Select the pricing plan you prefer and provide the necessary information.
- Create your account and complete your purchase using your PayPal account or Visa or Mastercard.
Form popularity
FAQ
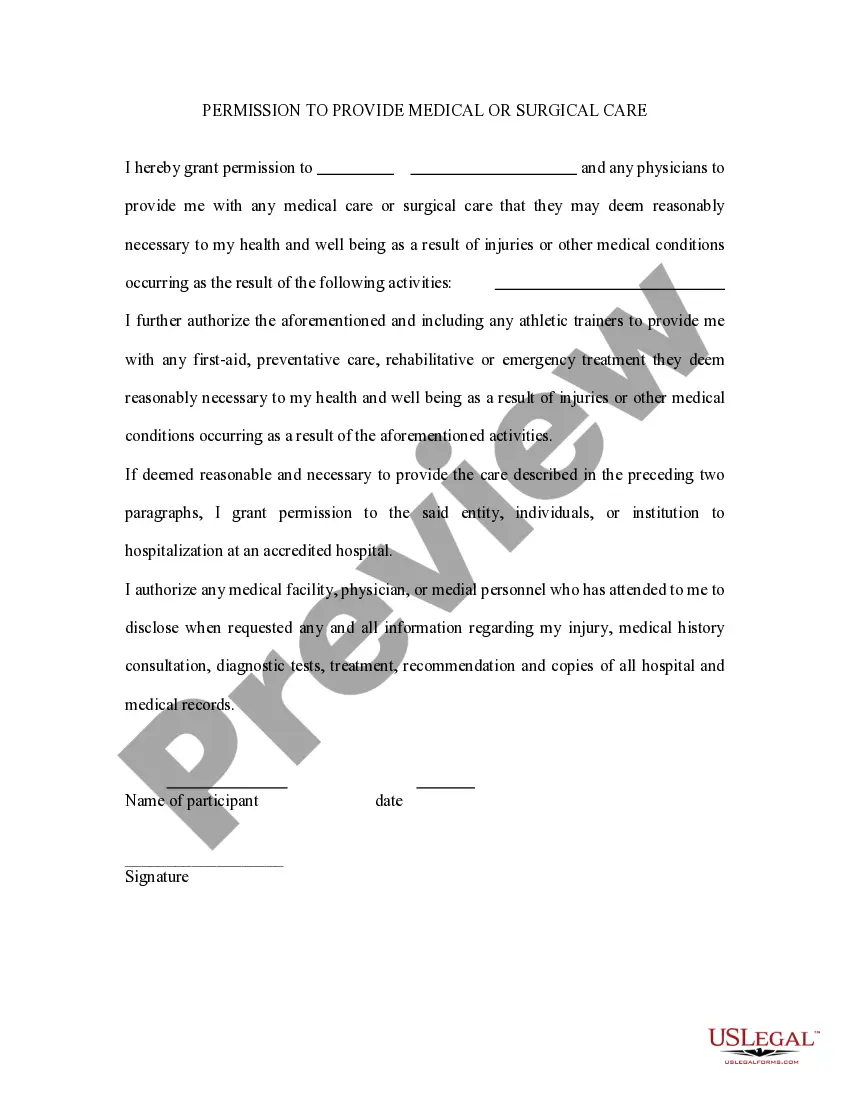
A letter of permission for medical treatment should include your name, the patient's name, and a clear statement granting permission for treatment. Specify the type of treatment and any conditions you wish to include. To simplify this task, consider using US Legal Forms, which provides templates that cater to North Carolina Medical Consent for Treatment requirements, ensuring your letter meets all necessary legal standards.
Writing an authorization letter for medical treatment involves stating your consent for a specific person, such as a family member or medical proxy, to make decisions on your behalf. Clearly detail the nature of the treatment and sign the letter to validate it. With US Legal Forms, you can find templates that comply with North Carolina Medical Consent for Treatment, making the process straightforward and legally sound.
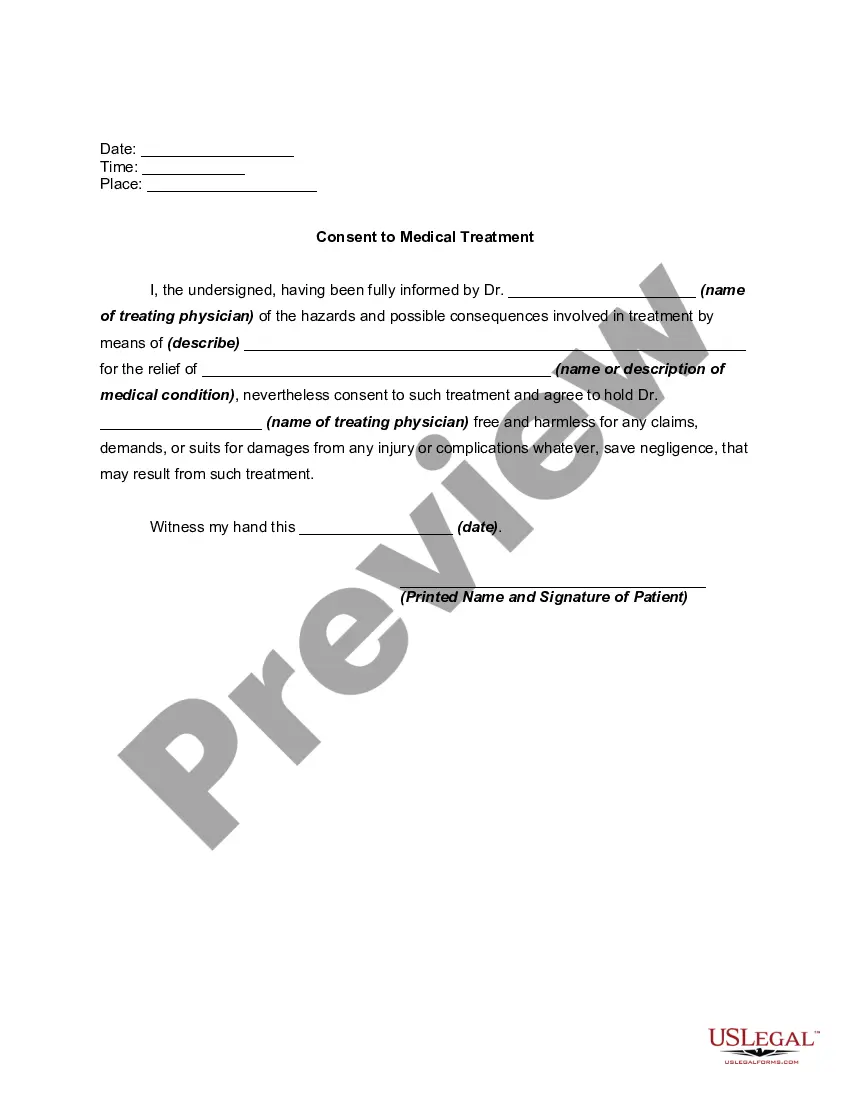
A medical consent letter typically includes your personal information, the healthcare provider’s details, and a clear statement of consent for a specific treatment or procedure. Additionally, the letter should outline any risks involved and your acknowledgment of these risks. If you need assistance, US Legal Forms offers examples and customizable templates for North Carolina Medical Consent for Treatment to ensure you write an effective letter.
To draft a letter of request for medical information or treatment, start by clearly stating your intent and the specific information you need. Include your contact details, and if applicable, mention any relevant medical history. For effective communication, you can utilize tools from US Legal Forms, which provide structured formats compliant with North Carolina Medical Consent for Treatment guidelines.
The informed consent law in North Carolina mandates that healthcare providers must obtain a patient’s consent before administering any treatment. This law requires practitioners to provide comprehensive information about the proposed treatment, including potential risks and benefits. Understanding your rights under North Carolina Medical Consent for Treatment empowers you to engage in informed discussions with your healthcare provider.
In North Carolina, any medical procedure that carries risks, such as surgeries, certain diagnostic tests, or the administration of medications, typically requires a consent to treatment form. This form ensures that you fully understand the procedure, the associated risks, and your choices. By doing so, you can make informed decisions regarding your medical care. North Carolina Medical Consent for Treatment is crucial for safeguarding your rights as a patient.
In North Carolina, generally, both parents must consent for a minor's therapy unless one parent has specific legal rights. If parents are divorced, the custody agreement may dictate consent requirements. For comprehensive understanding, reviewing North Carolina Medical Consent for Treatment guidelines can help clarify these situations.
Legal consent in North Carolina involves obtaining permission from a patient before any treatment is rendered. This consent must be informed, voluntary, and given by a competent individual. Familiarizing yourself with North Carolina Medical Consent for Treatment is essential for both healthcare providers and patients alike.
North Carolina recognizes implied consent in certain situations. This typically applies when a patient voluntarily participates in a medical situation where consent is reasonably expected. If you have inquiries about North Carolina Medical Consent for Treatment, understanding both implied and expressed consent can be beneficial.
Yes, North Carolina requires informed consent for medical treatment. This means that healthcare providers must explain the risks and benefits of a treatment so that patients can make educated decisions. For those exploring North Carolina Medical Consent for Treatment, knowing your rights is crucial.