North Dakota COBRA Notice Timing Delivery Chart
Description
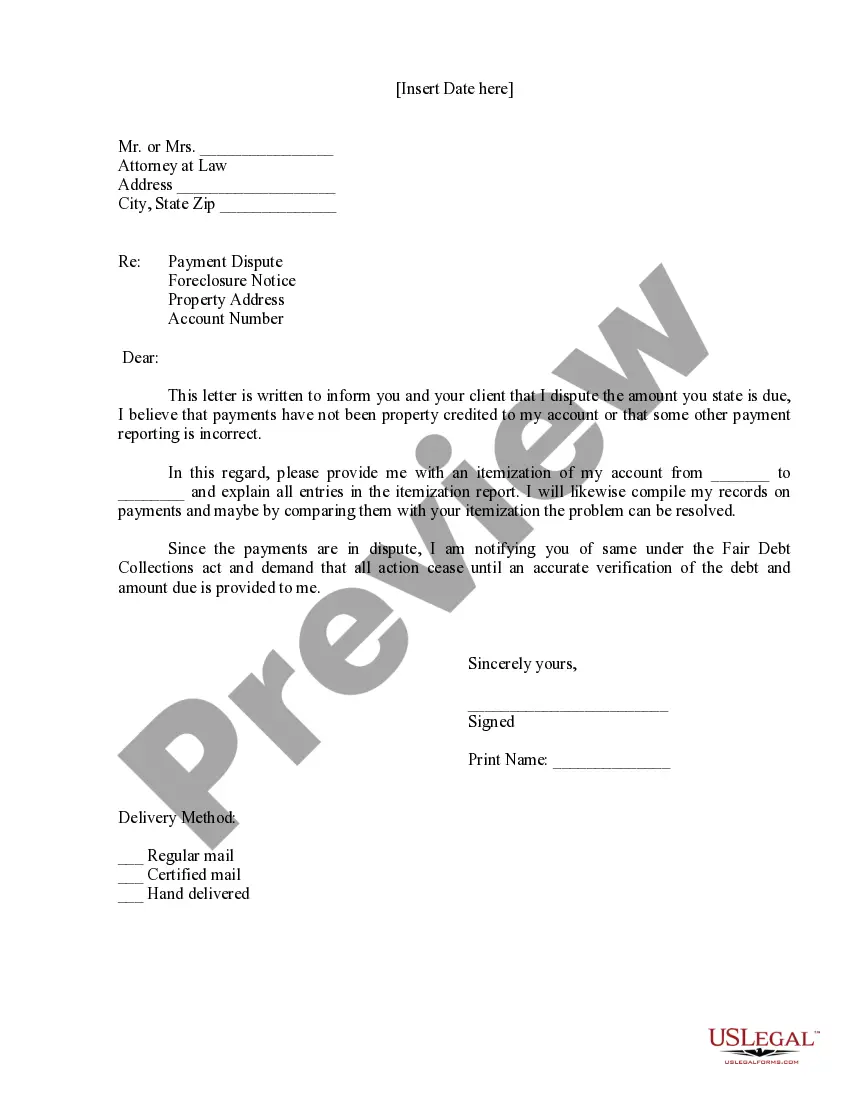
How to fill out COBRA Notice Timing Delivery Chart?
Selecting the appropriate legal document template can be challenging. It goes without saying that there are numerous templates accessible online, but how do you locate the legal format you require? Utilize the US Legal Forms website. This service offers a wealth of templates, such as the North Dakota COBRA Notice Timing Delivery Chart, which you can use for professional and personal purposes. All of the forms are vetted by professionals and comply with federal and state regulations.
If you are already registered, Log In to your account and then click the Download button to retrieve the North Dakota COBRA Notice Timing Delivery Chart. Use your account to check the legal forms you have previously purchased. Visit the My documents section of your account to download another copy of the document you require.
If you are a new user of US Legal Forms, here are simple steps that you should follow.
Choose the file format and download the legal document template to your device. Complete, modify, print, and sign the acquired North Dakota COBRA Notice Timing Delivery Chart. US Legal Forms is the largest repository of legal documents where you can find various template documents. Use the service to obtain professionally crafted papers that adhere to local regulations.
- First, ensure that you have selected the correct document for your city/county.
- You can view the form using the Review button and read the form description to confirm that it is suitable for you.
- If the form does not fulfill your requirements, utilize the Search field to find the appropriate document.
- Once you are certain that the form is accurate, click on the Buy now button to purchase the document.
- Select the pricing plan you prefer and enter the necessary information.
- Create your account and pay for your order using your PayPal account or credit card.
Form popularity
FAQ
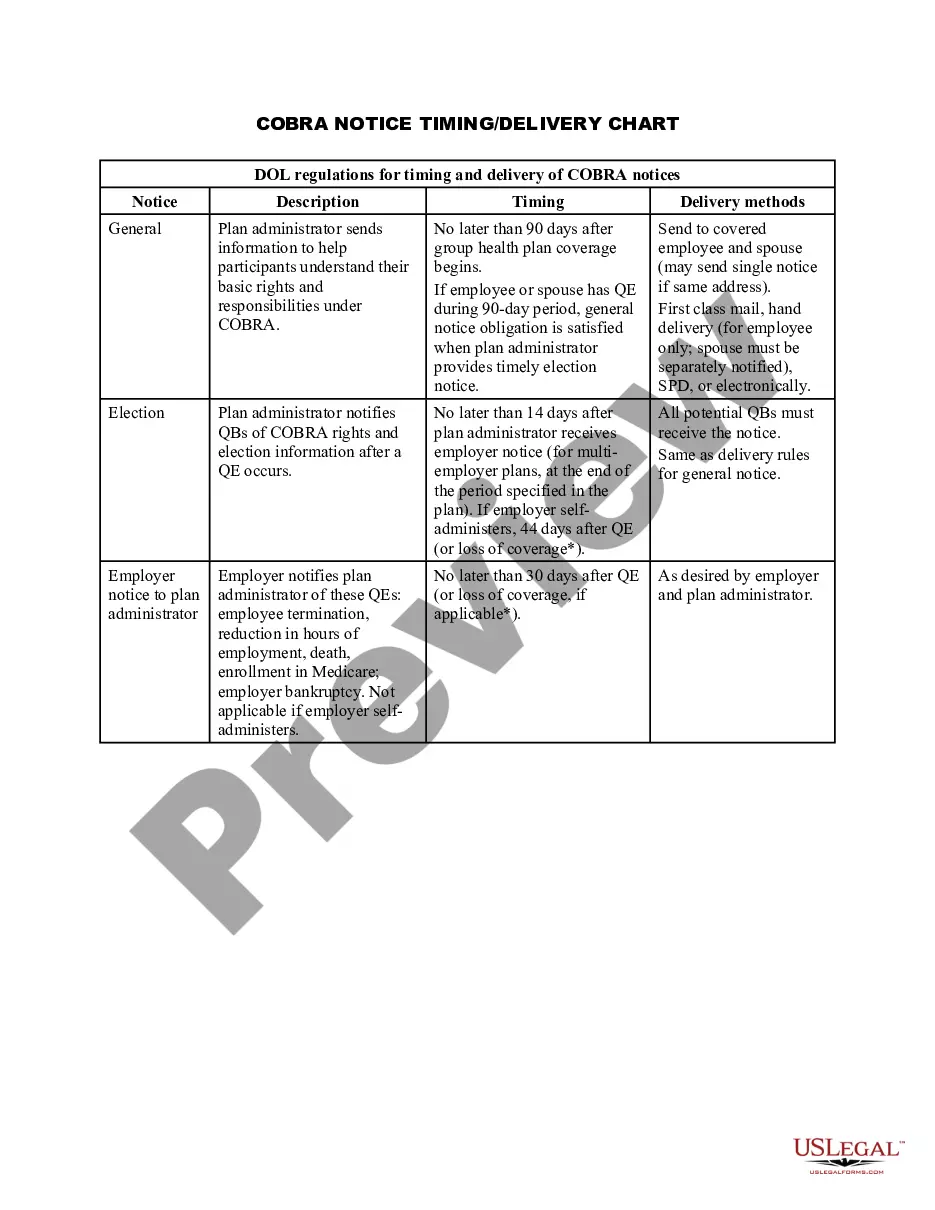
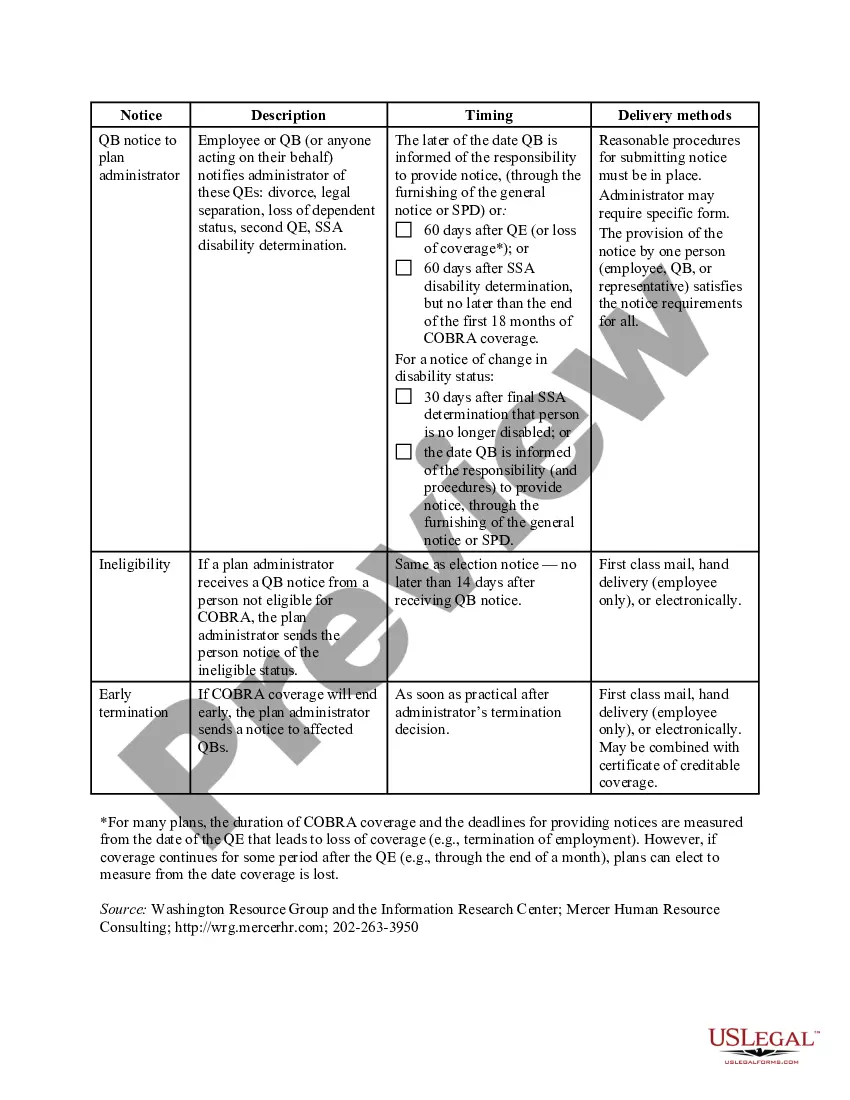
The timing of COBRA notices is crucial for compliance with regulations. Generally, the initial notice must be provided within 90 days of the qualifying event, while the election notice should follow within 14 days after the plan administrator receives notification of the qualifying event. Consult the North Dakota COBRA Notice Timing Delivery Chart for specific timelines related to your situation.
Are there penalties for failing to provide a COBRA notice? Yes, and the penalties can be substantial. Under the Employment Retirement Income Security Act of 1974 (ERISA), a penalty of up to $110 per day may be imposed for failing to provide a COBRA notice.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
COBRA allows a 30-day grace period. If your premium payment is not received within the 30-day grace period, your coverage will automatically be terminated without advance warning. You will receive a termination letter at that time to notify you of a lapse in your coverage due to non-payment of premiums.
Initial COBRA notices must generally be provided within 14 days of the employer notifying the third-party administrator (TPA) of a qualifying event.
Employers who fail to comply with the COBRA requirements can be required to pay a steep price. Failure to provide the COBRA election notice within this time period can subject employers to a penalty of up to $110 per day, as well as the cost of medical expenses incurred by the qualified beneficiary.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
Q11: How long does COBRA coverage last? COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.
COBRA continuation coverage may be terminated if we don't receive timely payment of the premium. What is the grace period for monthly COBRA premiums? After election and initial payment, qualified beneficiaries have a 30-day grace period to make monthly payments (that is, 30 days from the due date).