Title: New Hampshire Qualifying Event Notice Information for Employers to Plan Administrators: Understanding Your Obligations Introduction: In New Hampshire, employers are required to provide timely and accurate information about qualifying events to the plan administrators. This ensures the proper administration of employee benefit plans and allows employees to make informed decisions regarding their benefits. This article will delve into the different types of qualifying events and the essential details employers must include in their notices. 1. Types of Qualifying Events: 1.1 Regular Qualifying Events: Regular qualifying events include marriage, divorce, birth or adoption of a child, loss of dependent status, and gaining or losing eligibility for other group health coverage. 1.2 Special Enrollment Period (SEP) Qualifying Events: Special Enrollment Period qualifying events include loss of existing coverage, exhaustion of COBRA coverage, becoming eligible for state premium assistance, or court-ordered coverage. 2. New Hampshire Qualifying Event Notice Information: When providing notices to plan administrators, employers are required to include the following vital information: 2.1 Employee Information: Include the employee's full name, address, date of birth, and Social Security number. Additionally, provide the employee's job title and department for ease of identification. 2.2 Qualifying Event Description: Provide a clear and concise description of the qualifying event, mentioning whether it's a regular qualifying event or a Special Enrollment Period qualifying event. 2.3 Event Date: Specify the exact date on which the qualifying event occurred. This date is crucial for determining the employee's deadline for making changes to their benefits. 2.4 Dependent Information: Include the full names, dates of birth, and dependent status (marriage, birth, adoption, etc.) of any affected dependents. 2.5 Benefit Options: List the available benefit options for the employee and their dependents. This includes health insurance, dental coverage, vision plans, and any other applicable benefits. 2.6 Enrollment Deadlines: Specify the date by which the employee must enroll or make changes to their benefits due to the qualifying event. Provide clear instructions on how to do so, including any required forms or documentation. 2.7 Contact Information: Include the contact details of the employer's benefits department or designated person responsible for addressing questions and assisting employees with the enrollment process. Conclusion: Complying with New Hampshire's qualifying event notice requirements is crucial for employers to ensure proper administration of benefit plans. By providing accurate and timely information to the plan administrator, employers enable their employees to make informed decisions about their benefits. Remember to be thorough and include all necessary details as outlined above to meet your obligations as an employer in New Hampshire.
New Hampshire Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out New Hampshire Qualifying Event Notice Information For Employer To Plan Administrator?
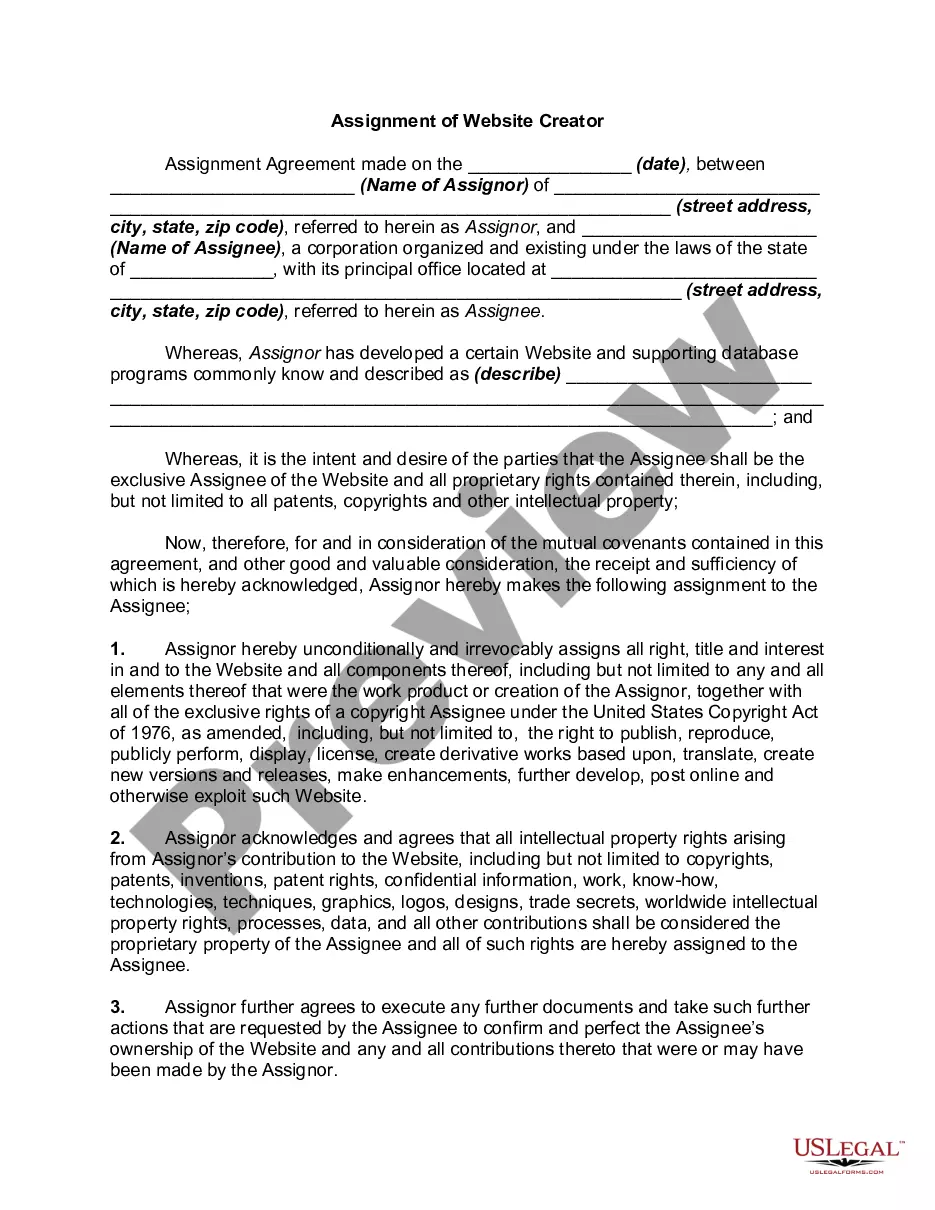
Are you presently in the place where you need papers for both enterprise or specific functions nearly every time? There are a lot of authorized document layouts available on the net, but finding ones you can trust is not effortless. US Legal Forms offers thousands of kind layouts, like the New Hampshire Qualifying Event Notice Information for Employer to Plan Administrator, which are created to meet federal and state requirements.
In case you are currently knowledgeable about US Legal Forms site and have an account, merely log in. Following that, you are able to download the New Hampshire Qualifying Event Notice Information for Employer to Plan Administrator template.
Unless you have an bank account and would like to begin using US Legal Forms, follow these steps:
- Find the kind you need and ensure it is for your appropriate metropolis/state.
- Use the Review option to examine the shape.
- Read the description to actually have chosen the proper kind.
- In the event the kind is not what you are searching for, take advantage of the Look for industry to find the kind that meets your requirements and requirements.
- If you discover the appropriate kind, just click Purchase now.
- Pick the costs program you would like, submit the specified details to make your money, and pay for the order making use of your PayPal or charge card.
- Pick a hassle-free paper formatting and download your duplicate.
Discover every one of the document layouts you may have purchased in the My Forms menus. You may get a additional duplicate of New Hampshire Qualifying Event Notice Information for Employer to Plan Administrator anytime, if possible. Just go through the needed kind to download or print out the document template.
Use US Legal Forms, the most substantial variety of authorized forms, to conserve some time and stay away from blunders. The support offers expertly created authorized document layouts that can be used for a range of functions. Produce an account on US Legal Forms and start making your lifestyle a little easier.
Form popularity
FAQ
For covered employees, the only qualifying event is termination of employment (whether the termination is voluntary or involuntary) including by retirement, or reduction of employment hours. In that case, COBRA lasts for eighteen months.
The COBRA Rights Notification Letter Template contains a model form of the letter that all employees must receive either from their employer or from the benefit plan administrator of their benefit plans.
Such a cool toy! the cobra flyer remote control helicopter flies up to 32ft! snatch it up & watch it go! flies up to 32ft - USB charging cord included - built in gyro specifications.
Federal COBRA & New Hampshire Continuation of Coverage Consolidated Omnibus Budget Reconciliation Act Continuation Coverage (COBRA) is a Federal law that gives employees and their covered dependents, who lose health benefits, the right to continue their coverage, in most cases, a maximum of 18 months.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.