New Hampshire General Notice of Preexisting Condition Exclusion serves as an essential document in the insurance industry, specifically health insurance. This notice is designed to inform policyholders about any preexisting condition exclusions that may apply to their coverage. A preexisting condition refers to any illness or medical condition that existed before the insurance coverage began. Typically, insurance providers may choose to impose an exclusion period for such conditions, during which the policyholder may not receive coverage for any treatment related to their preexisting condition. The purpose of this exclusion is to prevent individuals from obtaining insurance coverage solely to receive treatment for known health issues. The New Hampshire General Notice of Preexisting Condition Exclusion outlines the parameters and limitations regarding preexisting condition exclusions. It ensures that policyholders are aware of these exclusions before purchasing or renewing their insurance policies. The notice specifically provides detailed information about the duration of the exclusion period, which can vary depending on the insurance provider and policy type. Different types of New Hampshire General Notice of Preexisting Condition Exclusions can include: 1. Individual Health Insurance: This pertains to policies purchased by individuals directly from insurance providers, rather than through employer-sponsored group plans. The exclusion details for individual policies may vary, and it is essential for policyholders to carefully review the notice for their specific plan. 2. Group Health Insurance: This applies to insurance plans provided by employers and organizations to their employees or members. The notice provided by these group plans may differ from individual policies due to the unique nature of the plan's coverage and eligibility criteria. 3. Medicare and Medicaid: While these federal programs are not specifically covered by the New Hampshire General Notice of Preexisting Condition Exclusion, they may have their own guidelines and regulations regarding preexisting conditions. Medicare is primarily applicable to individuals over 65 years of age, while Medicaid is targeted towards low-income individuals and families. It's crucial for policyholders to understand the implications of a preexisting condition exclusion before signing up for any insurance plan. This knowledge allows individuals to make informed decisions regarding their healthcare coverage and seek alternative options if necessary. It's recommended to carefully review the New Hampshire General Notice of Preexisting Condition Exclusion alongside the insurance policy's terms and conditions to gain a comprehensive understanding of coverage limitations and exclusions.
New Hampshire General Notice of Preexisting Condition Exclusion
Description
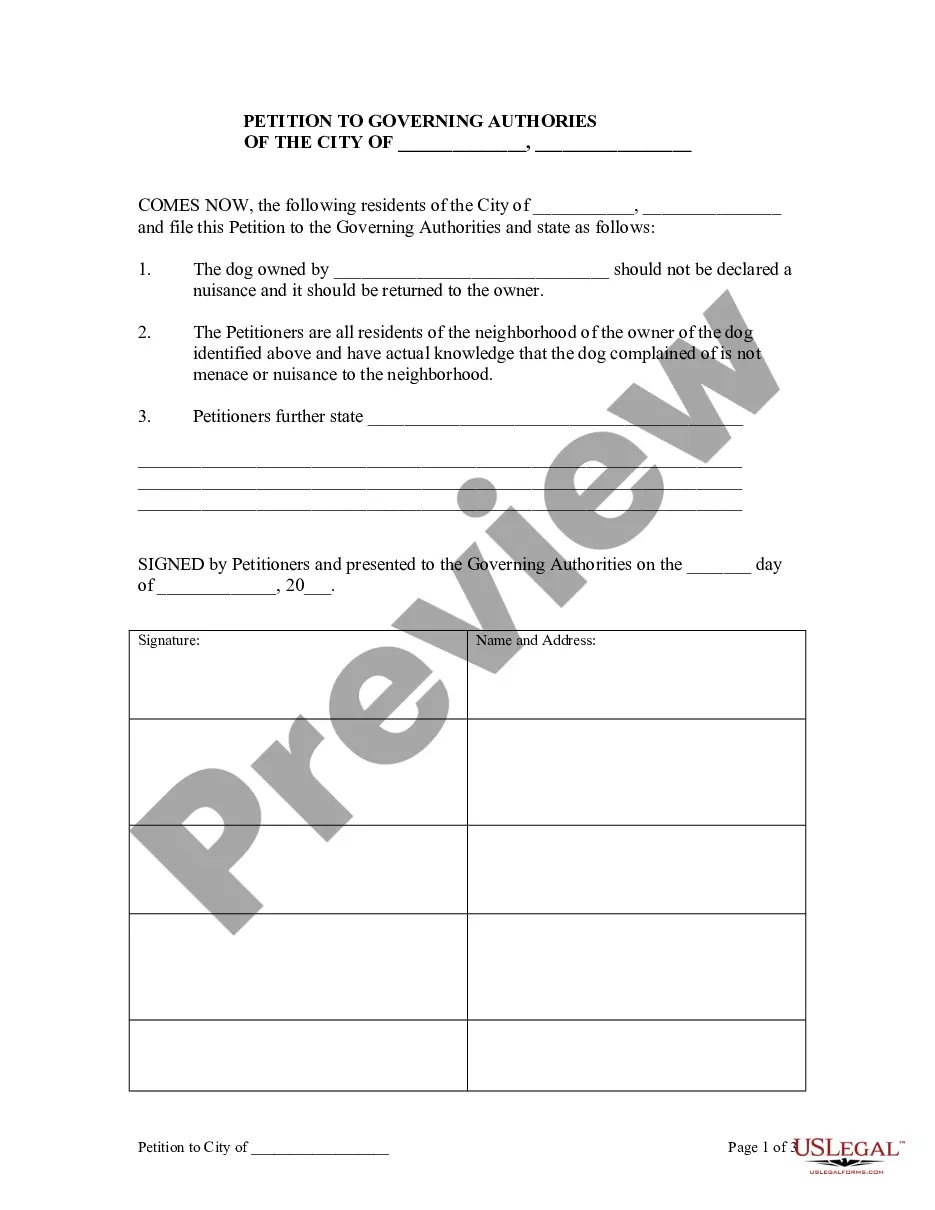
How to fill out New Hampshire General Notice Of Preexisting Condition Exclusion?
Finding the right authorized file format can be a battle. Obviously, there are a variety of web templates available on the Internet, but how do you obtain the authorized kind you need? Make use of the US Legal Forms site. The support gives thousands of web templates, like the New Hampshire General Notice of Preexisting Condition Exclusion, that you can use for company and private needs. All of the varieties are examined by experts and meet state and federal specifications.
If you are previously listed, log in for your bank account and click the Obtain switch to have the New Hampshire General Notice of Preexisting Condition Exclusion. Make use of bank account to check throughout the authorized varieties you may have ordered previously. Check out the My Forms tab of the bank account and acquire an additional version in the file you need.
If you are a fresh user of US Legal Forms, listed here are easy recommendations that you should adhere to:
- Initial, be sure you have selected the right kind for your personal city/area. You are able to examine the form making use of the Review switch and read the form description to ensure this is basically the right one for you.
- In case the kind will not meet your expectations, use the Seach area to get the right kind.
- When you are certain the form would work, go through the Buy now switch to have the kind.
- Select the costs plan you need and type in the needed information. Make your bank account and buy the order making use of your PayPal bank account or Visa or Mastercard.
- Choose the document formatting and down load the authorized file format for your device.
- Total, modify and produce and sign the attained New Hampshire General Notice of Preexisting Condition Exclusion.
US Legal Forms may be the most significant local library of authorized varieties for which you can see different file web templates. Make use of the company to down load appropriately-manufactured paperwork that adhere to state specifications.