New Jersey Notice of Qualifying Event from Employer to Plan Administrator: A Comprehensive Guide Introduction: In New Jersey, employers are required to notify their plan administrators about qualifying events that may affect the eligibility of employees for group health insurance coverage. This notification is crucial to ensure prompt administration of coverage and to keep employees and plan administrators informed about any changes or circumstances that may impact health insurance benefits. This article aims to provide a detailed description of the New Jersey Notice of Qualifying Event from Employer to Plan Administrator, highlighting relevant keywords and the various types of notices that may be involved. 1. Key Details: — New Jersey Notice of Qualifying Event: A formal written communication from employers to plan administrators regarding events that may result in modifications or terminations to an employee's health insurance coverage. — Employer: The organization or company responsible for providing health insurance benefits to its employees. — Plan Administrator: The designated entity responsible for managing and overseeing health insurance plans, including eligibility, enrollment, coverage amendments, and terminations. 2. Purpose: The purpose of the New Jersey Notice of Qualifying Event is to ensure that the plan administrator receives timely information regarding any significant changes in an employee's eligibility status for health insurance coverage. This allows for seamless coordination between the employer, plan administrator, and employee to guarantee uninterrupted coverage and avoid potential gaps in benefits. 3. Types of Qualifying Events: — New Hire: This notice provides information about a newly hired employee who is eligible to enroll in the group health insurance plan. — Termination of Employment: This notice notifies the plan administrator when an employee's employment is terminated, whether voluntarily or involuntarily, resulting in the termination of their health insurance coverage. — Change in Employment Status: If an employee experiences a change in work status (e.g., from full-time to part-time), the employer must submit a notice to reflect this change in eligibility for the health insurance plan. — Family Status Changes: Any qualifying event that affects an employee's dependent or beneficiary status, such as marriage, divorce, birth, adoption, or death, must be communicated to the plan administrator. — COBRA Eligibility: In instances where an employee becomes eligible for COBRA continuation coverage due to qualifying events, the employer must inform the plan administrator, who will subsequently facilitate the continuation of benefits. — Medicare Eligibility: If an employee becomes eligible for Medicare, the employer must report this change to the plan administrator for appropriate adjustments in coverage and benefits coordination. 4. Key Considerations: — Timeliness: The New Jersey Notice of Qualifying Event must be submitted promptly to ensure that the plan administrator can make necessary adjustments or take remedial actions within the stipulated timeframes. — Accuracy: Employers must provide accurate and complete information regarding the qualifying event to facilitate proper administration of the health insurance plan. — Documentation: Employers should maintain records of the notices sent to plan administrators for audit purposes and to demonstrate compliance with state regulations. In conclusion, the New Jersey Notice of Qualifying Event from Employer to Plan Administrator is an essential communication tool. It enables prompt adjustment of health insurance coverage based on various qualifying events. By adhering to the requirements and ensuring accurate and timely notifications, employers can boost employee satisfaction and guarantee a smooth administration process for health insurance benefits.
New Jersey Notice of Qualifying Event from Employer to Plan Administrator
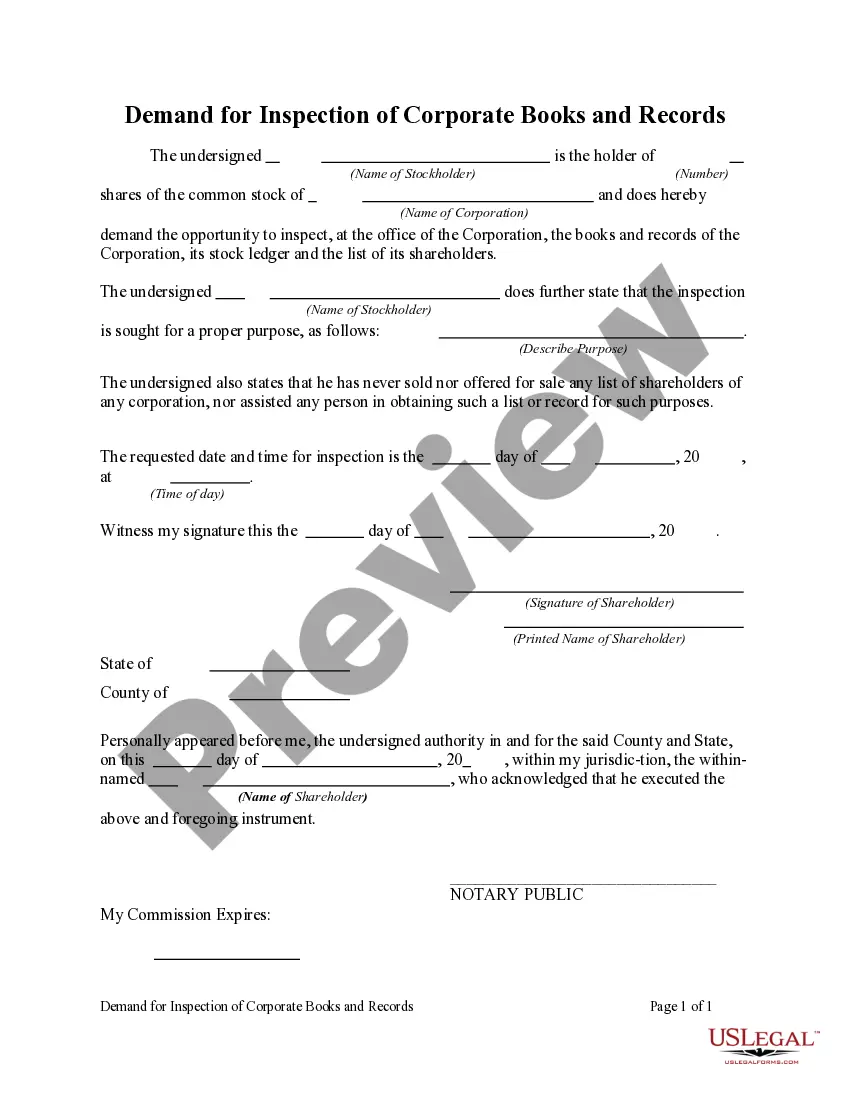
Description
How to fill out New Jersey Notice Of Qualifying Event From Employer To Plan Administrator?
If you have to comprehensive, download, or produce authorized record layouts, use US Legal Forms, the biggest variety of authorized varieties, that can be found on the Internet. Take advantage of the site`s basic and convenient look for to obtain the files you want. Various layouts for company and personal functions are sorted by categories and says, or key phrases. Use US Legal Forms to obtain the New Jersey Notice of Qualifying Event from Employer to Plan Administrator within a number of mouse clicks.
When you are presently a US Legal Forms consumer, log in in your accounts and click on the Download option to get the New Jersey Notice of Qualifying Event from Employer to Plan Administrator. You can also access varieties you earlier delivered electronically within the My Forms tab of your respective accounts.
If you use US Legal Forms for the first time, refer to the instructions beneath:
- Step 1. Make sure you have selected the form for that right town/region.
- Step 2. Take advantage of the Preview solution to look through the form`s information. Do not overlook to see the information.
- Step 3. When you are unsatisfied with the kind, utilize the Lookup area at the top of the display screen to get other variations of your authorized kind template.
- Step 4. After you have identified the form you want, select the Buy now option. Pick the prices plan you choose and put your accreditations to register for an accounts.
- Step 5. Method the transaction. You can use your credit card or PayPal accounts to accomplish the transaction.
- Step 6. Choose the formatting of your authorized kind and download it on the device.
- Step 7. Total, change and produce or indication the New Jersey Notice of Qualifying Event from Employer to Plan Administrator.
Every authorized record template you get is the one you have for a long time. You might have acces to each and every kind you delivered electronically with your acccount. Go through the My Forms segment and decide on a kind to produce or download again.
Remain competitive and download, and produce the New Jersey Notice of Qualifying Event from Employer to Plan Administrator with US Legal Forms. There are millions of skilled and state-certain varieties you can use for your company or personal requires.