New Jersey Qualifying Event Notice Information for Employer to Plan Administrator A New Jersey Qualifying Event Notice is an important document that must be provided by an employer to the plan administrator in certain situations. It serves to inform the plan administrator about any qualifying events that have occurred in the company, which may affect employee benefits and coverage. The Qualifying Event Notice is required by law in New Jersey under the Consolidated Omnibus Budget Reconciliation Act (COBRA) and the New Jersey Continuation of Health Benefits Law (CBL). It ensures that employees and their dependents are aware of their rights and options to continue their health coverage in case of qualifying events such as termination, reduction of hours, divorce, or a dependent child reaching the maximum age limit for coverage. Employers must provide this notice promptly and accurately to the plan administrator to initiate the necessary administrative processes. It contains crucial information regarding the event, including: 1. Employee Information: The notice should provide the employee's name, address, and contact details. It should also include the employee's Social Security number to ensure accurate identification. 2. Qualifying Event Details: The notice needs to clearly state the qualifying event that has occurred. This could be termination of employment, reduction in hours, divorce, legal separation, or the death of the employee. It is crucial to specify the date of the event to determine the effective date of coverage continuation. 3. Dependents Impacted: If the qualifying event affects dependents, the notice should list their names and relationships to the employee. This helps the plan administrator make appropriate arrangements for continuing their coverage. 4. Health Benefit Plan Information: The notice should include details of the health benefit plan through which the employee and dependents were covered. This includes the name of the insurance carrier, the plan number, and any other relevant identifiers. 5. COBRA or CBL Continuation Rights: The New Jersey Qualifying Event Notice should clearly outline the rights and options available to the employee and dependents for continuing health coverage. It should explain the COBRA or CBL continuation process, including deadlines, premium payments, and the duration of coverage. Different types of New Jersey Qualifying Event Notice Information may exist depending on the specific events triggering coverage continuation. Some additional types of qualifying events may include: 1. Eligibility End Date Notice: Given when an employee's eligibility for health coverage is ending due to a reduction in hours or the end of employment. This notice informs the employee about their rights to continue coverage. 2. COBRA Extension Notice: Required when an employee or dependent is already on COBRA coverage and experiences another qualifying event, such as a divorce or a dependent child's loss of dependent status. This notice informs them about their eligibility for an extended COBRA coverage period. 3. Dependent Age Limit Notice: Given when a dependent child covered under the employee's health plan reaches the maximum age limit for coverage. This notice informs the employee about the options available to extend coverage for their child. In summary, New Jersey Qualifying Event Notice Information is crucial for employers to provide accurate details of qualifying events to the plan administrator. This ensures compliance with state and federal laws and helps employees and dependents understand their rights and options for continuing health coverage.
New Jersey Qualifying Event Notice Information for Employer to Plan Administrator
Description
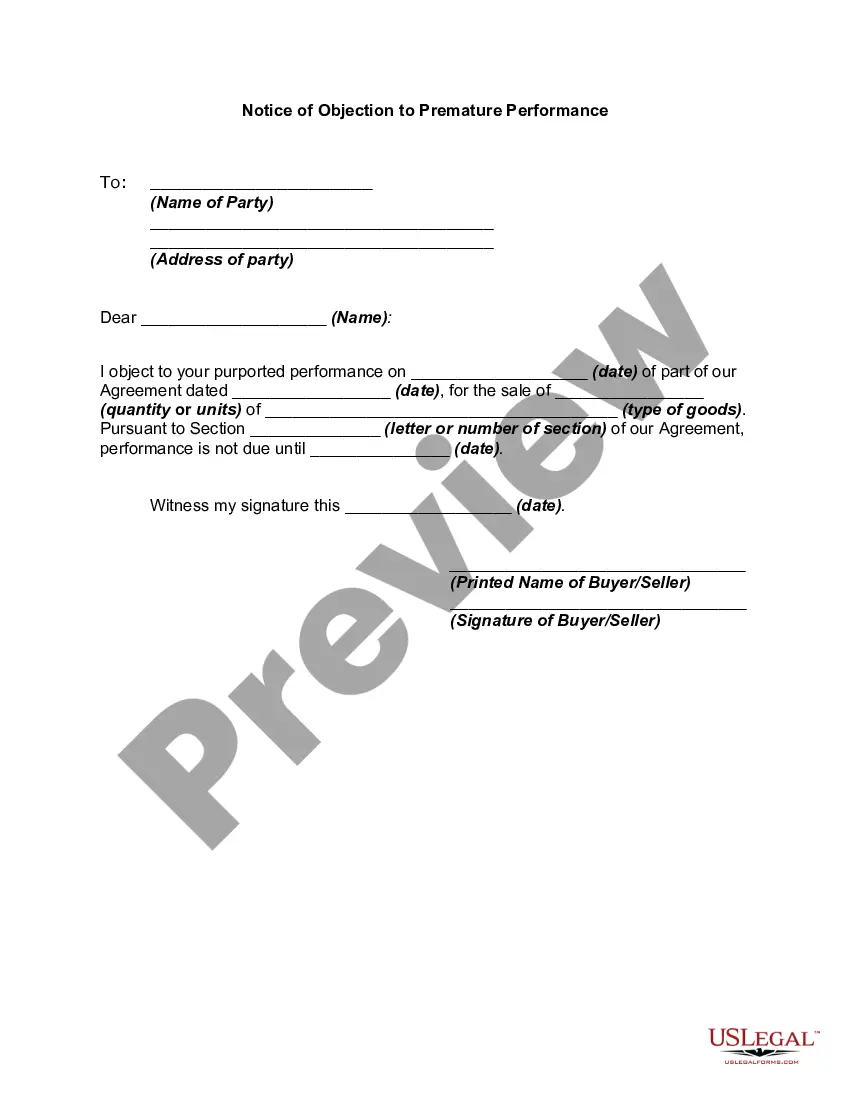
How to fill out New Jersey Qualifying Event Notice Information For Employer To Plan Administrator?
It is possible to commit several hours on the web attempting to find the authorized record format that meets the state and federal requirements you require. US Legal Forms gives a large number of authorized forms which are examined by specialists. It is possible to obtain or printing the New Jersey Qualifying Event Notice Information for Employer to Plan Administrator from the assistance.
If you already have a US Legal Forms profile, it is possible to log in and then click the Acquire button. After that, it is possible to comprehensive, revise, printing, or indicator the New Jersey Qualifying Event Notice Information for Employer to Plan Administrator. Each authorized record format you get is the one you have eternally. To have yet another version associated with a acquired develop, check out the My Forms tab and then click the related button.
If you are using the US Legal Forms site the very first time, follow the simple directions below:
- Initial, make sure that you have selected the correct record format to the county/metropolis of your choice. Look at the develop information to make sure you have picked out the proper develop. If offered, utilize the Preview button to appear from the record format at the same time.
- If you want to discover yet another version of the develop, utilize the Search discipline to get the format that meets your needs and requirements.
- Upon having discovered the format you need, simply click Buy now to carry on.
- Find the rates plan you need, type in your references, and register for a free account on US Legal Forms.
- Comprehensive the financial transaction. You can utilize your Visa or Mastercard or PayPal profile to cover the authorized develop.
- Find the format of the record and obtain it for your system.
- Make modifications for your record if necessary. It is possible to comprehensive, revise and indicator and printing New Jersey Qualifying Event Notice Information for Employer to Plan Administrator.
Acquire and printing a large number of record themes while using US Legal Forms Internet site, that offers the biggest selection of authorized forms. Use skilled and condition-distinct themes to tackle your small business or specific needs.
Form popularity
FAQ
In general: Employers in New Jersey with 50 or more employees must provide minimum essential health care coverage for employees who work 30 or more hours per week or must pay an annual penalty; Businesses in the Garden State with two to 50 employees are not required to offer health care coverage to their employees.
The New Jersey State Health Benefits Program (SHBP) and School Employees' Health Benefits Program (SEHBP) offer employees and their covered dependents the opportunity to join a Direct Primary Care doctor's office at no additional cost.
School Employees' Health Benefits Program Active Group Eligibility. Eligibility for Active Group coverage is determined by the School Employees' Health Benefits Program (SEHBP). All enrollments, changes to coverage, terminations, etc. must go through your employer. Full-time Employees.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
Members enrolled in the State Health Benefits Program (SHBP) or School Employees' Health Benefits Program (SEHBP) can call 1-800-414-SHBP (7427) to access the nurse line and Horizon Health Guide services. Q.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
The federal Consolidated Omnibus Budget Rec- onciliation Act of 1985 (COBRA) requires that most employers sponsoring group health plans offer employees and their eligible dependents also known under COBRA as qualified beneficia- ries the opportunity to temporarily extend their group health coverage in certain
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under