New Mexico Employer - Plan Administrator Notice to Employee of Unavailability of Continuation
Description
How to fill out Employer - Plan Administrator Notice To Employee Of Unavailability Of Continuation?
Are you in a situation the place you will need papers for both company or individual functions virtually every day time? There are a lot of lawful document layouts available online, but locating versions you can trust is not simple. US Legal Forms offers a large number of kind layouts, such as the New Mexico Employer - Plan Administrator Notice to Employee of Unavailability of Continuation, that happen to be published to satisfy federal and state requirements.
If you are currently informed about US Legal Forms web site and get an account, merely log in. Following that, you may down load the New Mexico Employer - Plan Administrator Notice to Employee of Unavailability of Continuation web template.
Should you not offer an bank account and want to begin using US Legal Forms, abide by these steps:
- Find the kind you want and ensure it is to the appropriate city/state.
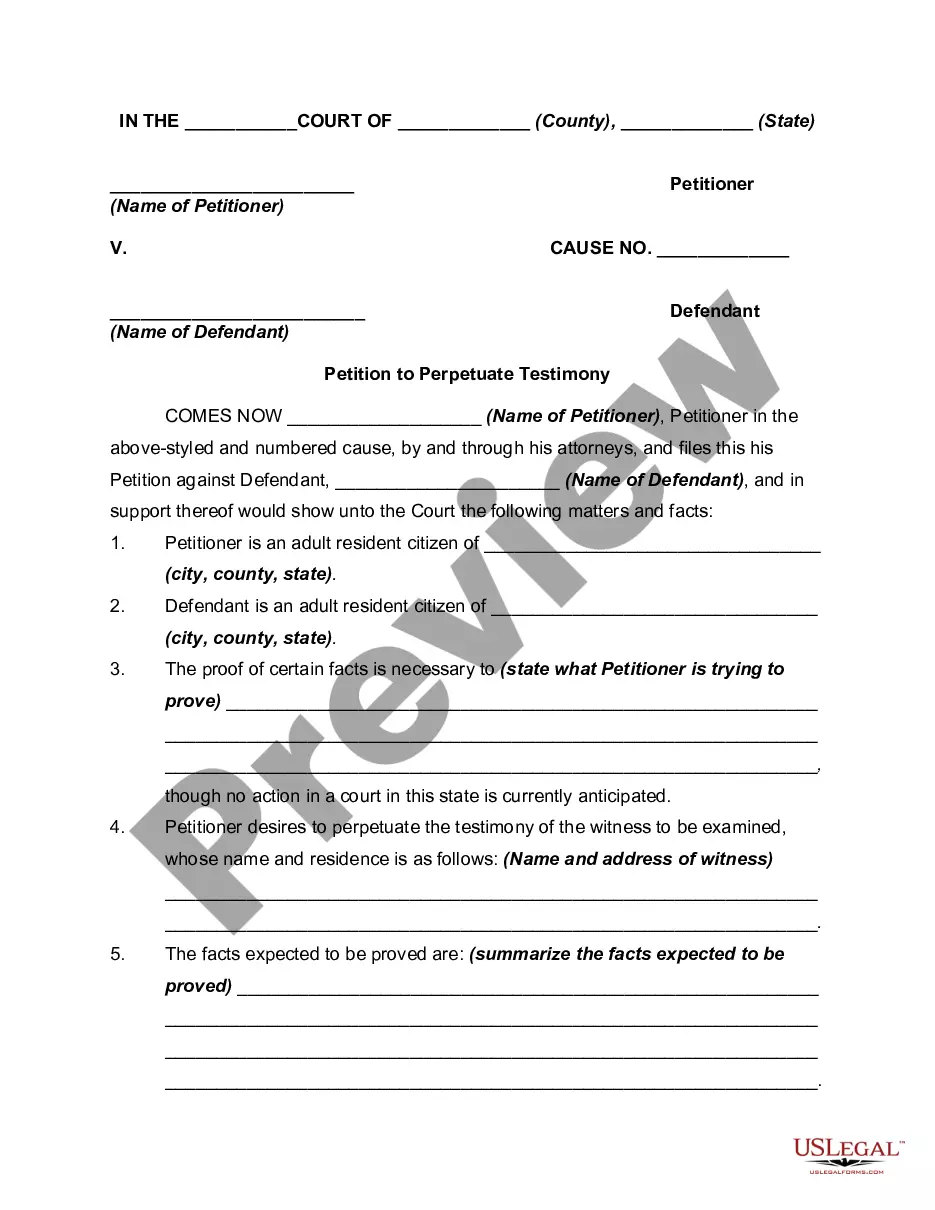
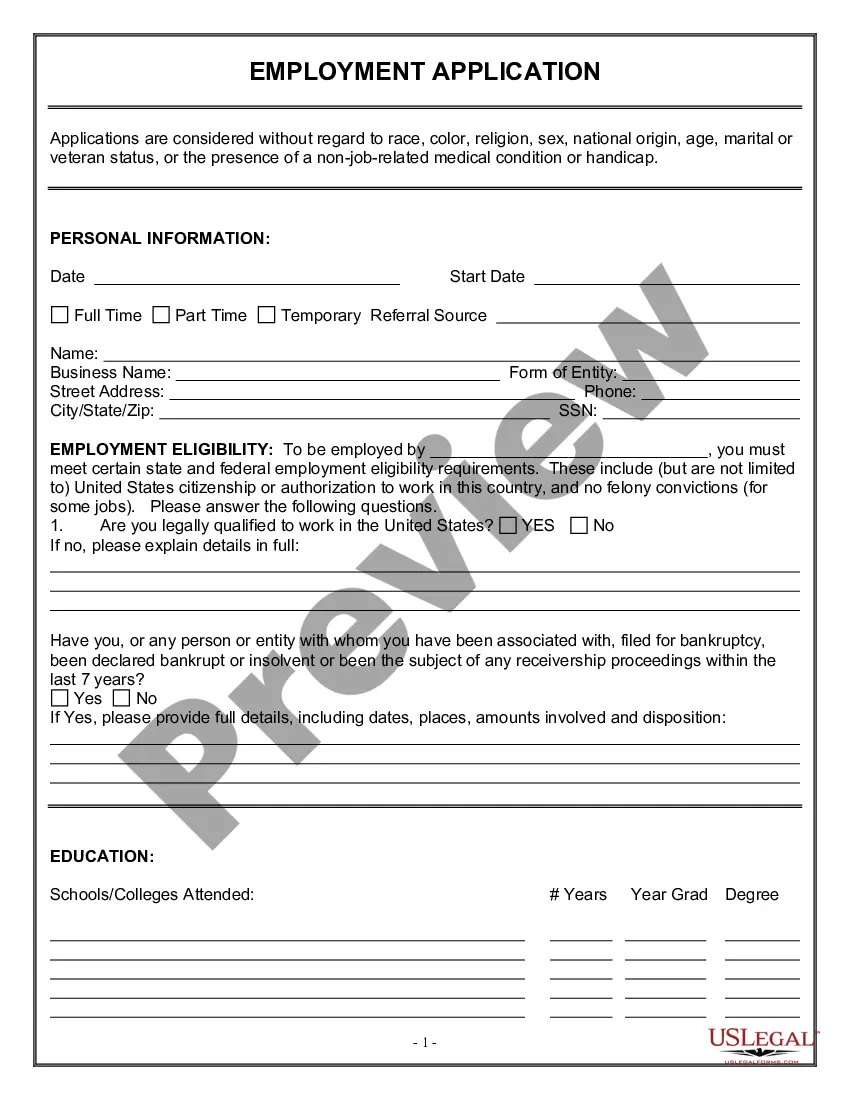
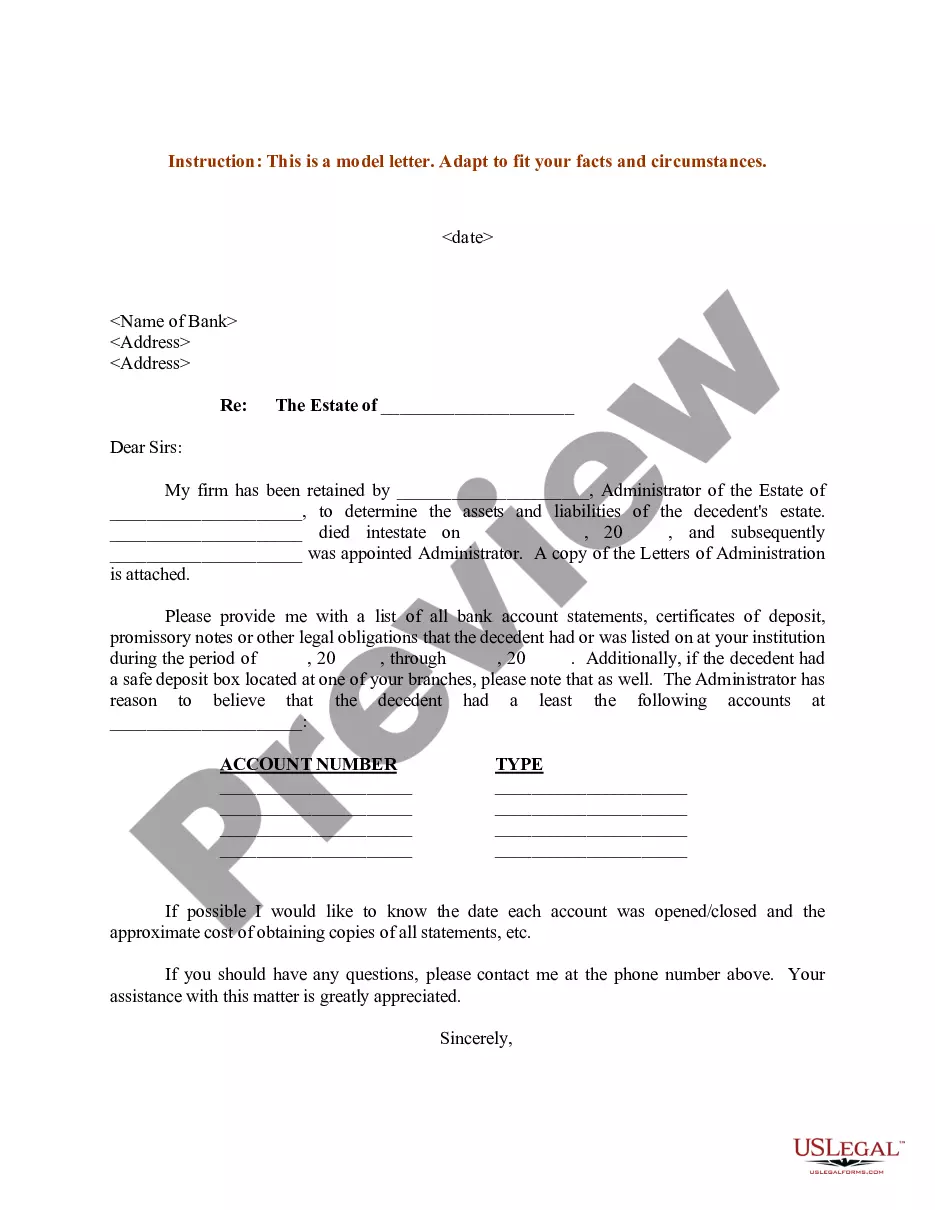
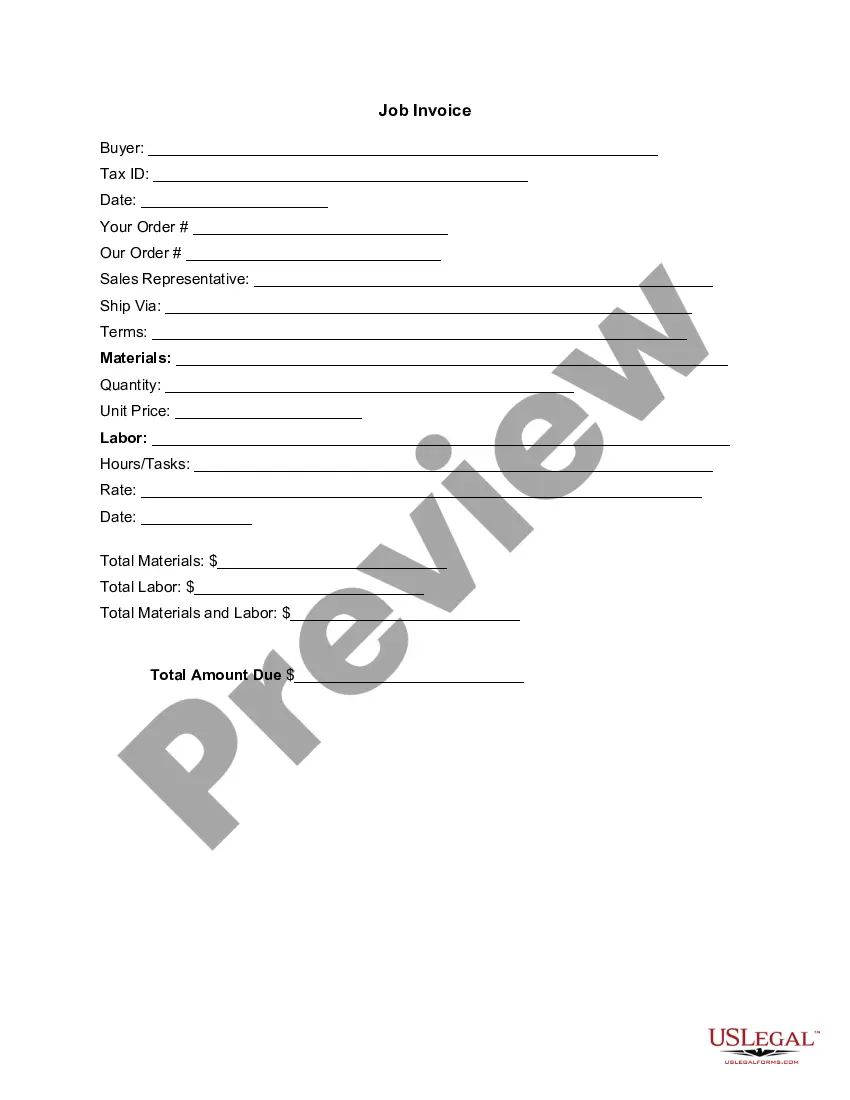
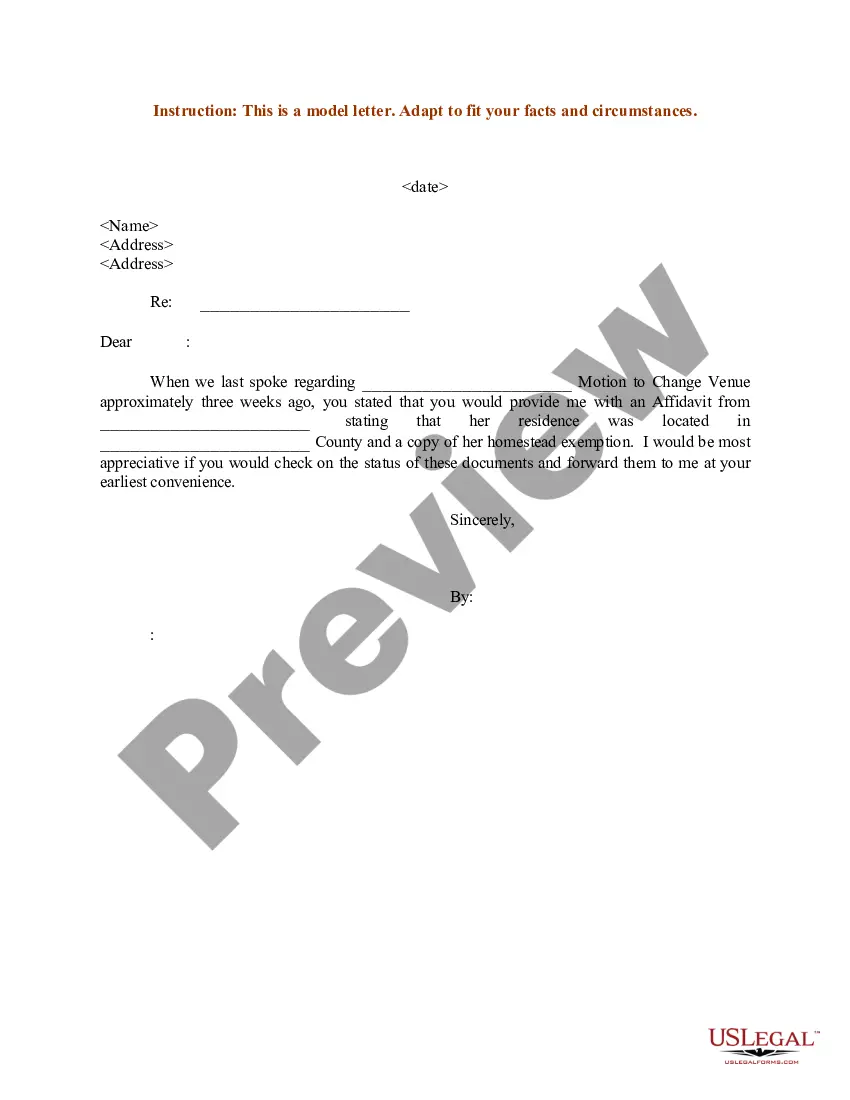
- Take advantage of the Preview key to check the shape.
- Look at the description to ensure that you have selected the appropriate kind.
- If the kind is not what you`re looking for, utilize the Search field to find the kind that meets your requirements and requirements.
- Whenever you find the appropriate kind, just click Get now.
- Select the prices prepare you need, submit the desired info to produce your bank account, and buy the transaction making use of your PayPal or bank card.
- Select a hassle-free document format and down load your duplicate.
Find all of the document layouts you might have purchased in the My Forms food list. You can obtain a more duplicate of New Mexico Employer - Plan Administrator Notice to Employee of Unavailability of Continuation whenever, if possible. Just click the essential kind to down load or produce the document web template.
Use US Legal Forms, by far the most substantial selection of lawful varieties, to save efforts and avoid errors. The services offers expertly made lawful document layouts which can be used for a variety of functions. Generate an account on US Legal Forms and commence creating your life easier.
Form popularity
FAQ
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
Continuation coverage allows someone who recently lost their employer-based health coverage to continue their current insurance policy as long as they pay the full monthly premiums.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Federal COBRA is a federal law that lets you keep your group health plan when your job ends or your hours are cut. Federal COBRA requires continuation coverage be offered to covered employees, their spouses, former spouses, and dependent children.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
Model COBRA notices are provided on the U.S. Department of Labor's COBRA Continuation webpage under the Regulations section.Step 1: Initial Notification.Step 2: Qualifying Event Notices.Step 3: Insurance Carrier Notification.Step 4: Election and Payment.Step 5 (if needed): Late or Missing Payments.More items...
What is Cal-COBRA? Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
Cal-COBRA administration requires four basic compliance components:Notifying all eligible group health care participants of their Cal-COBRA rights.Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.More items...
COBRA is an acronym for the Consolidated Omnibus Budget Reconciliation Act, which provides eligible employees and their dependents the option of continued health insurance coverage when an employee loses their job or experiences a reduction of work hours.