The Nevada General Notice of Preexisting Condition Exclusion is a legal document that outlines the details and provisions related to preexisting condition exclusions in health insurance policies. This notice is required by the Nevada Department of Insurance to be provided to individuals who are eligible for coverage under a health insurance plan. A preexisting condition refers to a health condition or illness that an individual has prior to obtaining health insurance coverage. The General Notice of Preexisting Condition Exclusion aims to inform individuals about the specific provisions related to the coverage of preexisting conditions under their health insurance policy. The notice explains that a preexisting condition exclusion may apply to certain medical conditions or illnesses that an individual had before enrolling in a health insurance plan. This means that the insurance company may choose to exclude coverage for any treatment, services, or medications related to the preexisting condition for a specific period of time. The exclusion period can vary depending on the type of policy. It is essential for individuals to thoroughly read and understand the General Notice of Preexisting Condition Exclusion to ensure they are aware of any limitations or restrictions when it comes to coverage for their preexisting conditions. By being aware of these exclusions, individuals can make informed decisions about their health insurance and seek alternative options if needed. Different types of General Notices of Preexisting Condition Exclusion in Nevada may include: 1. Individual Health Insurance Policy Exclusion: This type of notice outlines the provisions related to preexisting condition exclusions in individual health insurance plans. It explains the specific conditions or illnesses that may be excluded from coverage and the applicable exclusion period. 2. Group Health Insurance Policy Exclusion: This notice provides information about preexisting condition exclusions in group health insurance plans offered by employers or organizations. It details the conditions or illnesses that may be excluded and the duration of the exclusion period. 3. Short-Term Health Insurance Policy Exclusion: For individuals seeking temporary health insurance coverage, this type of notice explains the preexisting condition exclusion provisions that apply to short-term health insurance policies. It clarifies the specific conditions or illnesses that may be excluded and the length of the exclusion period. 4. Medicare Supplement Insurance Policy Exclusion: Medicare supplement insurance policies, also known as Median plans, often come with preexisting condition exclusion clauses. This notice informs individuals about the specific conditions or illnesses that may be excluded from coverage and the duration of the exclusion period for Medicare supplement plans. It is crucial for individuals to review and understand the applicable General Notice of Preexisting Condition Exclusion before enrolling in a health insurance plan. This will allow them to be fully aware of any limitations or exclusions related to their preexisting conditions and make informed decisions about their healthcare coverage.
Nevada General Notice of Preexisting Condition Exclusion
Description
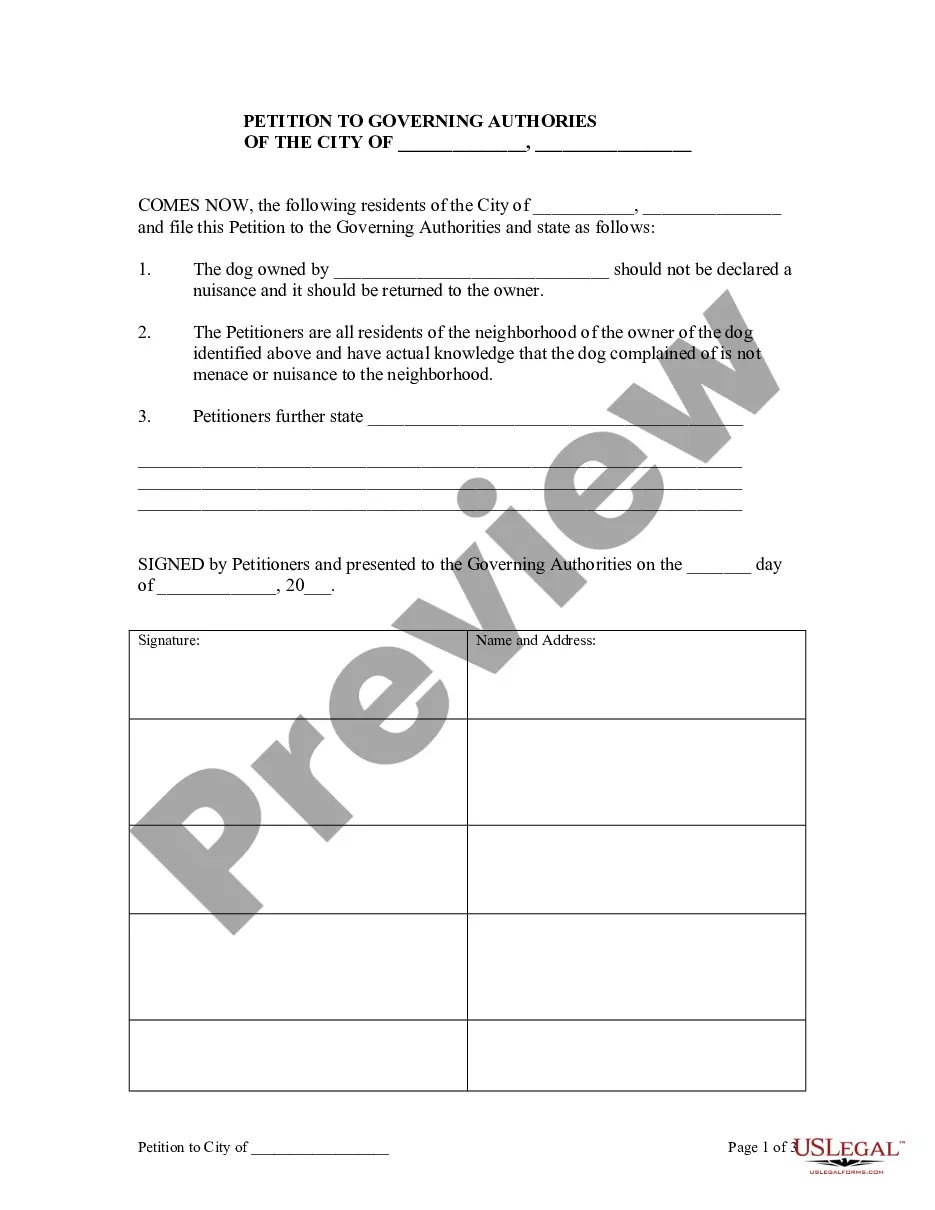
How to fill out Nevada General Notice Of Preexisting Condition Exclusion?
You may commit hrs online looking for the legal document design which fits the federal and state specifications you will need. US Legal Forms gives a huge number of legal varieties that are reviewed by pros. It is simple to acquire or produce the Nevada General Notice of Preexisting Condition Exclusion from my services.
If you currently have a US Legal Forms bank account, you may log in and click on the Down load option. Next, you may comprehensive, change, produce, or indication the Nevada General Notice of Preexisting Condition Exclusion. Each and every legal document design you acquire is the one you have eternally. To get an additional duplicate for any acquired form, visit the My Forms tab and click on the related option.
If you work with the US Legal Forms internet site initially, adhere to the straightforward guidelines listed below:
- Very first, make certain you have chosen the correct document design to the region/town of your choice. Look at the form description to ensure you have picked the right form. If accessible, use the Preview option to appear with the document design also.
- If you wish to get an additional edition of your form, use the Lookup area to obtain the design that fits your needs and specifications.
- When you have identified the design you desire, click Get now to continue.
- Pick the rates prepare you desire, enter your accreditations, and sign up for a free account on US Legal Forms.
- Complete the deal. You should use your bank card or PayPal bank account to cover the legal form.
- Pick the format of your document and acquire it in your gadget.
- Make adjustments in your document if possible. You may comprehensive, change and indication and produce Nevada General Notice of Preexisting Condition Exclusion.
Down load and produce a huge number of document web templates utilizing the US Legal Forms site, which provides the most important assortment of legal varieties. Use professional and status-particular web templates to deal with your small business or individual requires.