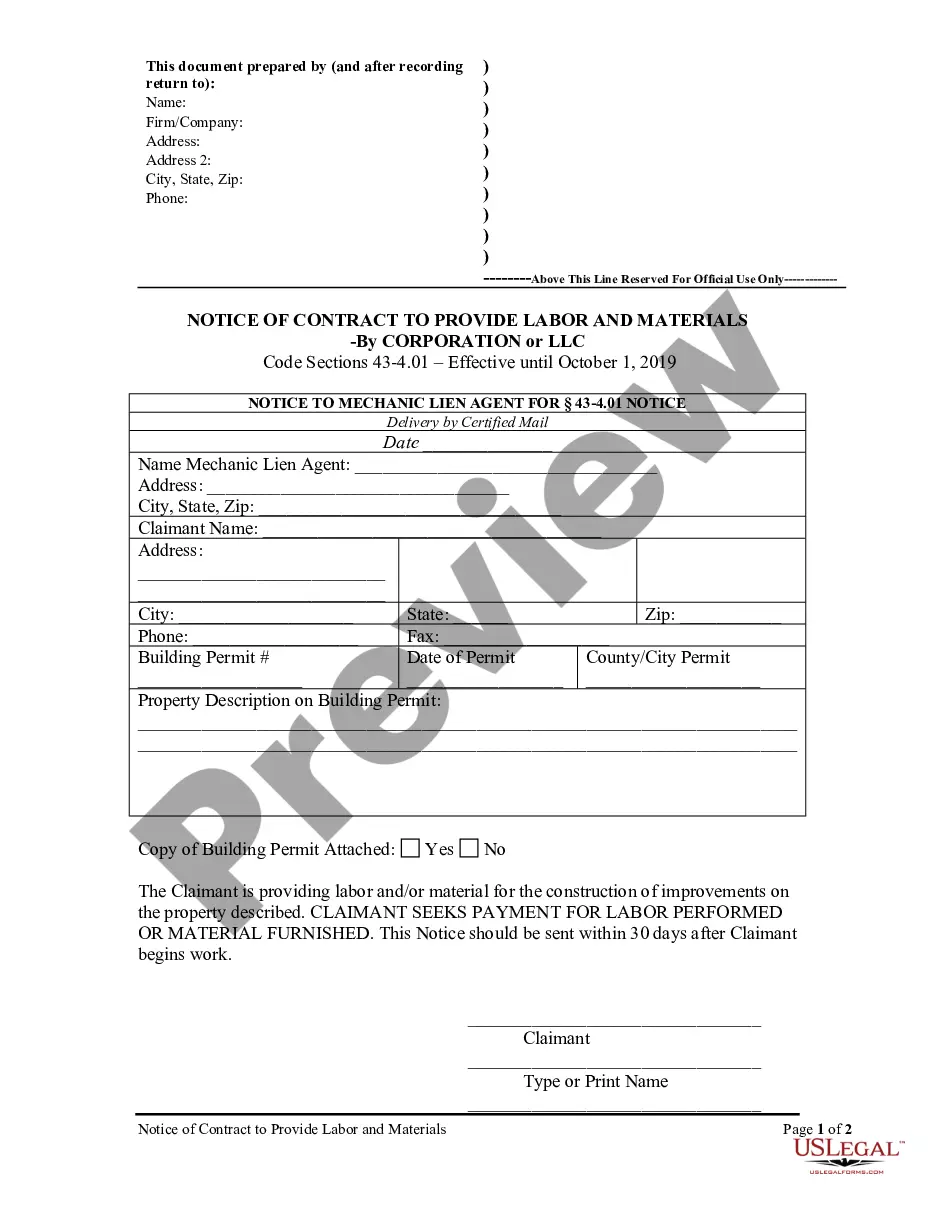
This New York adoption proceeding form, a Notice - Denial or Withdrawal of Application - Removal of Child, is an official New York court model form. Available in Wordperfect or pdf format.
New York Notice - Denial or Withdrawal of Application - Removal of Child
Description
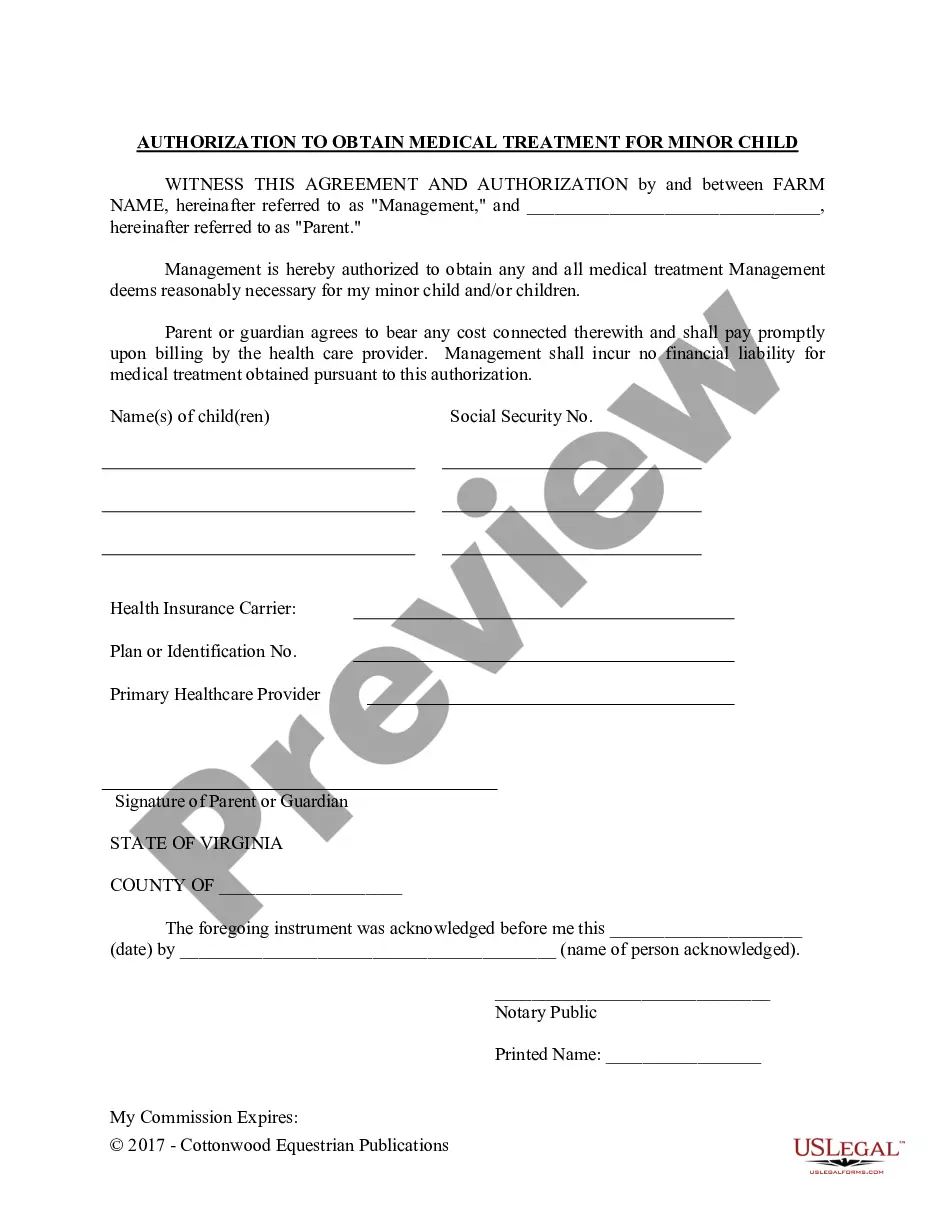
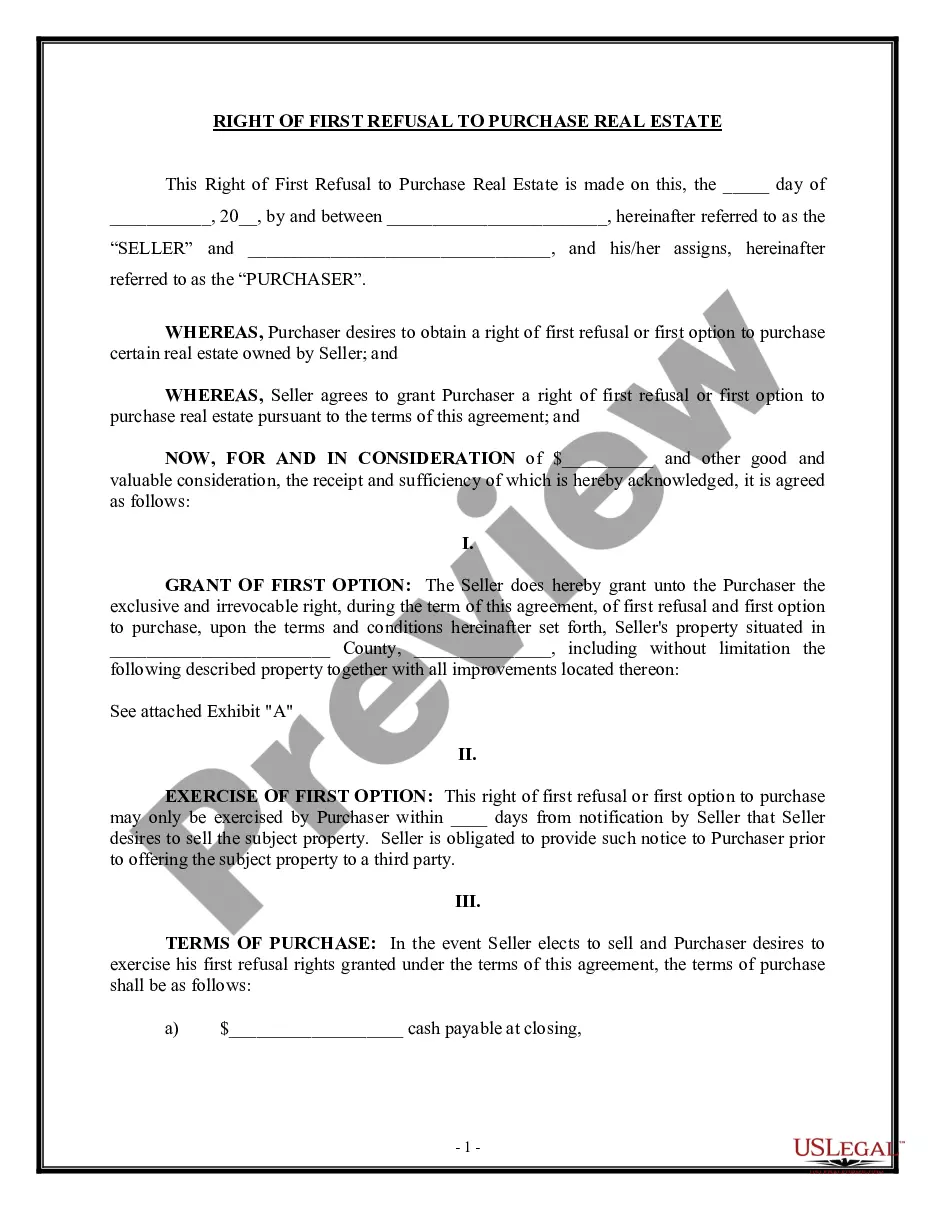
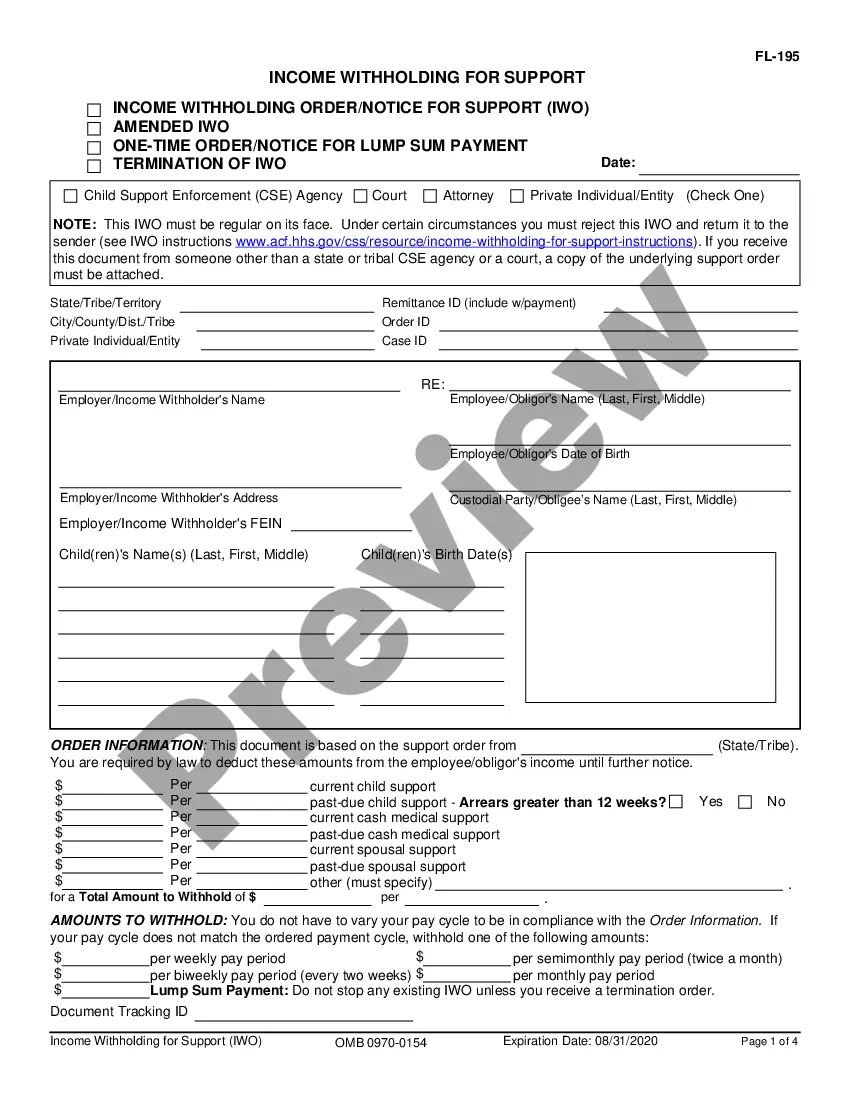
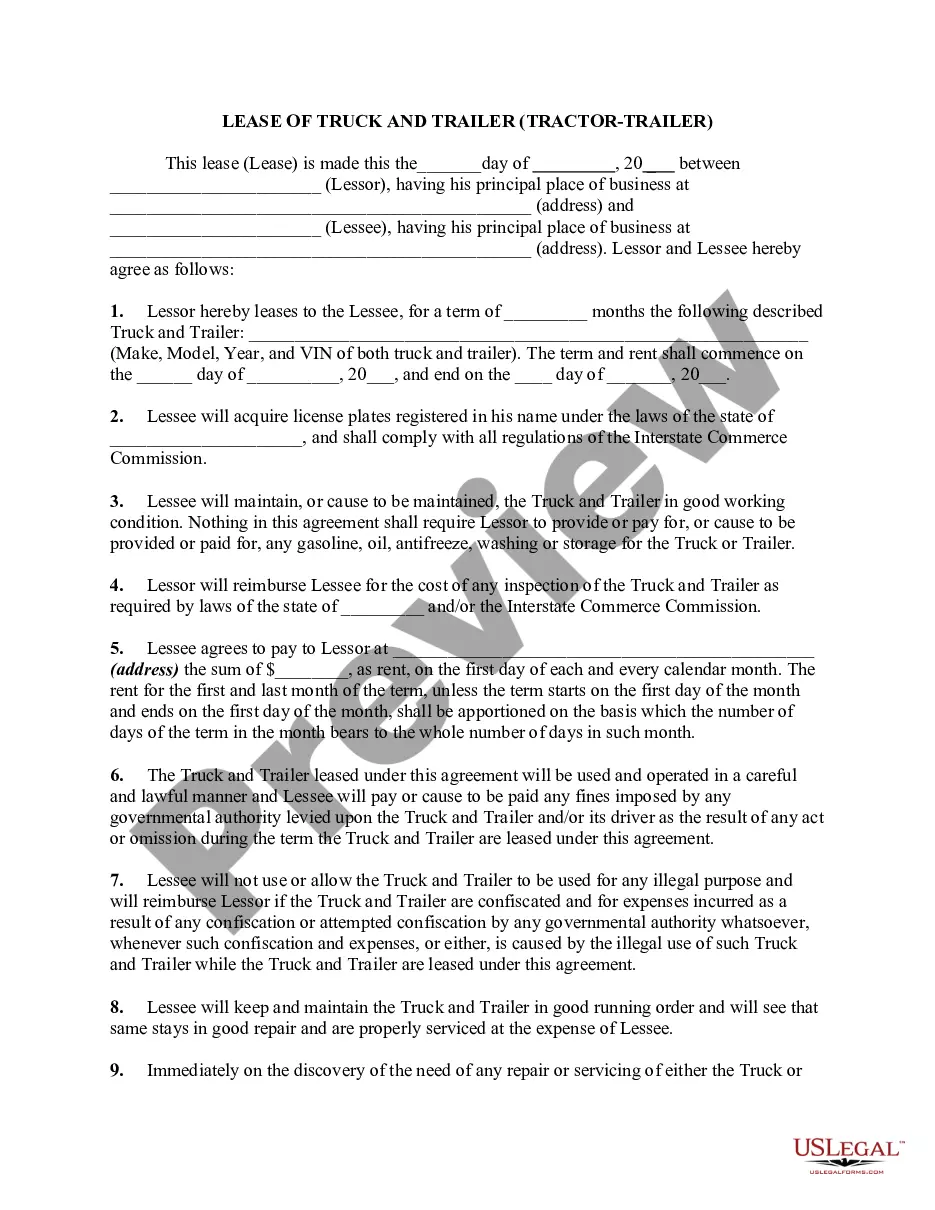
How to fill out New York Notice - Denial Or Withdrawal Of Application - Removal Of Child?
In terms of filling out New York Notice - Denial or Withdrawal of Application - Removal of Child, you most likely think about a long procedure that consists of getting a suitable sample among numerous similar ones and after that needing to pay out a lawyer to fill it out to suit your needs. In general, that’s a slow and expensive option. Use US Legal Forms and choose the state-specific form within just clicks.
For those who have a subscription, just log in and click Download to get the New York Notice - Denial or Withdrawal of Application - Removal of Child sample.
In the event you don’t have an account yet but need one, keep to the step-by-step guideline below:
- Be sure the document you’re downloading applies in your state (or the state it’s needed in).
- Do this by reading the form’s description and also by visiting the Preview function (if readily available) to view the form’s content.
- Click on Buy Now button.
- Choose the appropriate plan for your budget.
- Subscribe to an account and select how you want to pay: by PayPal or by credit card.
- Download the document in .pdf or .docx file format.
- Get the document on the device or in your My Forms folder.
Professional lawyers draw up our samples so that after downloading, you don't have to bother about enhancing content material outside of your personal information or your business’s details. Be a part of US Legal Forms and receive your New York Notice - Denial or Withdrawal of Application - Removal of Child document now.
Form popularity
FAQ
"Adverse Determination" means a determination made by us that a health care service has been reviewed and, based upon the information provided, is not medically necessary or appropriate.
Generally, if you're eligible for Original Medicare (Part A and Part B), you can't be denied enrollment into a Medicare Advantage plan.Your Medicare Advantage plan isn't allowed to make statements such as It is our policy to deny coverage for this service without providing justification.
If Medicaid says you're not eligible for benefits, you can appeal.You might be denied Medicaid because you have too much income or assets or, if you applied for Medicaid on the basis of disability, because your state Medicaid agency did not believe you were disabled.
This notice is called the Medicare Summary Notice (MSN) and is usually issued quarterly. Look for the reason for denial. The notice must state the reason for the denial. Sometimes payment is denied because of a problem with the claim form (e.g., missing information, errors or incorrect codes).
When and how will I be paid my New York State Unemployment? It takes about three to six weeks from the time you file New York unemployment claims to when you receive your first payment due to processing and reviewing of your New York unemployment application.
An adverse benefit determination is a denial, reduction of or a failure to provide or make payment, in whole or in part, for a benefit, including those based on a determination of eligibility, application of utilization review or medical necessity.
If you need to speak to a live customer service representative in New York Department of Labor customer service you need to dial 1-888-209-8124.
Medicare health plans are required to issue the Notice of Denial of Medical Coverage (or Payment), also known as the Integrated Denial Notice (IDN), upon denial, in whole or in part, of an enrollee's request for coverage and upon discontinuation or reduction of a previously authorized course of treatment.
File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim. Circle the item on your MSN that you are appealing and clearly explain why you think Medicare's decision is wrong. You can write on the MSN or attach a separate page.