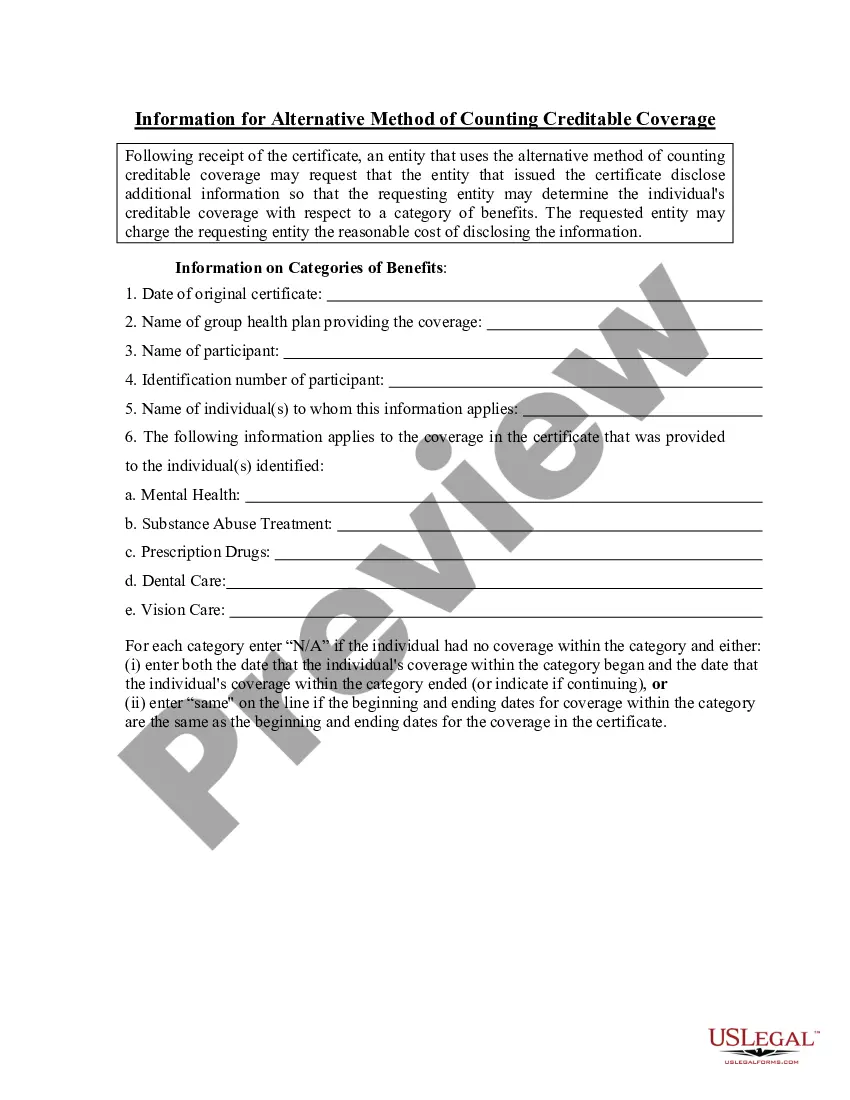
New York Information for Alternative Method of Counting Creditable Coverage
Description
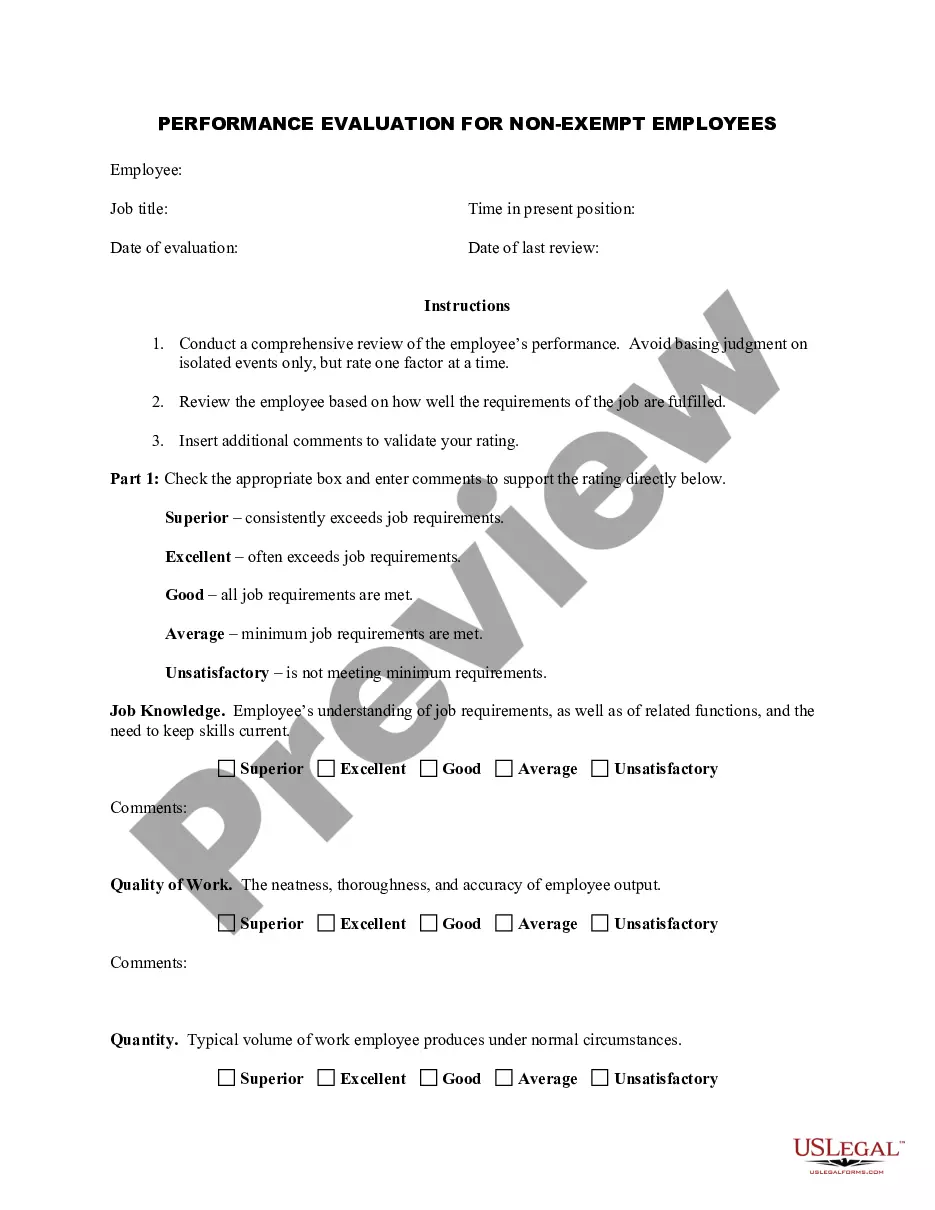
How to fill out Information For Alternative Method Of Counting Creditable Coverage?
If you need to finalize, acquire, or create sanctioned document templates, utilize US Legal Forms, the largest compilation of sanctioned forms available online.
Take advantage of the site's straightforward and efficient search to locate the documents you desire. Various templates for business and personal uses are organized by categories and states, or keywords.
Use US Legal Forms to locate the New York Information for Alternative Method of Counting Creditable Coverage with just a few clicks.
Every legal document template you purchase is yours forever. You have access to each form you downloaded in your account. Click the My documents section and select a form to print or download again.
Complete and obtain, and print the New York Information for Alternative Method of Counting Creditable Coverage with US Legal Forms. There are numerous professional and state-specific forms available for your business or personal needs.
- If you are already a US Legal Forms customer, Log In to your account and click the Acquire button to retrieve the New York Information for Alternative Method of Counting Creditable Coverage.
- You can also access documents you previously downloaded from the My documents tab in your account.
- If you are using US Legal Forms for the first time, follow the steps below.
- Step 1. Ensure you have selected the form appropriate for your city/state.
- Step 2. Use the Preview option to review the content of the form. Remember to read the description.
- Step 3. If you are dissatisfied with the form, use the Search box at the top of the screen to find other documents from the legal form template.
- Step 4. Once you find the form you want, click on the Buy now button. Choose your preferred pricing plan and provide your information to register for an account.
- Step 5. Process the order. You can use your credit card or PayPal account to complete the transaction.
- Step 6. Select the format of the legal form and download it to your device.
- Step 7. Complete, edit, and print or sign the New York Information for Alternative Method of Counting Creditable Coverage.
Form popularity
FAQ
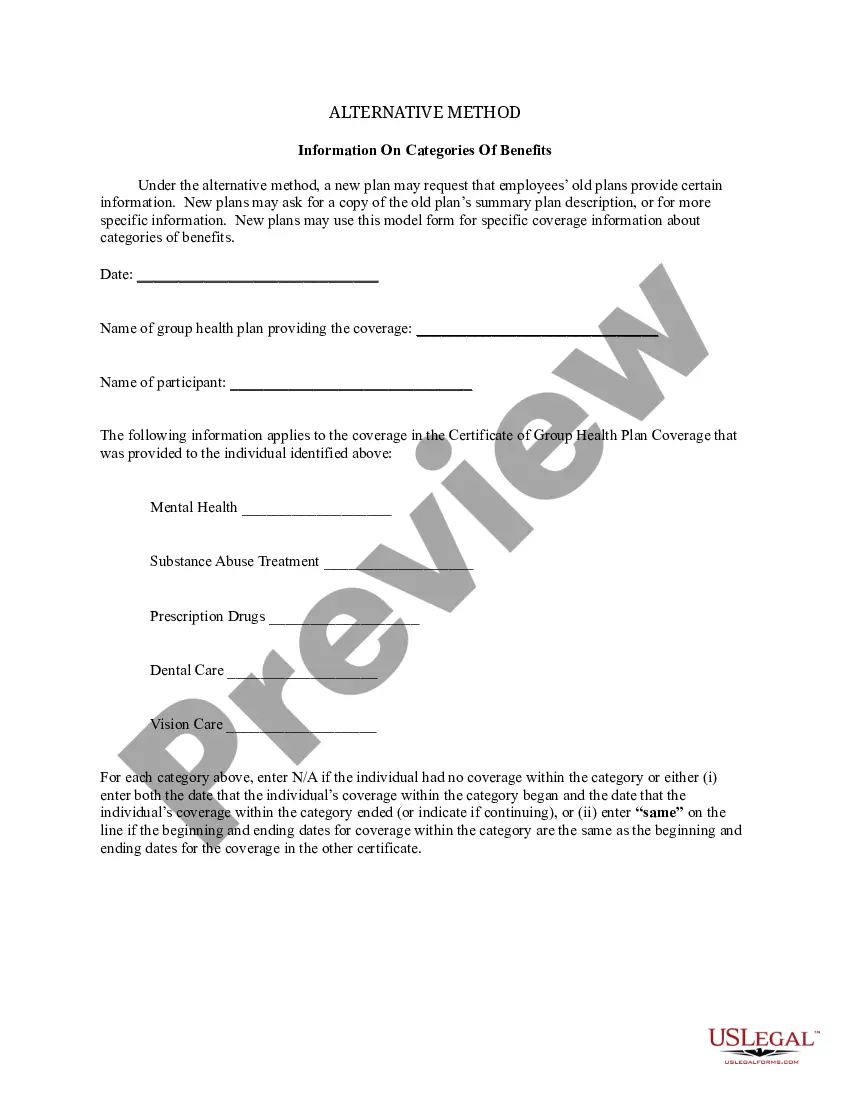
Electronic DeliveryPlan sponsors may send Medicare Part D notices electronically under certain circumstances. CMS has stated that health plan sponsors may follow the electronic disclosure standards under U.S. Department of Labor regulations.
Notices of creditable/non-creditable coverage may be included in annual enrollment materials, sent in separate mailings or delivered electronically.
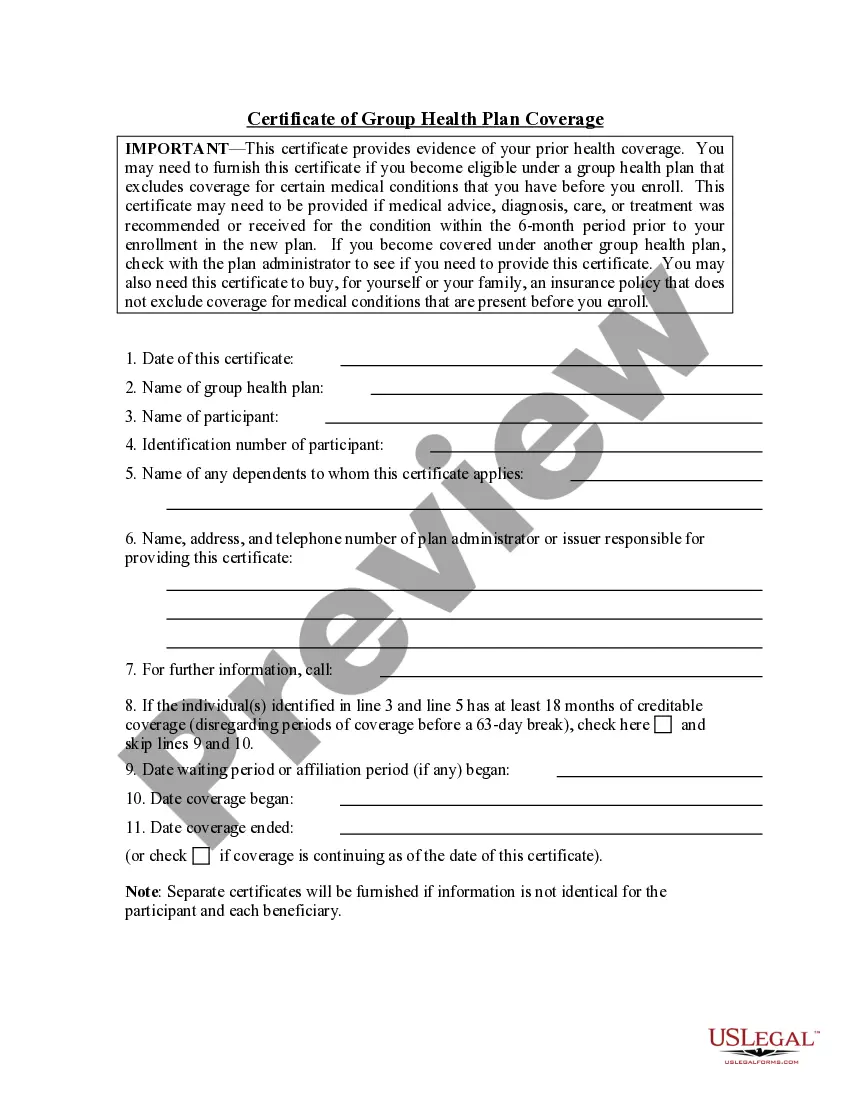
A certificate of Creditable Coverage (COCC) is a document provided by your previous insurance carrier that proves that your insurance has ended. This includes the name of the member to whom it applies as well as the coverage effective date and cancelation date.
Creditable coverage is a health insurance or health benefit plan that meets a minimum set of qualifications. Some examples include group and individual health plans, student health plans, and government-provided plans.
The Notice of Creditable Coverage works as proof of your coverage when you first become eligible for Medicare. Those who have creditable coverage through an employer or union receive a Notice of Creditable Coverage in the mail each year. This notice informs you that your current coverage is creditable.
Employers must provide creditable or non-creditable coverage notice to all Medicare eligible individuals who are covered under, or who apply for, the entity's prescription drug plan (Part D eligibles), whether active employees or retirees, at least once a year.
At a minimum, the CMS creditable coverage disclosure notice must be provided at the following times: Within 60 days after the beginning date of the plan year for which the entity is providing the form; Within 30 days after the termination of the prescription drug plan; and.
Non-creditable coverage: A health plan's prescription drug coverage is non-creditable when the amount the plan expects to pay, on average, for prescription drugs for individuals covered by the plan in the coming year is less than that which standard Medicare prescription drug coverage would be expected to pay.