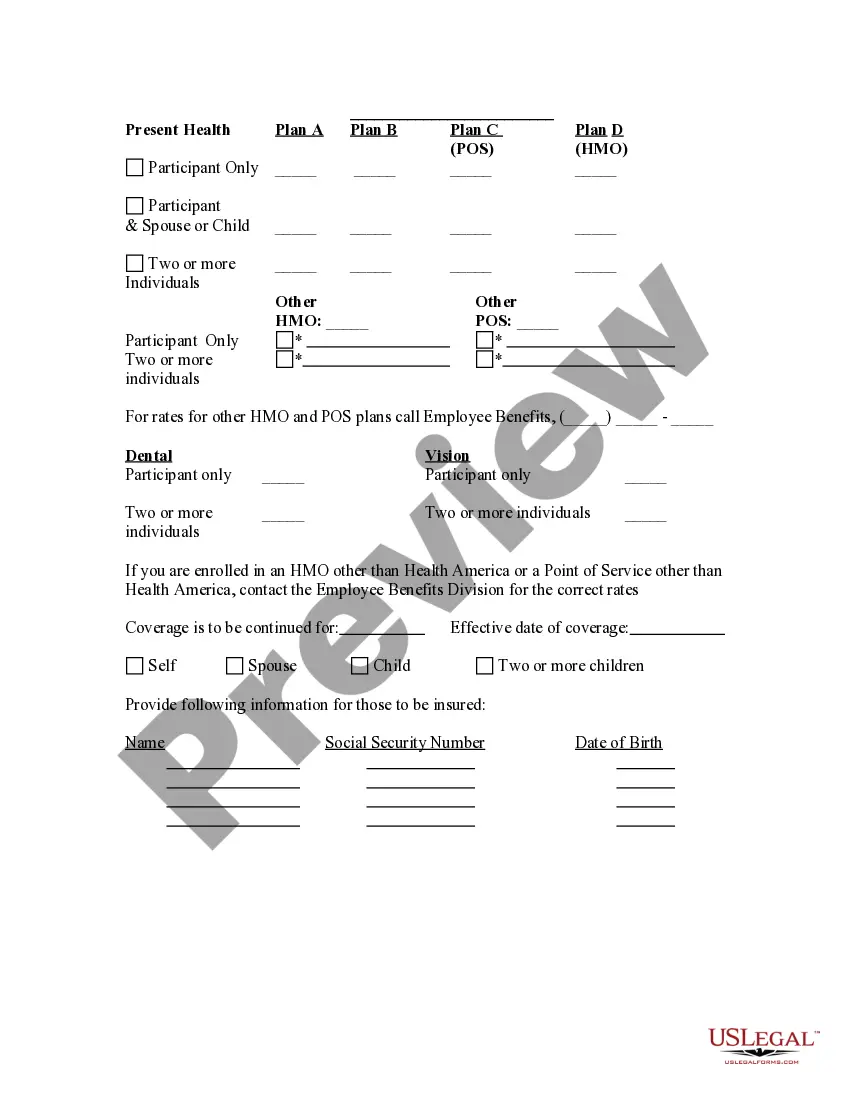
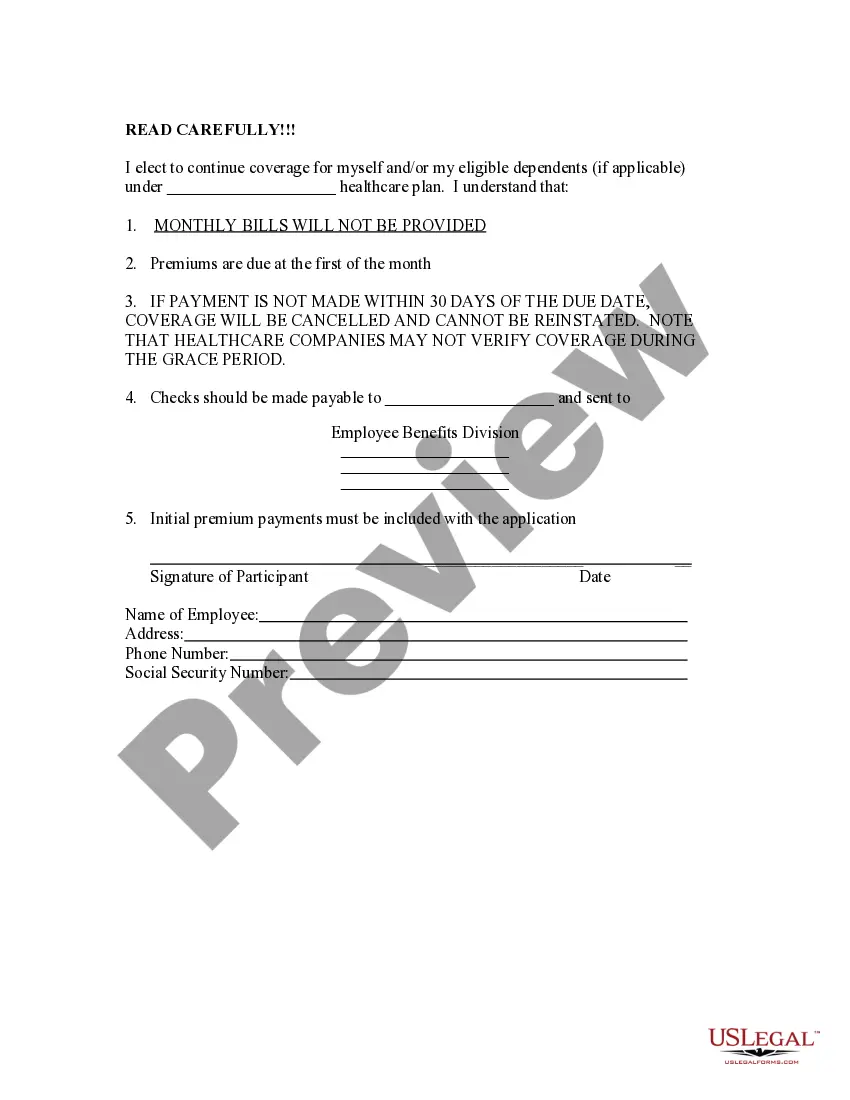
The New York Election Form for Continuation of Benefits — COBRA is a crucial document used in the state of New York to facilitate employee access to continued healthcare coverage. This form is specifically designed to help those individuals who have experienced a qualifying event that would typically result in a loss of healthcare benefits. COBRA, which stands for Consolidated Omnibus Budget Reconciliation Act, provides eligible employees and their dependents the opportunity to temporarily continue their health insurance coverage after the loss of benefits due to certain events such as termination, reduction in working hours, or even divorce or death of the covered employee. There are different types of New York Election Forms for Continuation of Benefits — COBRA that accommodate various qualifying events and situations. Some of these forms include: 1. New York Election Form for Continuation of Benefits after Termination — This form is utilized when an employee's healthcare benefits are terminated due to reasons such as job loss or reduction in working hours. 2. New York Election Form for Continuation of Benefits after Divorce — This specific form is used when an employee's healthcare coverage is lost due to a divorce from the covered employee. 3. New York Election Form for Continuation of Benefits after Death — This form comes into play when the covered employee passes away, resulting in the loss of healthcare coverage for the dependents. 4. New York Election Form for Continuation of Benefits after Reduction in Working Hours — This form is employed in situations where an employee's healthcare coverage is reduced due to a decrease in working hours. 5. New York Election Form for Continuation of Benefits after Loss of Dependent Status — This form is used when an employee's dependent is no longer eligible for coverage, such as when a child reaches the age limit specified by the insurance provider. These individualized New York Election Forms for Continuation of Benefits — COBRA ensure that individuals experiencing specific qualifying events are able to secure the necessary continuation of healthcare coverage for themselves and their eligible dependents. It is crucial for employees to carefully complete these forms with accurate and up-to-date information to avoid any discrepancies or delays in their insurance coverage during this transitional period.
New York Election Form for Continuation of Benefits - COBRA
Description
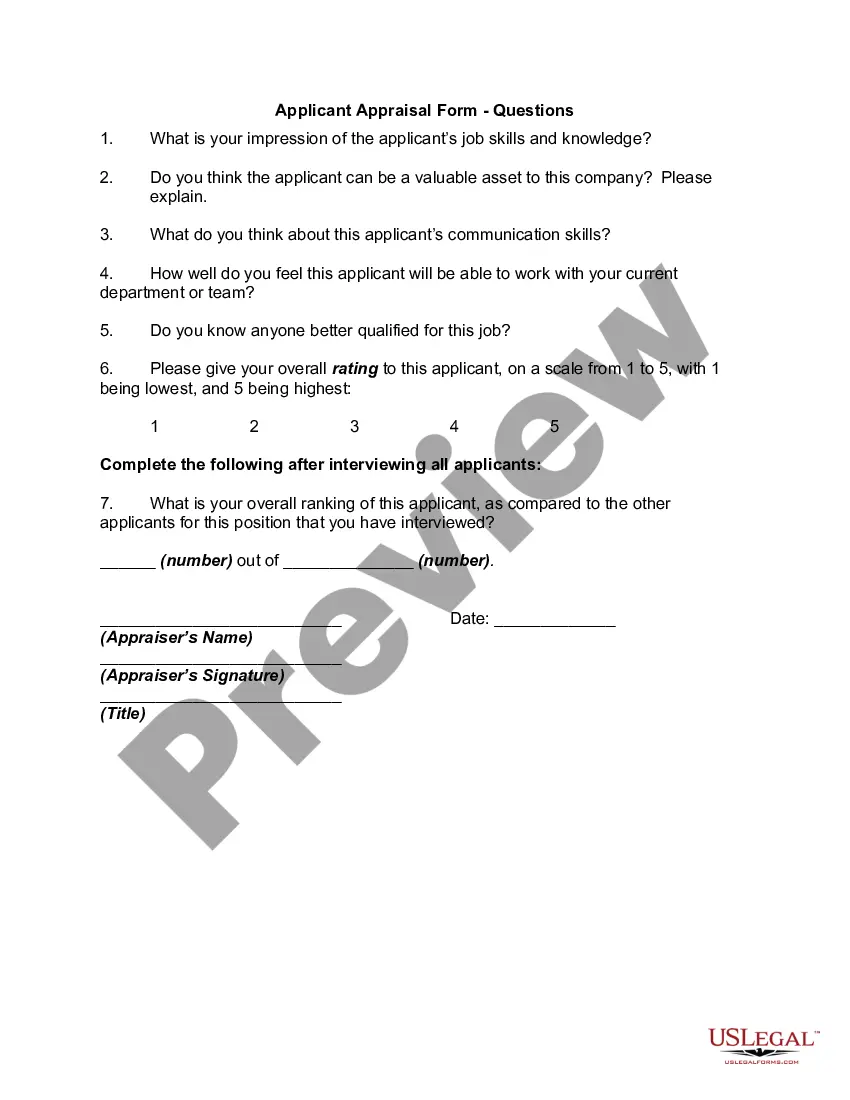
How to fill out New York Election Form For Continuation Of Benefits - COBRA?
Choosing the right authorized record web template could be a have a problem. Obviously, there are tons of templates available on the net, but how would you obtain the authorized kind you require? Utilize the US Legal Forms web site. The assistance gives thousands of templates, including the New York Election Form for Continuation of Benefits - COBRA, that can be used for enterprise and private needs. All of the varieties are checked out by experts and meet up with federal and state specifications.
Should you be already listed, log in for your accounts and then click the Acquire key to obtain the New York Election Form for Continuation of Benefits - COBRA. Make use of accounts to search through the authorized varieties you may have purchased earlier. Proceed to the My Forms tab of your own accounts and obtain an additional copy of your record you require.
Should you be a new end user of US Legal Forms, listed below are easy directions so that you can adhere to:
- Initial, make certain you have selected the appropriate kind for your personal city/state. You are able to check out the shape while using Preview key and look at the shape description to guarantee this is basically the right one for you.
- In the event the kind will not meet up with your expectations, utilize the Seach area to get the appropriate kind.
- When you are positive that the shape is suitable, go through the Acquire now key to obtain the kind.
- Choose the costs program you would like and type in the needed info. Make your accounts and pay for your order making use of your PayPal accounts or credit card.
- Pick the document structure and acquire the authorized record web template for your product.
- Complete, revise and print out and indication the received New York Election Form for Continuation of Benefits - COBRA.
US Legal Forms is the biggest library of authorized varieties where you can find different record templates. Utilize the service to acquire skillfully-manufactured documents that adhere to status specifications.
Form popularity
FAQ
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
COBRA continuation coverage lets you stay on your employer's group health insurance plan after leaving your job. COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. It's shorthand for the law change that required employers to extend temporary group health insurance to departing employees.
Qualified beneficiaries must be given an election period of at least 60 days during which each qualified beneficiary may choose whether to elect COBRA coverage. This period is measured from the later of the date of the qualifying event or the date the COBRA election notice is provided.
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
New York State law requires small employers (less than 20 employees) to provide the equivalent of COBRA benefits. You are entitled to 36 months of continued health coverage at a monthly cost to you of 102% of the actual cost to the employer which may be different from the amount deducted from your paychecks.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.