New York Employer - Plan Administrator Notice to Employee of Unavailability of Continuation
Description
How to fill out Employer - Plan Administrator Notice To Employee Of Unavailability Of Continuation?
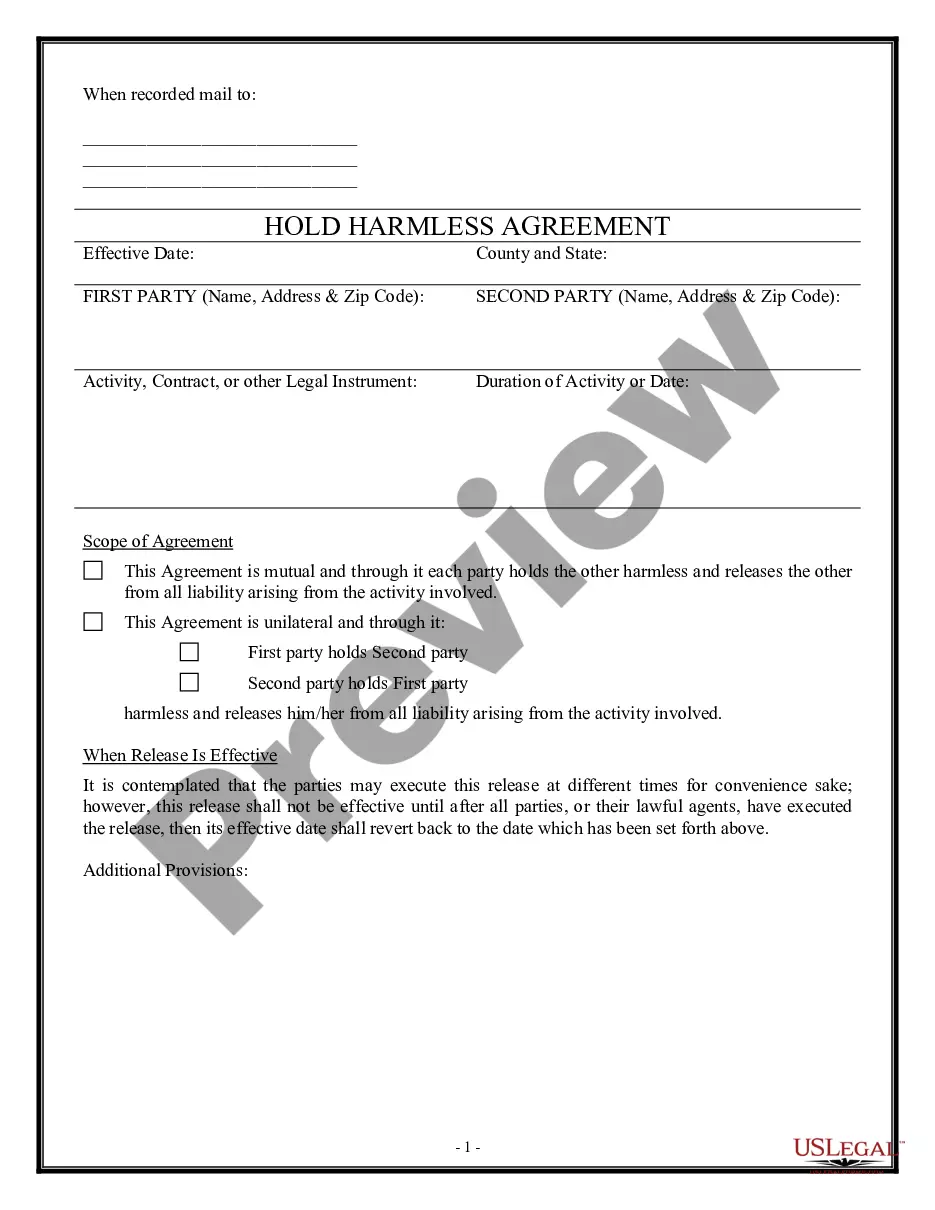
Discovering the right lawful document format can be a have a problem. Naturally, there are tons of web templates available on the net, but how will you obtain the lawful develop you need? Utilize the US Legal Forms site. The services gives a large number of web templates, including the New York Employer - Plan Administrator Notice to Employee of Unavailability of Continuation, which you can use for business and private requirements. All the types are inspected by experts and meet up with federal and state needs.
In case you are already authorized, log in to the accounts and click on the Down load key to get the New York Employer - Plan Administrator Notice to Employee of Unavailability of Continuation. Make use of accounts to look from the lawful types you possess ordered previously. Check out the My Forms tab of the accounts and obtain an additional duplicate from the document you need.
In case you are a fresh end user of US Legal Forms, listed below are easy guidelines for you to adhere to:
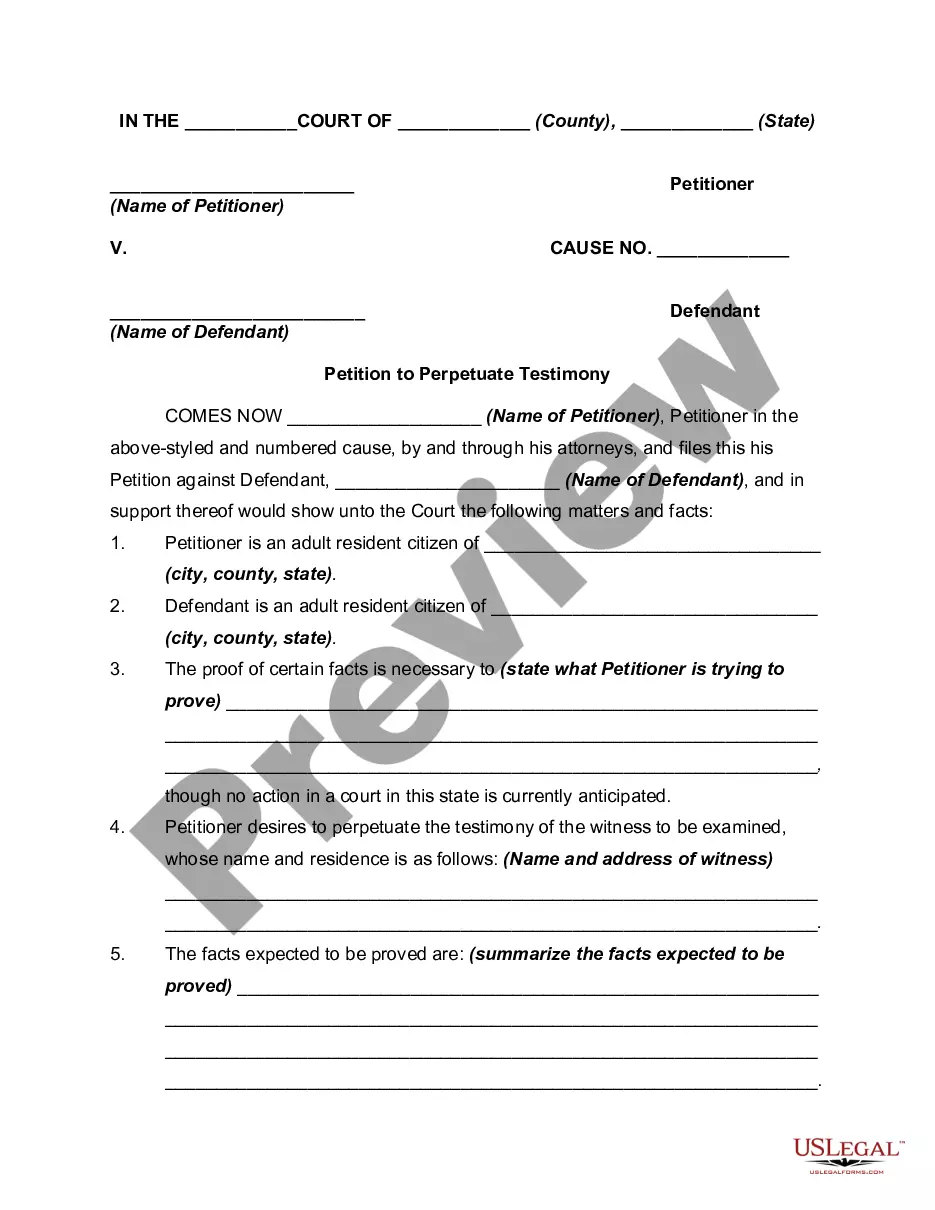
- Initial, make certain you have selected the proper develop for your town/area. You are able to look through the shape making use of the Review key and browse the shape description to make sure this is the best for you.
- If the develop will not meet up with your requirements, use the Seach industry to obtain the appropriate develop.
- Once you are sure that the shape is proper, click the Purchase now key to get the develop.
- Opt for the prices plan you need and enter in the needed info. Build your accounts and buy the transaction making use of your PayPal accounts or bank card.
- Opt for the submit format and obtain the lawful document format to the product.
- Complete, modify and print out and signal the acquired New York Employer - Plan Administrator Notice to Employee of Unavailability of Continuation.
US Legal Forms is definitely the biggest collection of lawful types where you will find a variety of document web templates. Utilize the service to obtain skillfully-produced documents that adhere to express needs.
Form popularity
FAQ
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
New York State law requires small employers (less than 20 employees) to provide the equivalent of COBRA benefits. You are entitled to 36 months of continued health coverage at a monthly cost to you of 102% of the actual cost to the employer which may be different from the amount deducted from your paychecks.
What is Cal-COBRA? Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
Federal COBRA is a federal law that lets you keep your group health plan when your job ends or your hours are cut. Federal COBRA requires continuation coverage be offered to covered employees, their spouses, former spouses, and dependent children.
COBRA is an acronym for the Consolidated Omnibus Budget Reconciliation Act, which provides eligible employees and their dependents the option of continued health insurance coverage when an employee loses their job or experiences a reduction of work hours.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
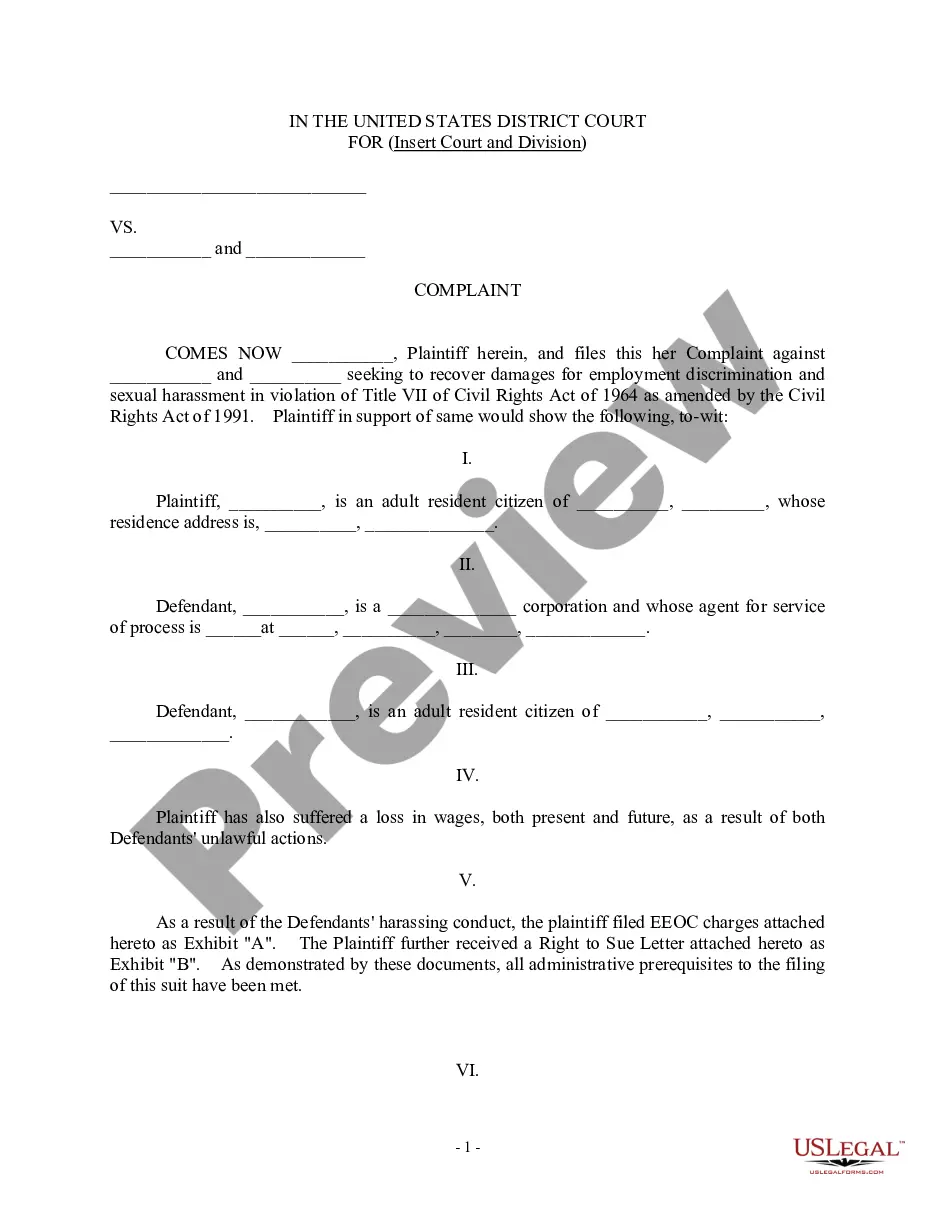
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,