Title: Ohio Summary of Rights and Obligations under COBRA: An Overview of Employee Benefits Introduction: The Ohio Summary of Rights and Obligations under COBRA (Consolidated Omnibus Budget Reconciliation Act) is a comprehensive piece of legislation designed to protect and provide continued access to health insurance benefits for employees and their eligible dependents, in case of certain qualifying events. This content aims to delve into the intricacies of this act, while highlighting its significance and types specific to Ohio. I. Understanding COBRA: An Overview — Introduction to COBRA and its main purpose — Explanation of qualifying events triggering COBRA coverage — Overview of beneficiaries who are eligible for coverage II. Ohio Summary of Rights and Obligations under COBRA: A. State-specific Provisions 1. Continuation Coverage Duration: — Detailed explanation of the maximum continuation period in Ohio — Types of qualifying events determining coverage duration 2. Eligibility Requirements: — Coverage eligibility criteria for employees, dependents, and former employees — Documentation and timing requirements for beneficiaries to enroll 3. Notification Processes: — The importance of employers' responsibility to notify affected individuals — Description of participants' role in informing their employer about qualifying events 4. Coverage Costs: — Explanation of the premium responsibilities for employees and their dependents — Breakdown of the maximum percentage employers can charge for COBRA coverage 5. Termination of COBRA Coverage: — Conditions leading to the termination of continuation coverage — Process and timeline for beneficiaries to transition to alternative coverage options III. Additional Ohio COBRA Coverage Types: A. Mini-COBRA Coverage: — Overview of Ohio's continuation coverage for smaller employers — Eligibility requirements and duration specific to Mini-COBRA B. Divorce and COBRA: — Explanation of how divorce affects COBRA in Ohio — Procedures and responsibilities for divorcing couples regarding continuation coverage C. Retirement and COBRA: — Detailed information on COBRA eligibility for retirees in Ohio — Coverage duration and considerations for retired employees Conclusion: Throughout Ohio, the Summary of Rights and Obligations under COBRA establishes a vital safety net for employees and their dependents regarding health insurance coverage. Understanding the specific provisions and additional types of COBRA coverage available under Ohio law is crucial to ensure the continuation of benefits during qualifying events. By remaining informed about COBRA obligations and rights specific to Ohio, individuals can make well-informed decisions for themselves and their families.
Ohio Summary of Rights and Obligations under COBRA
Description
How to fill out Ohio Summary Of Rights And Obligations Under COBRA?
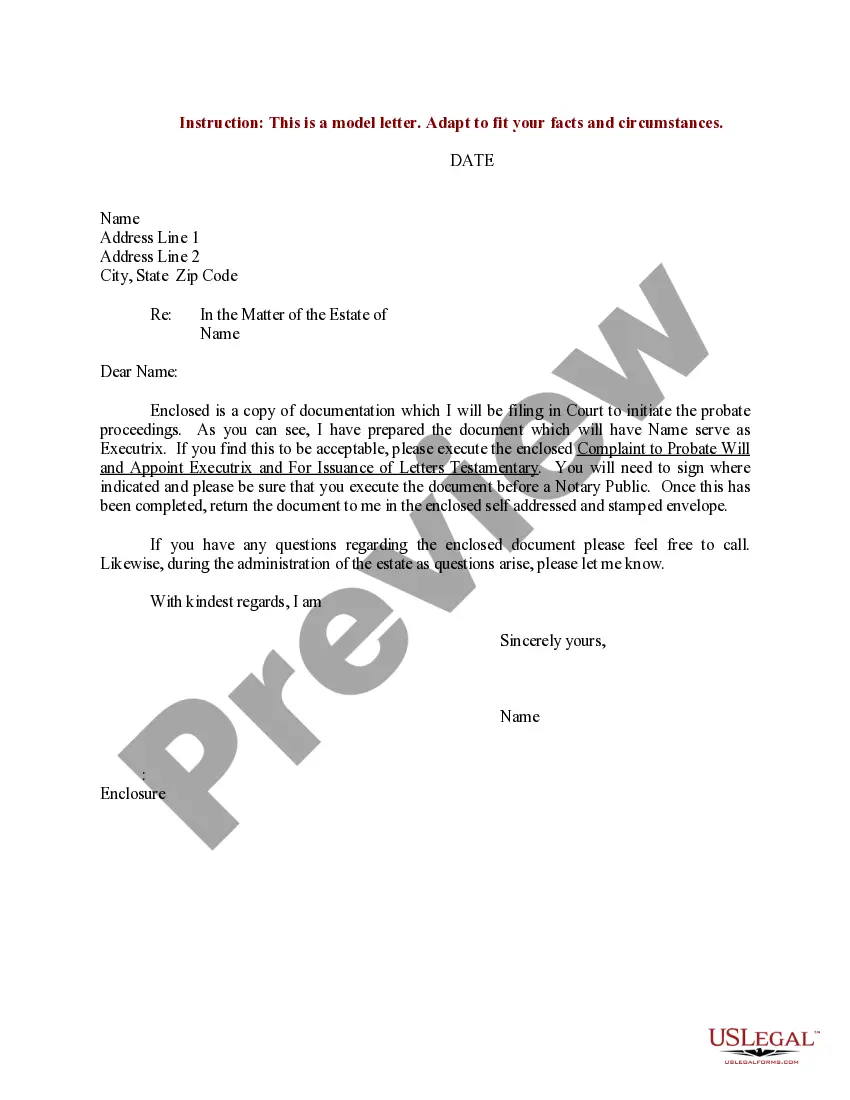
Are you currently in the place that you need paperwork for both business or individual reasons virtually every day? There are a lot of legal document layouts available online, but discovering kinds you can rely on isn`t simple. US Legal Forms offers a large number of type layouts, like the Ohio Summary of Rights and Obligations under COBRA, which can be composed to fulfill state and federal specifications.
If you are previously informed about US Legal Forms site and possess a merchant account, merely log in. Following that, you can acquire the Ohio Summary of Rights and Obligations under COBRA format.
If you do not offer an profile and need to begin using US Legal Forms, follow these steps:
- Get the type you will need and ensure it is for that correct city/county.
- Use the Review switch to review the shape.
- Read the description to actually have chosen the proper type.
- When the type isn`t what you`re seeking, make use of the Look for area to get the type that meets your requirements and specifications.
- Once you discover the correct type, click on Purchase now.
- Choose the costs program you want, fill out the desired info to produce your account, and buy your order utilizing your PayPal or charge card.
- Decide on a handy file formatting and acquire your copy.
Find every one of the document layouts you have bought in the My Forms menu. You can obtain a further copy of Ohio Summary of Rights and Obligations under COBRA anytime, if needed. Just go through the required type to acquire or printing the document format.
Use US Legal Forms, probably the most considerable collection of legal varieties, to save lots of efforts and stay away from faults. The services offers professionally created legal document layouts that can be used for a range of reasons. Create a merchant account on US Legal Forms and initiate generating your lifestyle easier.
Form popularity
FAQ
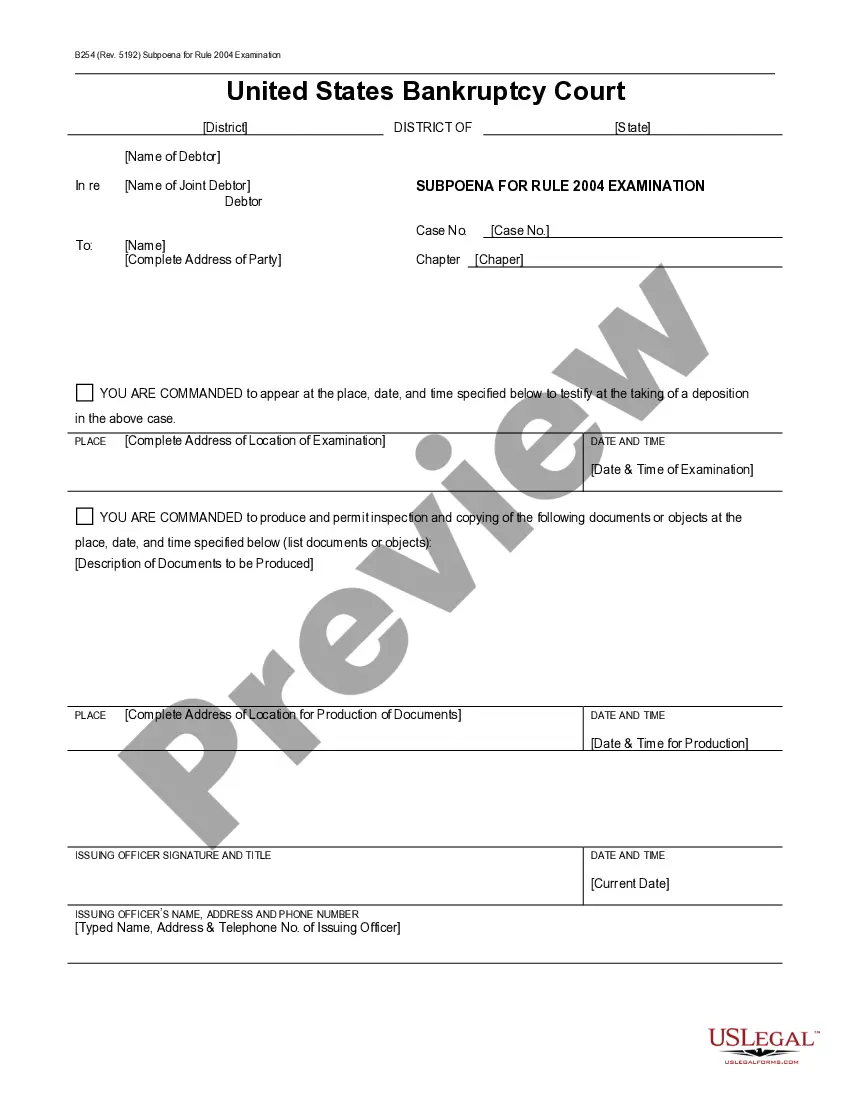
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
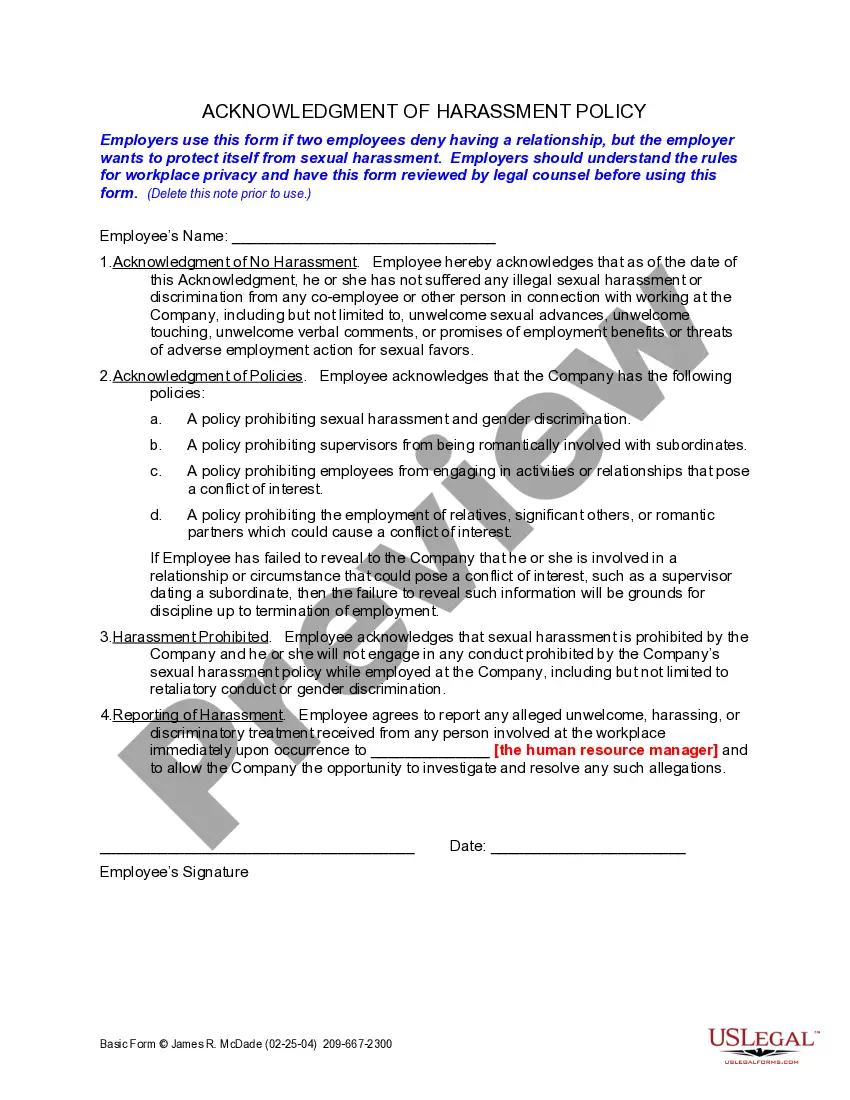
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
As an employer, you are responsible for notifying your former employee of the right to elect COBRA continuing health care coverage under your group plan. Most employers will include COBRA coverage information in the business employee handbook and as part of an employee's exit paperwork.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
State continuation coverage refers to state laws that enable employees to extend their employer-sponsored group health insurance even if they are not eligible for an extension through COBRA. While COBRA law applies throughout the U.S., it is only applicable to employers with 20 or more employees.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
Employers failing to comply with COBRA face a tax penalty of up to $100 daily for each affected former employer and each violation. The company is also subject to Employee Retirement Income Security Act penalties of up to $110 daily, commencing from the date the employer fails to comply.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
The term continuation coverage refers to the extended coverage provided under the group benefit plan in which an eligible employee or eligible dependent is currently enrolled.
COBRA is not an insurance company. COBRA is simply the continuation of the same coverage you had through a previous employer. To get proof of insurance, you would need to contact the COBRA Administrator at your previous employer. Typically, the COBRA Administrator is in the HR department.