Ohio Election Form for Continuation of Benefits - COBRA
Description
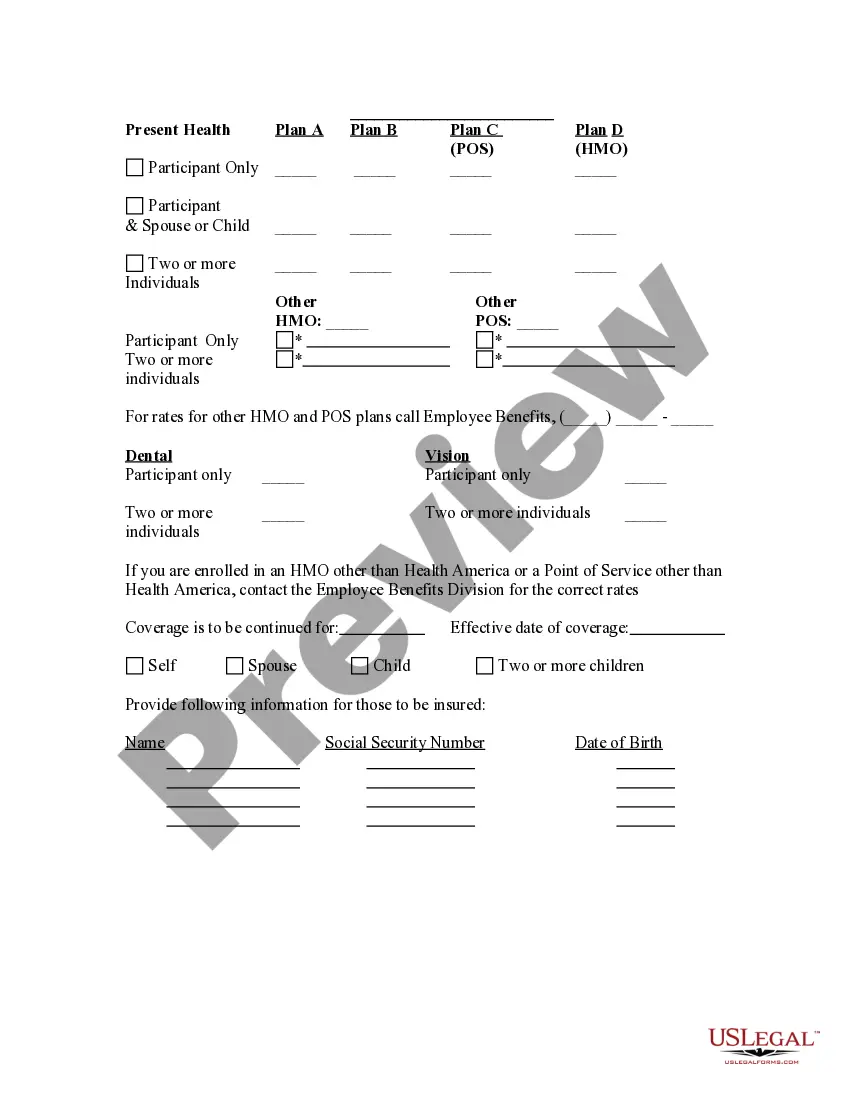
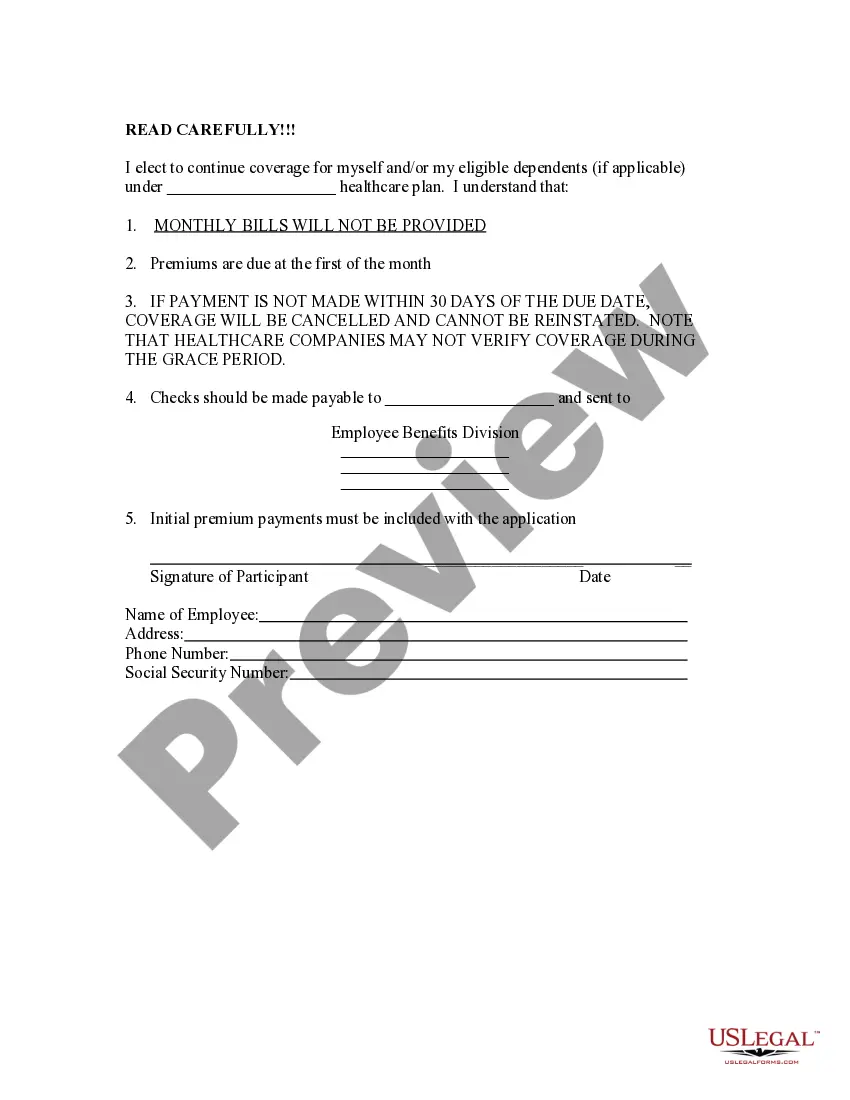
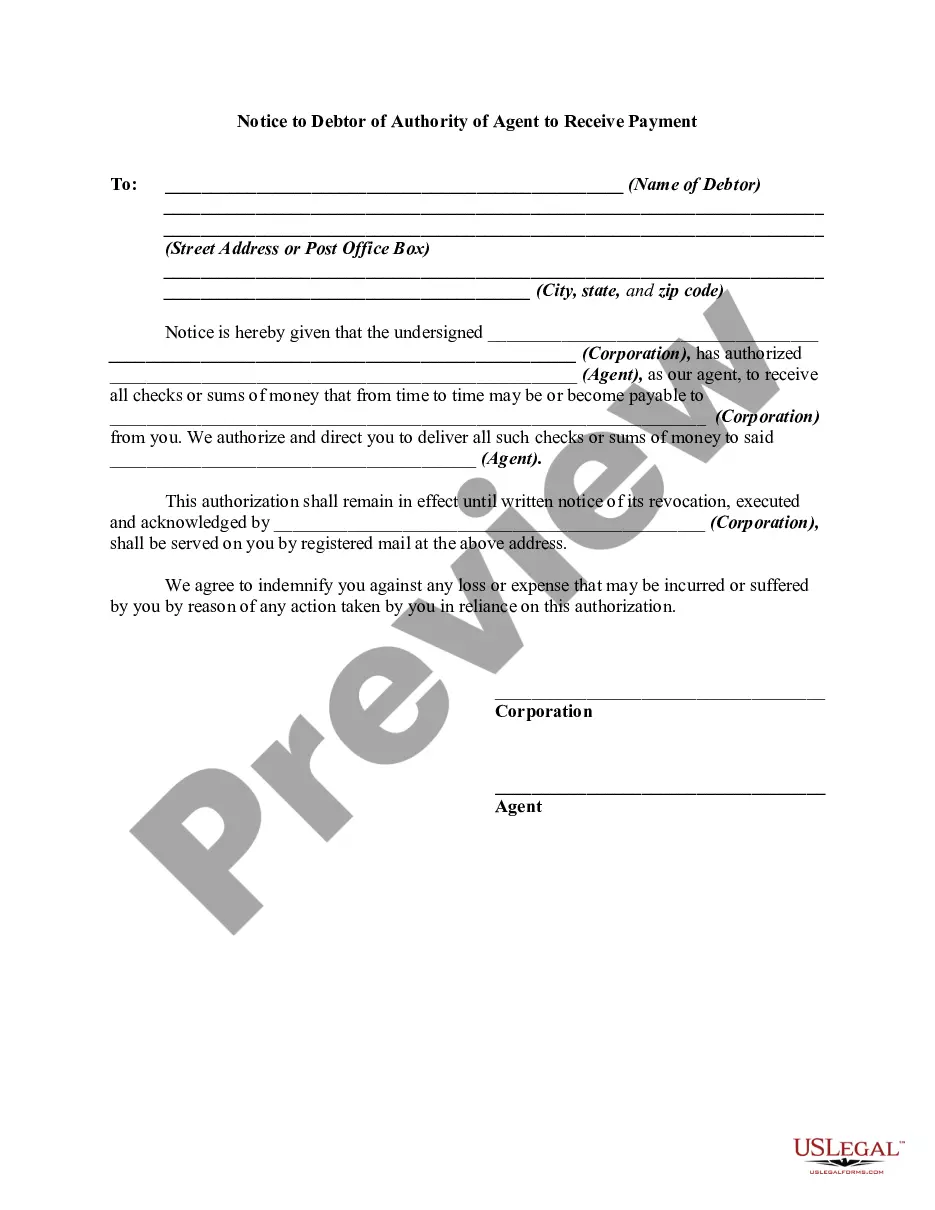
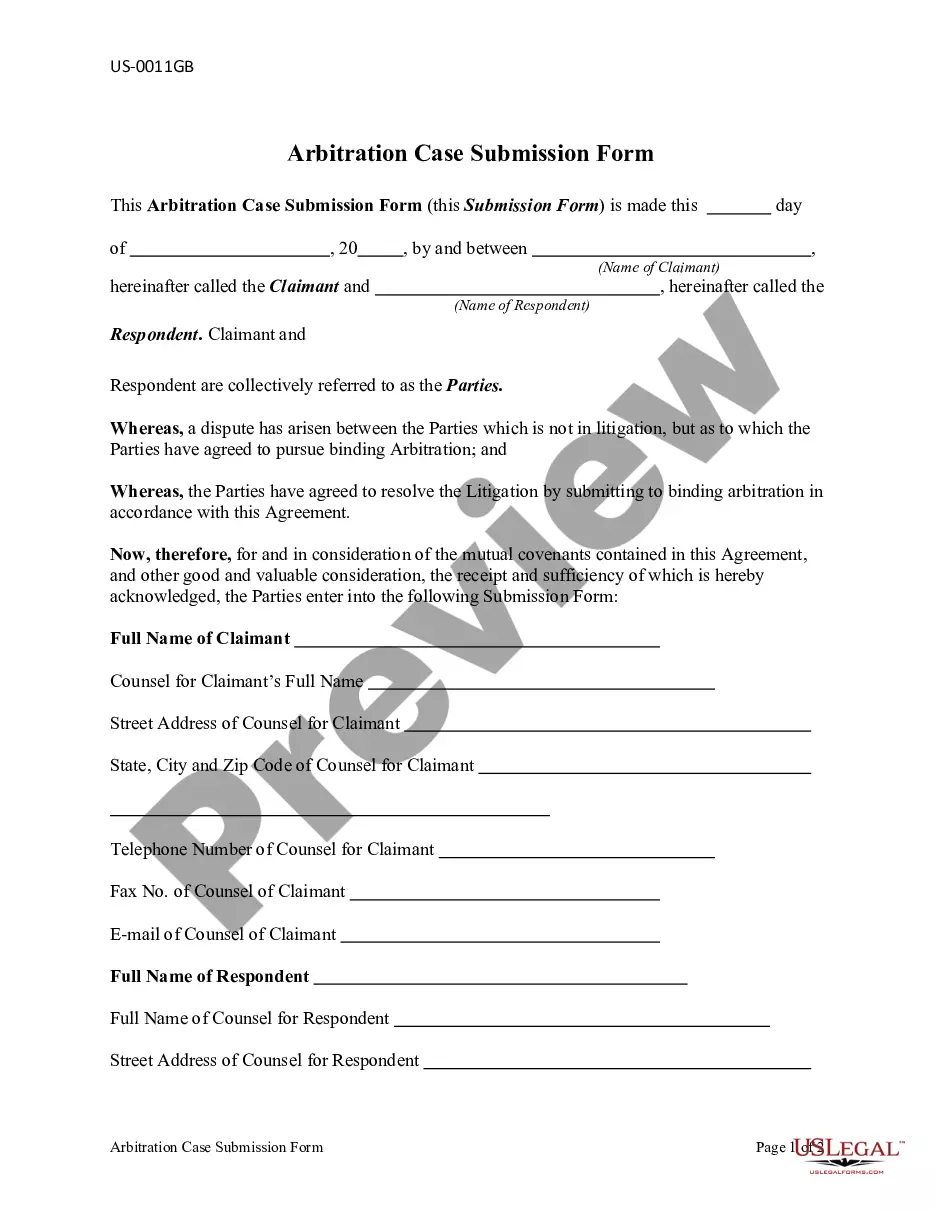
How to fill out Election Form For Continuation Of Benefits - COBRA?
Have you been in the place in which you require files for either company or specific functions almost every time? There are a lot of legitimate document layouts available on the Internet, but discovering ones you can rely isn`t straightforward. US Legal Forms provides 1000s of form layouts, such as the Ohio Election Form for Continuation of Benefits - COBRA, that are composed to fulfill federal and state requirements.
Should you be currently familiar with US Legal Forms website and have your account, basically log in. Afterward, you may acquire the Ohio Election Form for Continuation of Benefits - COBRA web template.
If you do not offer an bank account and wish to start using US Legal Forms, adopt these measures:
- Obtain the form you need and make sure it is for the proper metropolis/region.
- Take advantage of the Preview switch to review the shape.
- Read the description to actually have chosen the correct form.
- If the form isn`t what you`re trying to find, utilize the Lookup discipline to obtain the form that meets your requirements and requirements.
- Whenever you obtain the proper form, click Purchase now.
- Pick the costs program you would like, submit the specified information and facts to make your bank account, and buy the transaction with your PayPal or charge card.
- Choose a practical paper format and acquire your duplicate.
Discover each of the document layouts you have bought in the My Forms food selection. You can get a further duplicate of Ohio Election Form for Continuation of Benefits - COBRA whenever, if needed. Just go through the required form to acquire or printing the document web template.
Use US Legal Forms, one of the most substantial variety of legitimate varieties, to conserve time and prevent errors. The support provides appropriately created legitimate document layouts which you can use for a variety of functions. Make your account on US Legal Forms and start producing your way of life a little easier.
Form popularity
FAQ
Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Key Takeaways. COBRA provides a good option for keeping your employer-sponsored health plan for a while after you leave your job. Although, the cost can be high. Make an informed choice by looking at all your options during the 60-day enrollment period, and don't focus on the premium alone.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
Ohio's continuation coverage applies to employer sickness and accident coverage and the employer's eligible employees generally, and to an employer not provided for under federal law, such as church plans or governmental plans.
If you are entitled to elect COBRA coverage, you must be given an election period of at least 60 days (starting on the later of the date you are furnished the election notice or the date you would lose coverage) to choose whether or not to elect continuation coverage.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.