Oklahoma Schedule of Reimbursement
Description
How to fill out Oklahoma Schedule Of Reimbursement?
When it comes to filling out Oklahoma Schedule of Reimbursement, you almost certainly imagine an extensive procedure that requires choosing a perfect form among countless very similar ones and after that being forced to pay a lawyer to fill it out for you. In general, that’s a sluggish and expensive choice. Use US Legal Forms and select the state-specific template in a matter of clicks.
For those who have a subscription, just log in and then click Download to find the Oklahoma Schedule of Reimbursement form.
If you don’t have an account yet but need one, keep to the point-by-point manual below:
- Be sure the file you’re saving applies in your state (or the state it’s required in).
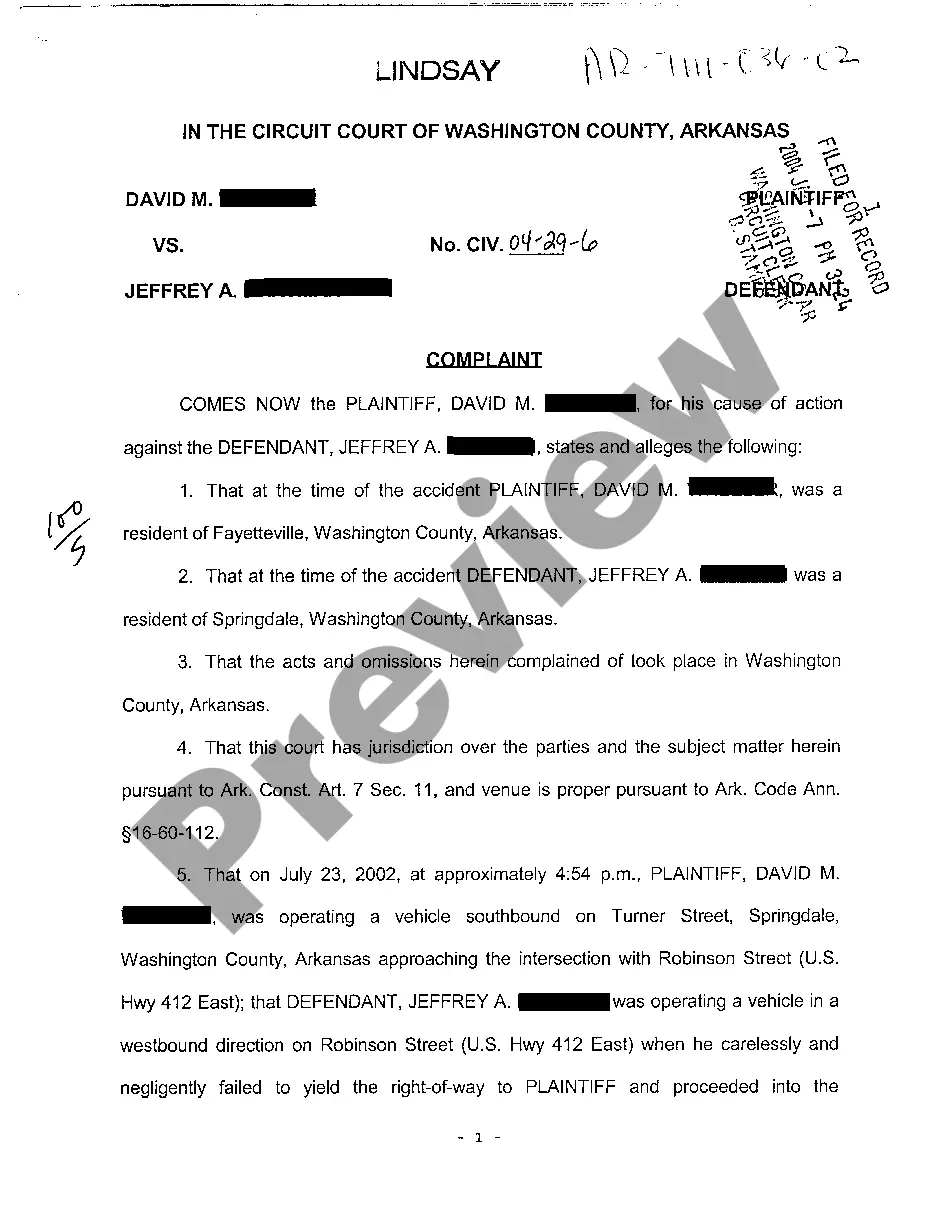
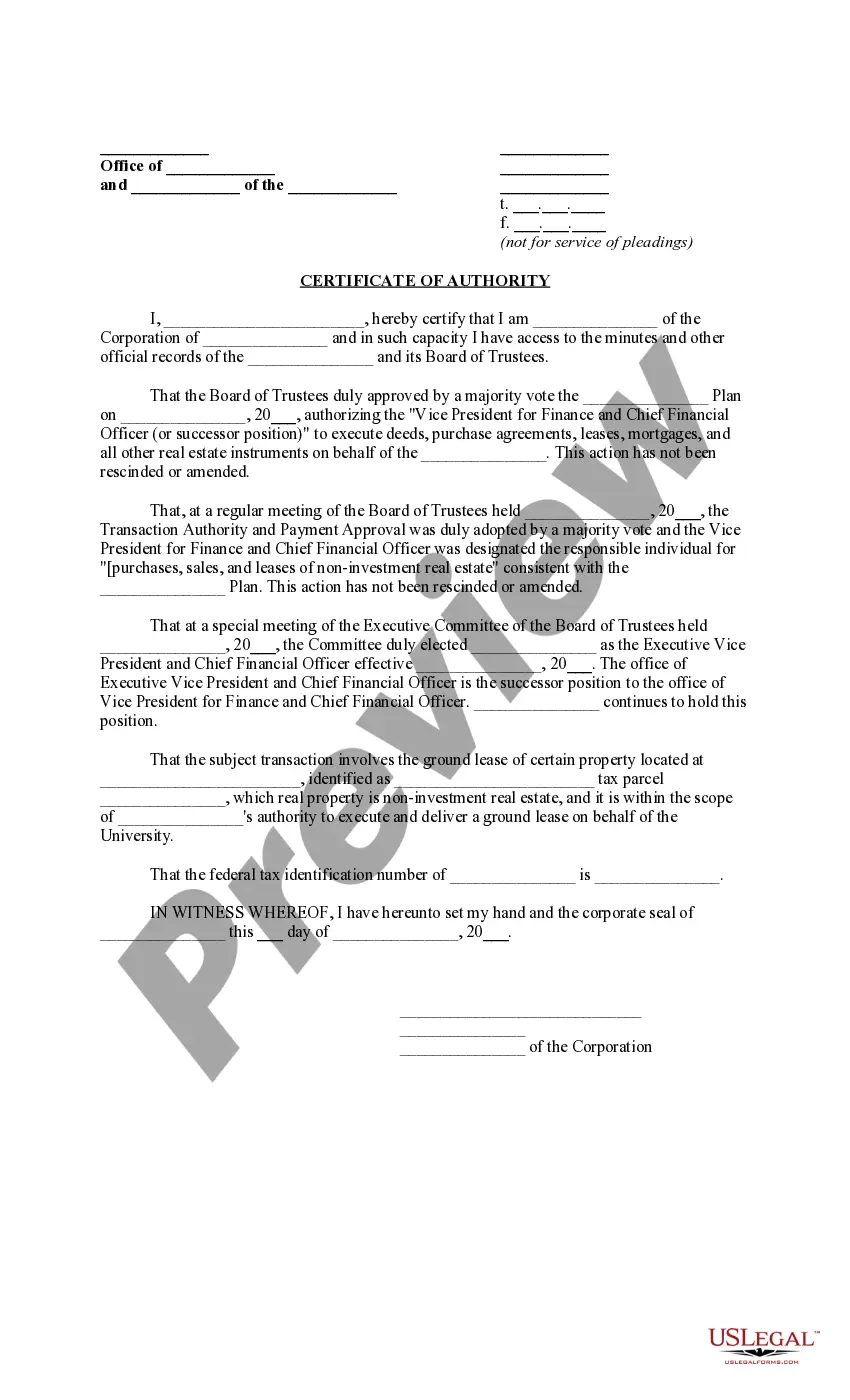
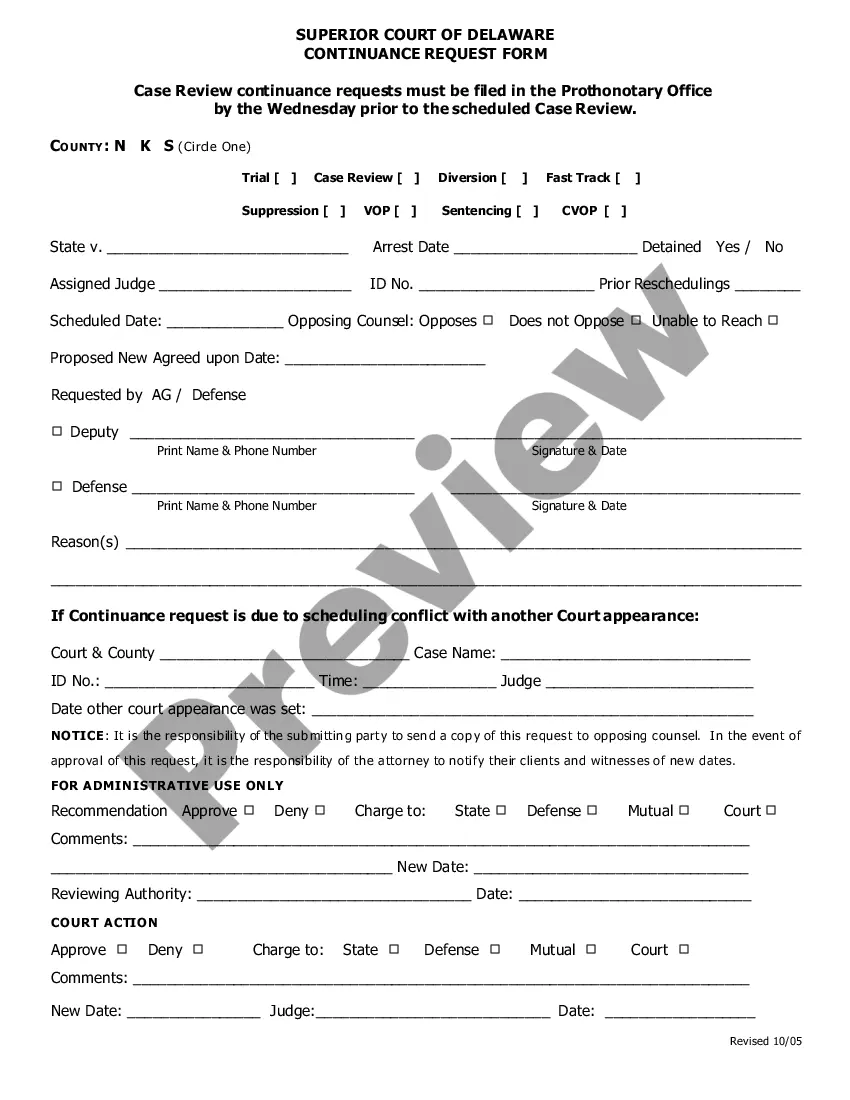
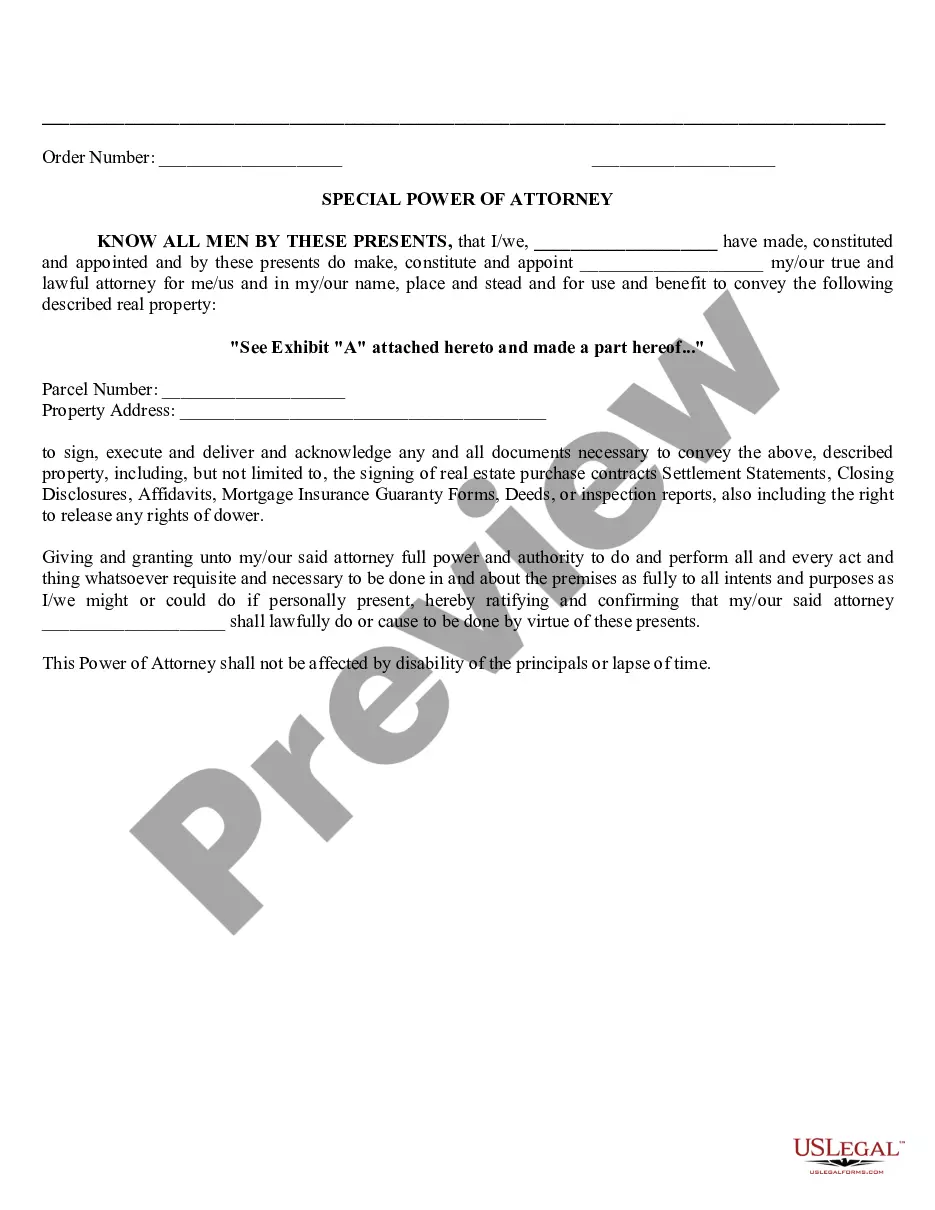
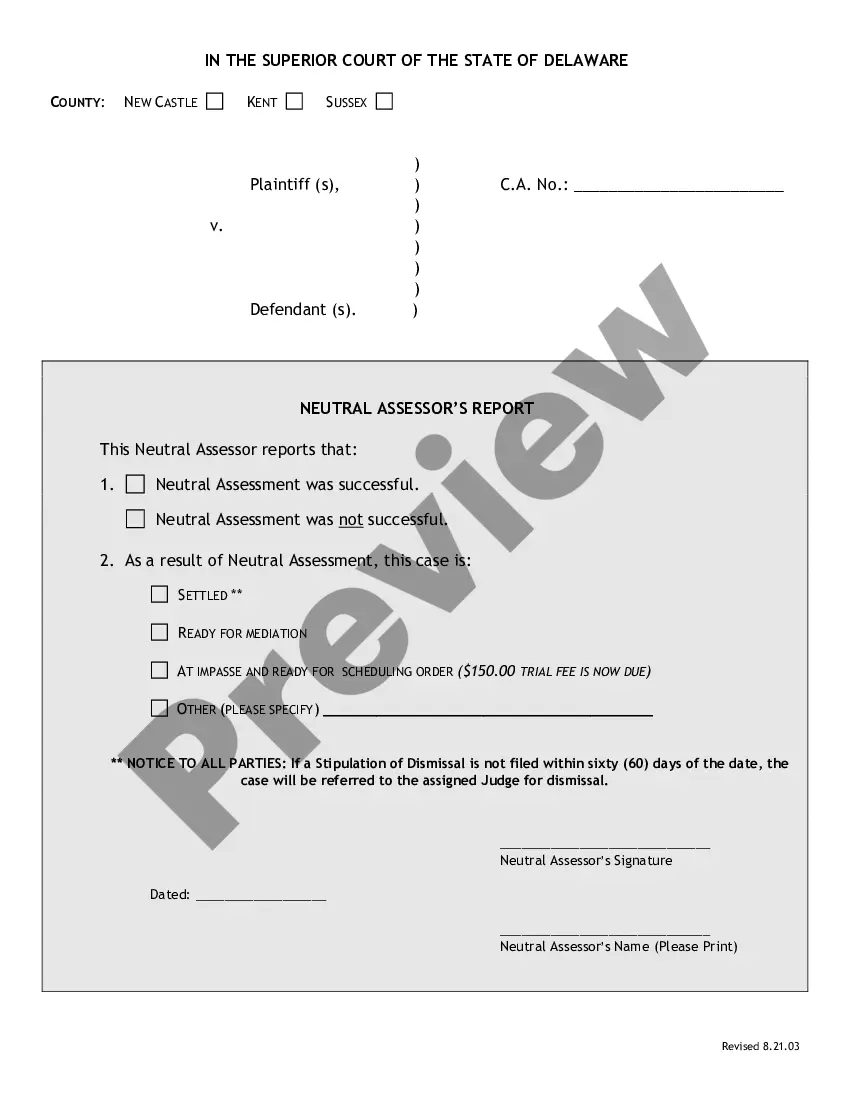
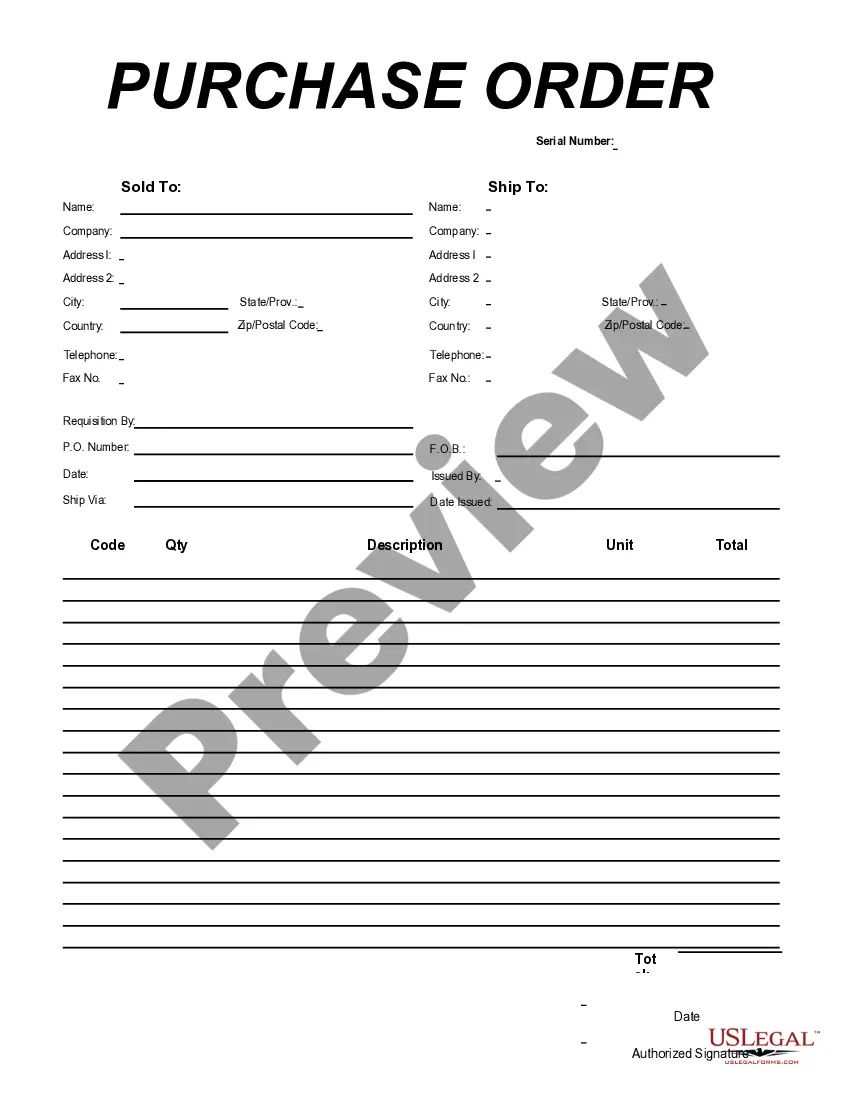
- Do this by reading the form’s description and also by visiting the Preview option (if offered) to see the form’s information.
- Simply click Buy Now.
- Select the appropriate plan for your budget.
- Subscribe to an account and select how you would like to pay: by PayPal or by card.
- Save the file in .pdf or .docx format.
- Get the file on your device or in your My Forms folder.
Skilled lawyers draw up our templates to ensure that after saving, you don't have to bother about enhancing content material outside of your personal info or your business’s information. Sign up for US Legal Forms and get your Oklahoma Schedule of Reimbursement document now.
Form popularity
FAQ
Reimbursement schedule also called a fee schedule is a complete listing of fees that are used by medicare.
A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis.
Most payers determine fee schedules first by establishing relative weights (also referred to as relative value units) for the list of service codes and then by using a dollar conversion factor to establish the fee schedule.
An insurance company will negotiate a fee schedule within its network of preferred doctors for members to use. Since a provider is able to bill any amount, this allows insurance companies to pay less than billed charges while still allowing the providers to be reimbursed an amount they deem reasonable.
In its simplest form, a conversion factor (CF) is a value used to convert some unit of measurement into a charge.For our purposes here, the conversion factor is a per725bunit value that is multiplied by the relative value units (RVU) to convert it into a fee (or charge) for a particular medical service or procedure.
An insurance company will negotiate a fee schedule within its network of preferred doctors for members to use. Since a provider is able to bill any amount, this allows insurance companies to pay less than billed charges while still allowing the providers to be reimbursed an amount they deem reasonable.
The Centers for Medicare and Medicaid Services (CMS) determines the final relative value unit (RVU) for each code, which is then multiplied by the annual conversion factor (a dollar amount) to yield the national average fee. Rates are adjusted according to geographic indices based on provider locality.
You can call the provider representative at the insurance company (payer) and ask them to fax you a copy of your contract with an updated fee schedule. Go to the provider section on the insurance company's website, and download a copy of the fee schedule.
A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis.