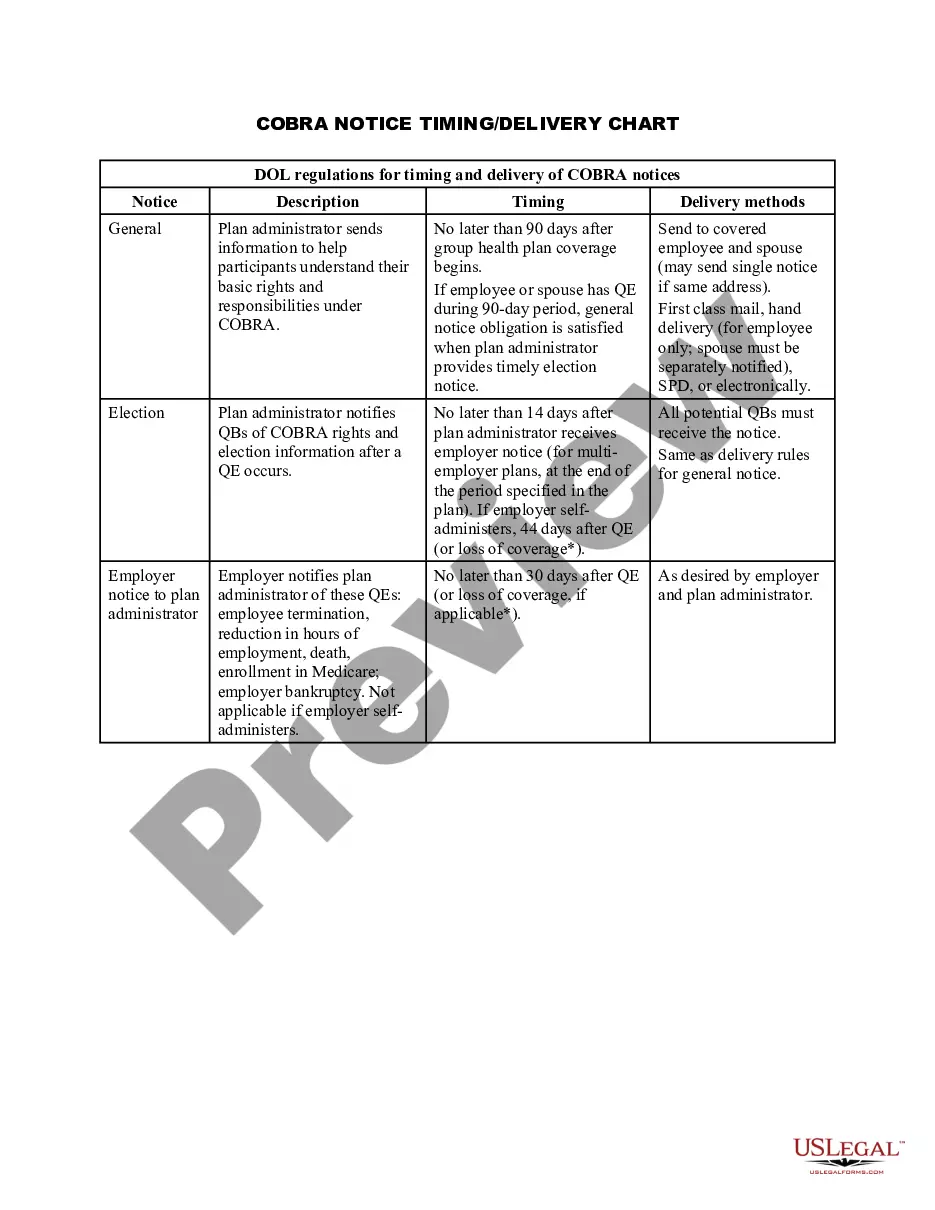
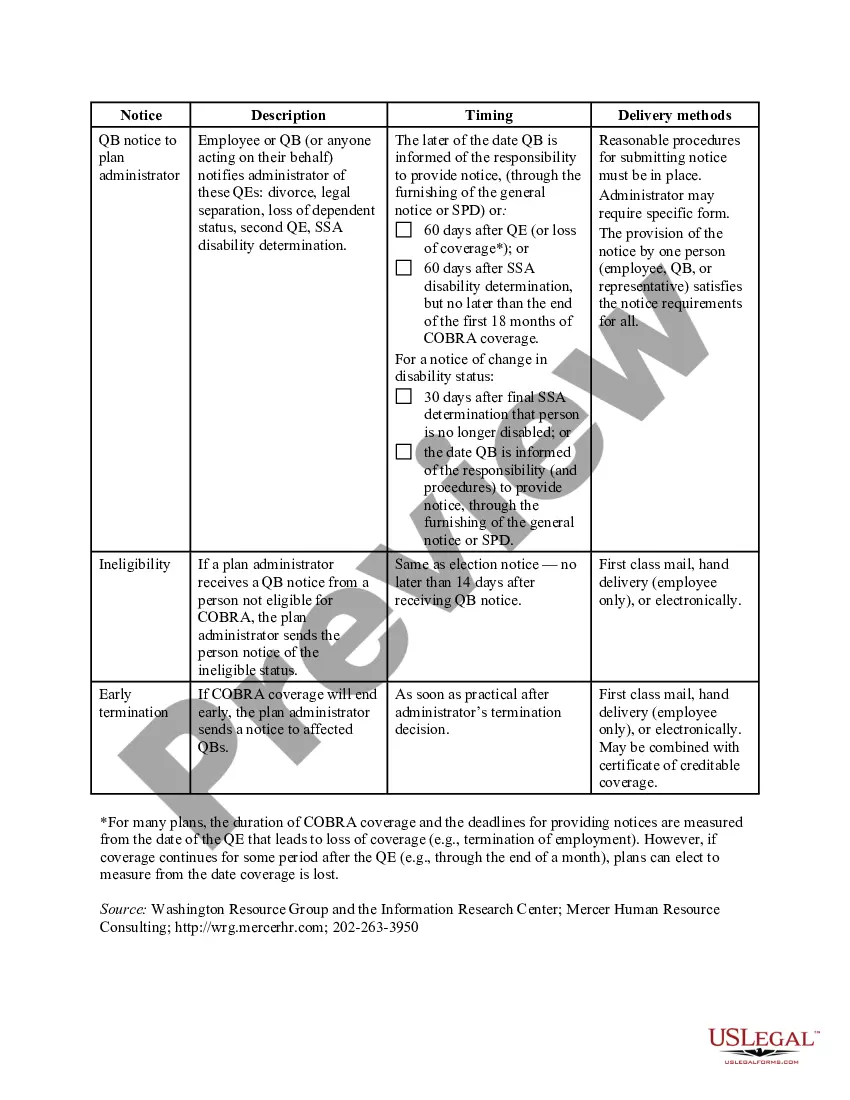
The Oklahoma COBRA Notice Timing Delivery Chart is a vital document that outlines the timelines and requirements for delivering COBRA notices in the state of Oklahoma. COBRA, short for Consolidated Omnibus Budget Reconciliation Act, is a federal law that allows eligible individuals to continue their health insurance coverage after experiencing a qualifying event, such as job loss or reduction in work hours. The COBRA Notice Timing Delivery Chart provides employers, employees, and health insurance administrators with a clear understanding of when and how the COBRA notices should be delivered. This chart ensures compliance with the law, preventing any legal repercussions and ensuring that employees receive timely information about their rights to continue their health coverage. Multiple types of Oklahoma COBRA Notice Timing Delivery Charts exist, each tailored to specific qualifying events. Some of these charts include: 1. Termination of Employment: This chart outlines the timeline for providing COBRA notices when an employee's employment has been terminated. It defines when the notice must be sent, the deadline for the employee to elect COBRA coverage, and the duration of coverage. 2. Reduction in Work Hours: This type of chart applies to situations where an employee's work hours have been reduced, making them eligible for COBRA coverage. It specifies the timeline for delivering the notice, the deadline for electing the coverage, and the duration of coverage. 3. Death of Employee: In cases where an employee passes away, this chart highlights the timeline for delivering COBRA notices to the employee's eligible dependents or beneficiaries. It outlines the deadline for electing coverage and the duration of coverage. 4. Divorce or Legal Separation: This chart caters to situations where an employee loses coverage due to a divorce or legal separation. It specifies the timing for delivering COBRA notices, the deadline for electing coverage, and the duration of coverage. The Oklahoma COBRA Notice Timing Delivery Chart serves as a crucial tool for employers and health insurance administrators, enabling them to effectively communicate important COBRA information to eligible individuals within the legal timeframes. It ensures compliance with the law, avoiding potential penalties and liabilities, while also providing eligible individuals with the necessary information to make informed decisions regarding their healthcare coverage during challenging times.
Oklahoma COBRA Notice Timing Delivery Chart
Description
How to fill out Oklahoma COBRA Notice Timing Delivery Chart?
Are you currently in the situation in which you require paperwork for both enterprise or specific purposes almost every day time? There are plenty of legal document templates accessible on the Internet, but finding types you can rely on is not easy. US Legal Forms offers a large number of form templates, like the Oklahoma COBRA Notice Timing Delivery Chart, that happen to be created to fulfill state and federal requirements.
In case you are already knowledgeable about US Legal Forms site and get your account, simply log in. Next, you may download the Oklahoma COBRA Notice Timing Delivery Chart design.
Unless you provide an accounts and want to start using US Legal Forms, abide by these steps:
- Find the form you require and make sure it is to the correct town/region.
- Take advantage of the Review button to analyze the form.
- Look at the outline to ensure that you have chosen the proper form.
- When the form is not what you`re seeking, utilize the Search field to obtain the form that meets your requirements and requirements.
- If you discover the correct form, click on Acquire now.
- Opt for the pricing plan you would like, complete the necessary information to generate your bank account, and purchase an order using your PayPal or bank card.
- Pick a convenient paper format and download your copy.
Locate each of the document templates you may have bought in the My Forms food list. You can get a further copy of Oklahoma COBRA Notice Timing Delivery Chart anytime, if necessary. Just click the essential form to download or print out the document design.
Use US Legal Forms, by far the most comprehensive variety of legal forms, to save some time and steer clear of errors. The services offers appropriately manufactured legal document templates which can be used for a range of purposes. Create your account on US Legal Forms and begin generating your lifestyle a little easier.