Title: Understanding Oregon Summary of Rights and Obligations under COBRA: A Comprehensive Guide Keywords: Oregon Summary of Rights and Obligations, COBRA, continuation coverage, health insurance, termination, eligibility, notification, enrollment, time frames, premiums, coverage options. Introduction: The Oregon Summary of Rights and Obligations under COBRA provides crucial information to employees and their families about their rights to continue health insurance coverage after certain qualifying events. Under the Consolidated Omnibus Budget Reconciliation Act (COBRA), employees and dependents may be eligible to receive continuation coverage. This guide aims to provide a detailed description of the various types of Oregon Summary of Rights and Obligations under COBRA, ensuring clarity and understanding of the process. 1. Basic Overview and Eligibility: The Oregon Summary of Rights and Obligations under COBRA explains the basic requirements for individuals to be eligible for continuation coverage. It highlights the qualifying events that can trigger the COBRA rights, such as employment termination, reduction in work hours, divorce, or death of the covered employee. 2. Notification and Enrollment: This section explains the rights and obligations regarding notification and enrollment procedures. Employers are mandated to provide timely COBRA notices to employees and their dependents. The Oregon Summary outlines the critical information that must be included in the notification. It also covers important enrollment deadlines and the consequences of failing to enroll within the prescribed timeframe. 3. Coverage Options and Duration: The Oregon Summary of Rights and Obligations under COBRA outlines the coverage options available to individuals under continuation coverage. It explains the health insurance plans that can be continued and for how long. Additionally, it highlights instances where the coverage can be extended due to disability or a second qualifying event. 4. Maintaining Coverage and Premiums: This section details the obligations of individuals to continue their COBRA coverage. It clarifies the payment timeframes, acceptable payment methods, and grace periods for premium payments. Moreover, it emphasizes the consequences of non-payment, including loss of coverage. Types of Oregon Summary of Rights and Obligations under COBRA: a) Individual Coverage: This type of Oregon Summary applies to employees who experience qualifying events entitling them to individual COBRA coverage. It provides a comprehensive overview of the rights and obligations specific to individuals. b) Family Coverage: The Oregon Summary for Family Coverage addresses the rights and obligations related to family members who become eligible for COBRA continuation coverage due to a qualifying event affecting the covered employee. c) Extended Coverage: The Oregon Summary for Extended Coverage highlights the rights and obligations of individuals who are eligible for an extended duration of COBRA continuation coverage, primarily due to disability or a second qualifying event. Conclusion: The Oregon Summary of Rights and Obligations under COBRA plays a crucial role in providing individuals and families with the necessary information to make well-informed decisions about their health insurance coverage. By understanding the types of Oregon COBRA summaries, eligible individuals can ensure they are aware of their rights, obligations, and available options during critical life transitions.
Oregon Summary of Rights and Obligations under COBRA
Description
How to fill out Oregon Summary Of Rights And Obligations Under COBRA?
If you want to full, obtain, or produce legitimate record web templates, use US Legal Forms, the largest selection of legitimate varieties, which can be found online. Make use of the site`s easy and convenient research to discover the documents you require. A variety of web templates for enterprise and individual uses are sorted by types and states, or keywords. Use US Legal Forms to discover the Oregon Summary of Rights and Obligations under COBRA in just a number of click throughs.
When you are already a US Legal Forms client, log in in your accounts and then click the Down load button to obtain the Oregon Summary of Rights and Obligations under COBRA. You can even entry varieties you formerly saved in the My Forms tab of your respective accounts.
If you use US Legal Forms the very first time, follow the instructions listed below:
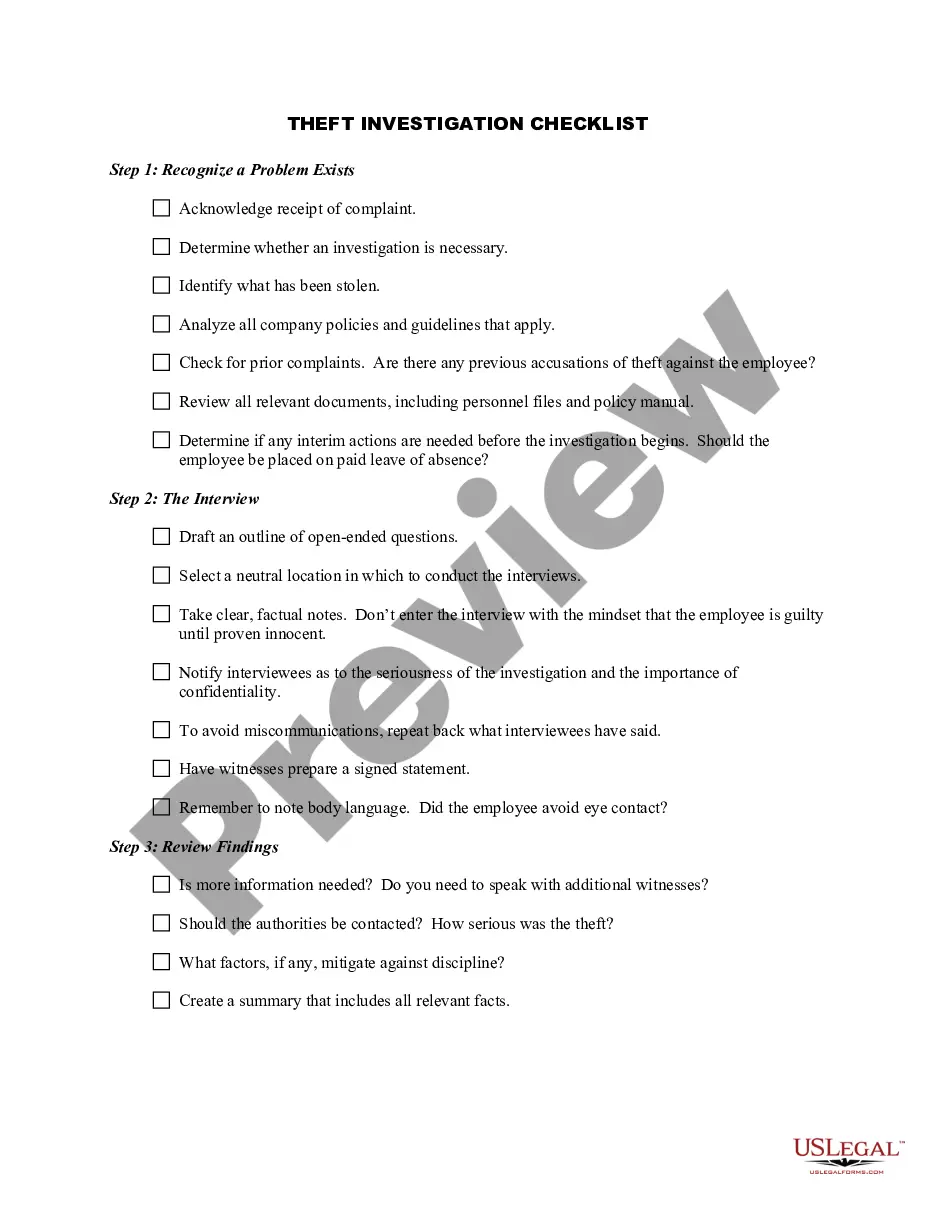
- Step 1. Ensure you have chosen the form for your proper city/country.
- Step 2. Take advantage of the Review option to check out the form`s content. Do not neglect to read through the information.
- Step 3. When you are unhappy with all the kind, take advantage of the Search field at the top of the display screen to find other versions of the legitimate kind web template.
- Step 4. After you have found the form you require, click the Acquire now button. Pick the pricing program you favor and put your accreditations to register for the accounts.
- Step 5. Procedure the purchase. You may use your bank card or PayPal accounts to complete the purchase.
- Step 6. Find the structure of the legitimate kind and obtain it in your product.
- Step 7. Total, modify and produce or sign the Oregon Summary of Rights and Obligations under COBRA.
Every legitimate record web template you acquire is yours for a long time. You might have acces to every kind you saved in your acccount. Select the My Forms segment and decide on a kind to produce or obtain yet again.
Contend and obtain, and produce the Oregon Summary of Rights and Obligations under COBRA with US Legal Forms. There are millions of professional and condition-particular varieties you can utilize for your personal enterprise or individual requires.
Form popularity
FAQ
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Who is eligible? An employee who has had continuous health coverage (not necessarily with the same employer) for at least three months prior to the date employment or coverage ended. The employee's spouse and children are also eligible to maintain coverage.
What is COBRA continuation coverage? COBRA is a federal law that requires large employers (including Multnomah County) to offer employees and their families the opportunity to continue their health care coverage when there is a qualifying event that would result in a loss of coverage in the County's health plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Who pays for COBRA coverage? The employee generally pays the full cost of the insurance premiums. In fact, the law allows the employer to charge 102 percent of the premium, and to keep the 2 percent to cover your administrative costs.
As an employer, you are responsible for notifying your former employee of the right to elect COBRA continuing health care coverage under your group plan. Most employers will include COBRA coverage information in the business employee handbook and as part of an employee's exit paperwork.
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
COBRA continuation coverage is a temporary continuation of coverage that generally lasts for 18 months due to employment termination or reduction of hours of work.