Title: Understanding Oregon Employer — Plan Administrator Notice to Employee of Unavailability of Continuation: Types and Detailed Description Introduction: The Oregon Employer — Plan Administrator Notice to Employee of Unavailability of Continuation is an important document that outlines the unavailability of continuation benefits for employees. It helps employees understand the circumstances under which they may not be eligible for continued coverage and what alternatives they may have. This comprehensive guide will provide a detailed description of the notice and highlight its different types. Types of Oregon Employer — Plan Administrator Notice to Employee of Unavailability of Continuation: 1. Termination of Group Health Plan Coverage: This notice is provided to employees when their group health plan coverage is terminated due to specific reasons, such as the cessation of the employer's business operations or the non-payment of premiums. It outlines the options available to employees for securing alternative health coverage. 2. Ineligibility for Continuation Benefits: This type of notice is issued to employees who are ineligible for continuation benefits. It specifies the reasons for ineligibility, such as not meeting the minimum length of employment, not having group health plan coverage, or engaging in conduct that disqualifies them from continued coverage. The notice also provides information about other coverage options. 3. Exhaustion of Continuation Benefits: When an employee exhausts their continuation benefits, this notice will inform them about the end of their coverage period and the termination of their extended health benefits. It may include information about conversion plans or alternative coverage options that the employee can pursue. 4. Plan Discontinuation or Modifications: In certain cases, employers may decide to discontinue the group health plan or make significant modifications to its benefits. This notice details the changes, provides reasons for the modifications, and explains the implications for employee coverage. It may also outline alternative coverage options that employees can explore. Detailed Description of the Oregon Employer — Plan Administrator Notice to Employee of Unavailability of Continuation: — Purpose and Importance: This notice is crucial as it informs employees about the unavailability of continuation benefits, helps them understand the reasons, and guides them towards alternative coverage options. — Legal Requirements: Oregon law mandates that employers provide this notice to employees to ensure transparency and protect their rights. — Content of Notice: The notice contains detailed information such as the employee's eligibility for continuation benefits, reasons for ineligibility, effective date of termination or modification of coverage, duration of continuation benefits if applicable, and details about alternative coverage options. — Delivery Method: Employers must provide this notice in writing, either by hand delivery or by mail. Some employers may also provide it electronically, depending on employee preferences and consent. — Timing: The notice should be provided promptly after the employee's ineligibility is determined or when significant changes are made to the group health plan. — Employee Rights and Responsibilities: The notice emphasizes that employees still have certain rights and responsibilities even if they are ineligible for continuation benefits. It may include information about state or federal programs that could assist them in securing health coverage. — Contact Information: The notice typically includes the relevant contact details of the employer's plan administrator or human resources department to address any questions or concerns employees may have. Conclusion: The Oregon Employer — Plan Administrator Notice to Employee of Unavailability of Continuation serves as a vital communication tool to inform employees about their eligibility for continuation benefits, the reasons for ineligibility, and alternative coverage options. It ensures compliance with state laws and helps employees navigate their healthcare needs effectively. Employers must provide these notices accurately, promptly, and in a comprehensive manner to empower employees and support their well-being.
Oregon Employer - Plan Administrator Notice to Employee of Unavailability of Continuation
Description
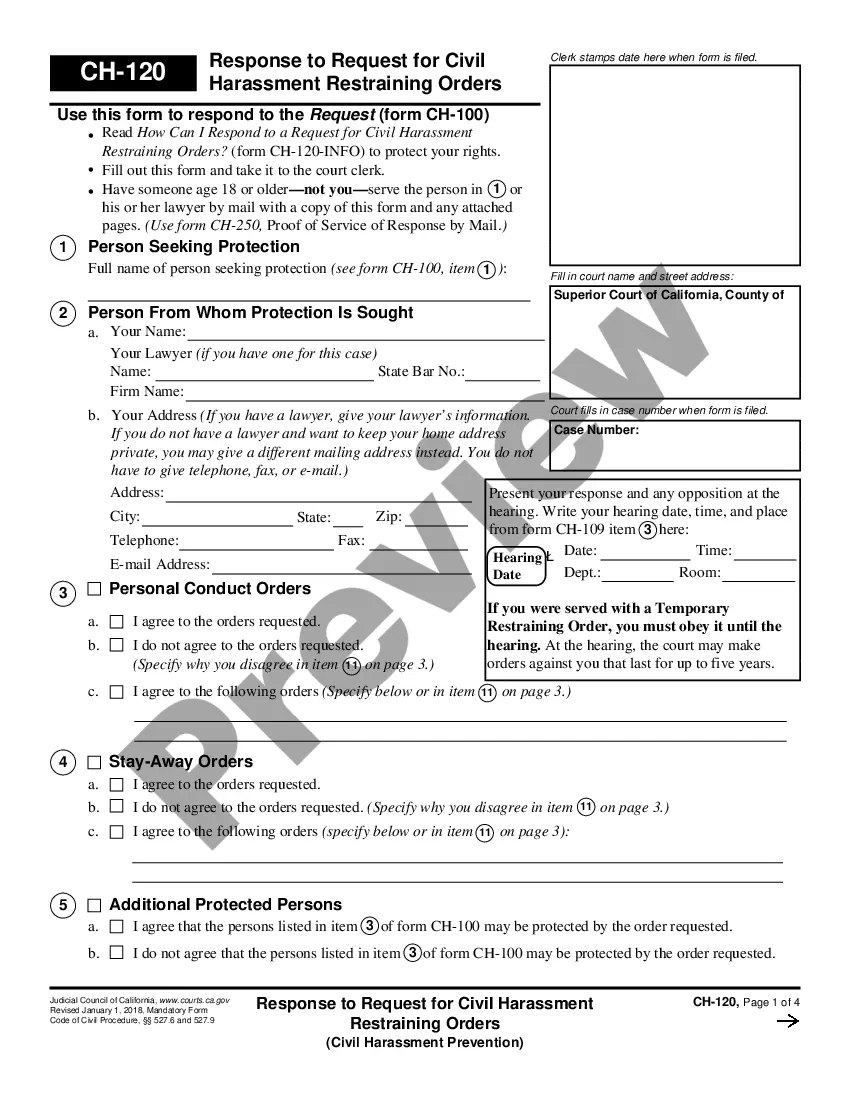
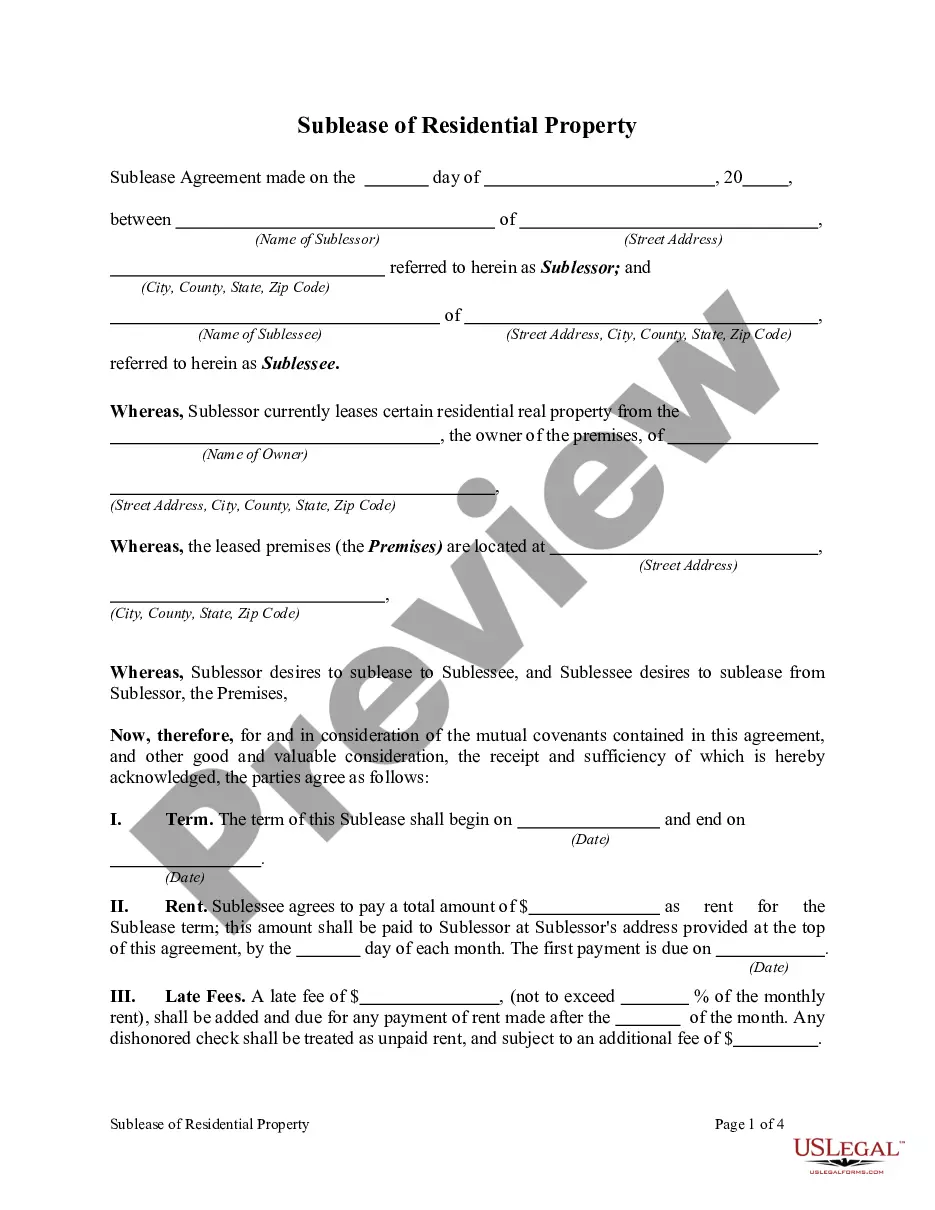
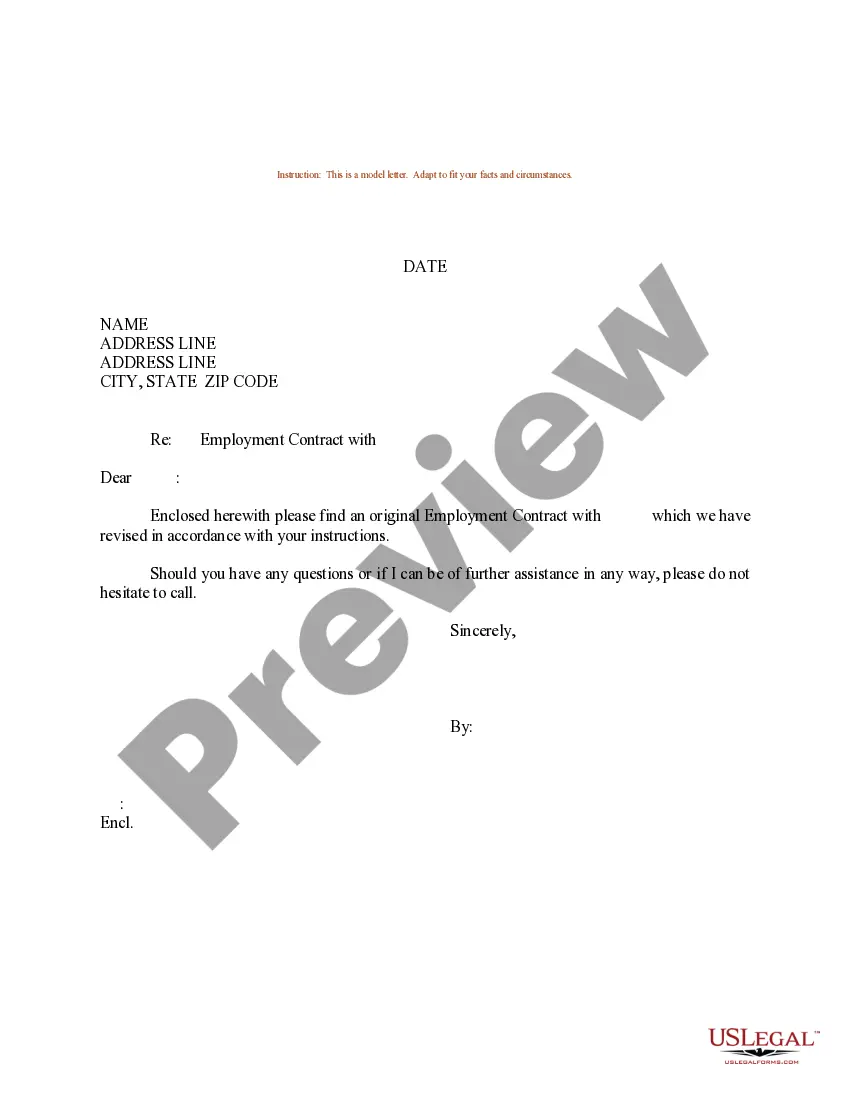
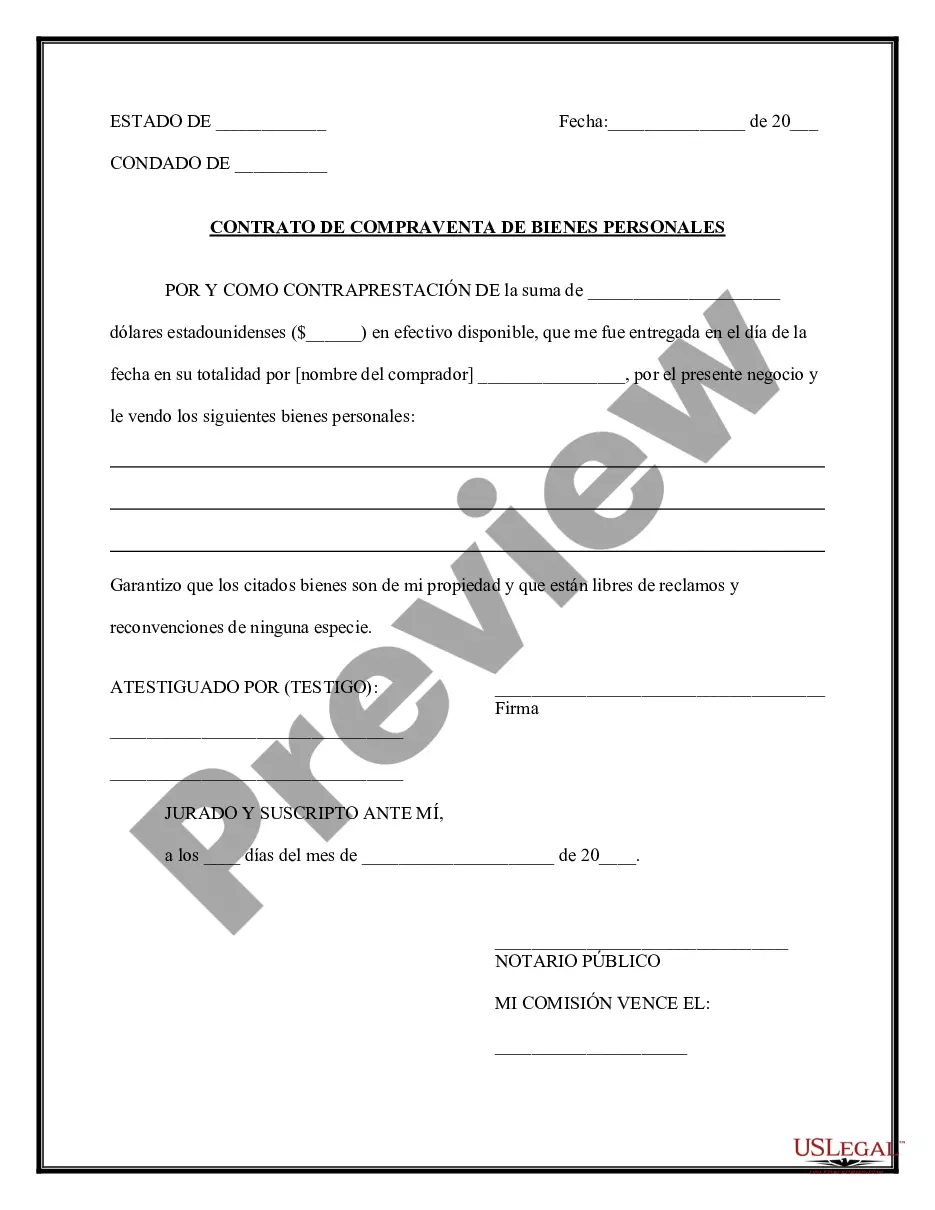
How to fill out Oregon Employer - Plan Administrator Notice To Employee Of Unavailability Of Continuation?
If you want to total, download, or print authorized record web templates, use US Legal Forms, the biggest variety of authorized forms, which can be found online. Use the site`s basic and practical research to obtain the files you require. Numerous web templates for business and specific uses are categorized by categories and suggests, or keywords and phrases. Use US Legal Forms to obtain the Oregon Employer - Plan Administrator Notice to Employee of Unavailability of Continuation in just a handful of mouse clicks.
If you are presently a US Legal Forms consumer, log in to the profile and click on the Download key to get the Oregon Employer - Plan Administrator Notice to Employee of Unavailability of Continuation. Also you can accessibility forms you previously delivered electronically from the My Forms tab of the profile.
If you work with US Legal Forms the very first time, refer to the instructions beneath:
- Step 1. Ensure you have chosen the shape for that right town/nation.
- Step 2. Take advantage of the Preview solution to look through the form`s information. Do not forget to read through the information.
- Step 3. If you are unhappy together with the form, use the Lookup industry on top of the screen to find other versions of your authorized form web template.
- Step 4. Once you have discovered the shape you require, click the Purchase now key. Select the prices strategy you prefer and add your accreditations to register for an profile.
- Step 5. Approach the purchase. You may use your Мisa or Ьastercard or PayPal profile to finish the purchase.
- Step 6. Find the formatting of your authorized form and download it on your own system.
- Step 7. Comprehensive, change and print or sign the Oregon Employer - Plan Administrator Notice to Employee of Unavailability of Continuation.
Each and every authorized record web template you buy is yours permanently. You have acces to every single form you delivered electronically with your acccount. Go through the My Forms segment and choose a form to print or download yet again.
Contend and download, and print the Oregon Employer - Plan Administrator Notice to Employee of Unavailability of Continuation with US Legal Forms. There are thousands of professional and status-particular forms you can use for your business or specific requires.
Form popularity
FAQ
Loss of Coverage Letter Letter from your previous health carrier indicating an involuntary loss of coverage. The supporting document must indicate your name, the names of any dependents that were covered under the prior plan and the date the previous health coverage ended.
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
Model COBRA notices are provided on the U.S. Department of Labor's COBRA Continuation webpage under the Regulations section.Step 1: Initial Notification.Step 2: Qualifying Event Notices.Step 3: Insurance Carrier Notification.Step 4: Election and Payment.Step 5 (if needed): Late or Missing Payments.More items...
Cal-COBRA administration requires four basic compliance components:Notifying all eligible group health care participants of their Cal-COBRA rights.Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.More items...
COBRA is an acronym for the Consolidated Omnibus Budget Reconciliation Act, which provides eligible employees and their dependents the option of continued health insurance coverage when an employee loses their job or experiences a reduction of work hours.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Federal COBRA is a federal law that lets you keep your group health plan when your job ends or your hours are cut. Federal COBRA requires continuation coverage be offered to covered employees, their spouses, former spouses, and dependent children.
What is Cal-COBRA? Cal-COBRA is a California Law that lets you keep your group health plan when your job ends or your hours are cut. It may also be available to people who have exhausted their Federal COBRA.
Oregon state continuation allows you to continue to be covered under your employer's insurance plan for up to nine months. It is the state's equivalent to federal Consolidated Omnibus Budget Reconciliation Act (COBRA) for employers with fewer than 20 employees and others who are not subject to COBRA law.