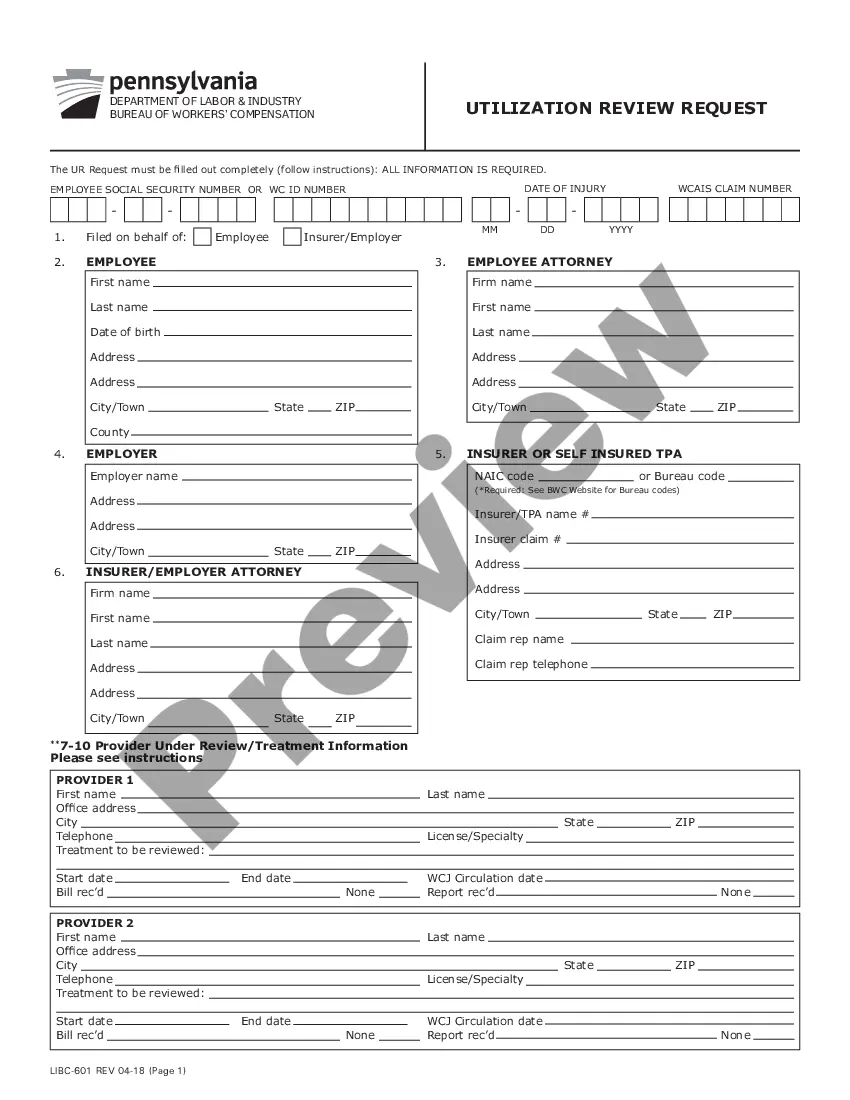
Pennsylvania requires individuals to submit a Utilization Review Request when they are seeking coverage for healthcare services that are not typically covered by their insurance plan. The Utilization Review Request must be completed and submitted to the insurance company for review and approval. The Pennsylvania instructions for Completing Utilization Review Request include: 1. Identifying the patient: In the Utilization Review Request, the patient must provide their name, address, date of birth, insurance plan information, and contact information. 2. Identifying the provider: The patient must also provide the name, address, and contact information of the provider who will be providing the services. 3. Describing the services: The patient must provide a detailed description of the services they are requesting coverage for. This should include the diagnosis or condition that the services are being requested for, the type of services being requested, the frequency of the services, and the expected duration of the services. 4. Requesting pre-authorization: The patient must include a request for pre-authorization for the services. This request should include any additional information that the insurance company may need to make a decision on the request. 5. Submitting the form: The Utilization Review Request must be signed and dated by the patient and submitted to the insurance company for review. These are the Pennsylvania instructions for Completing Utilization Review Request. Following these instructions will help ensure that the request is processed quickly and accurately.
Pennsylvania instructions for Completing Utilization Review Request
Description
How to fill out Pennsylvania Instructions For Completing Utilization Review Request?
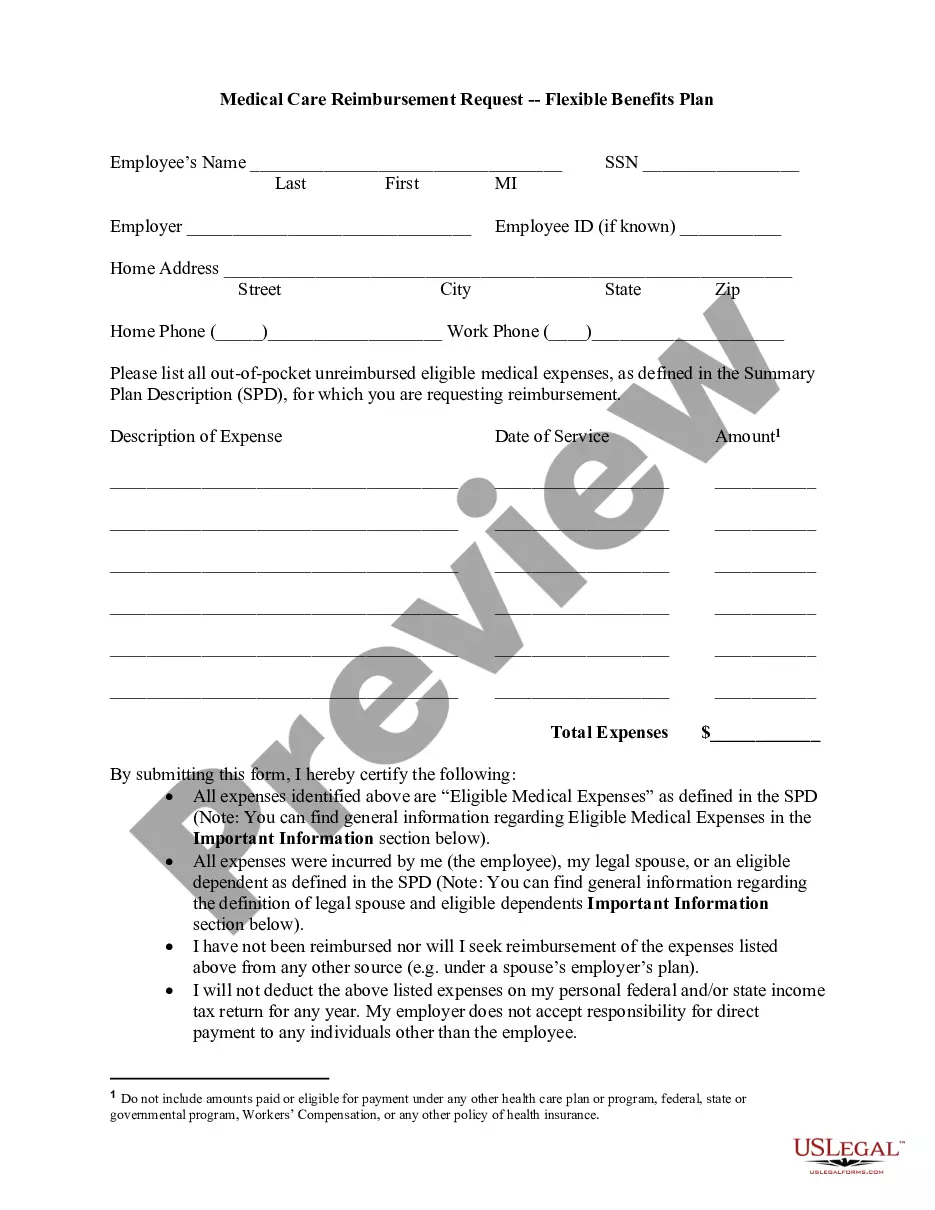
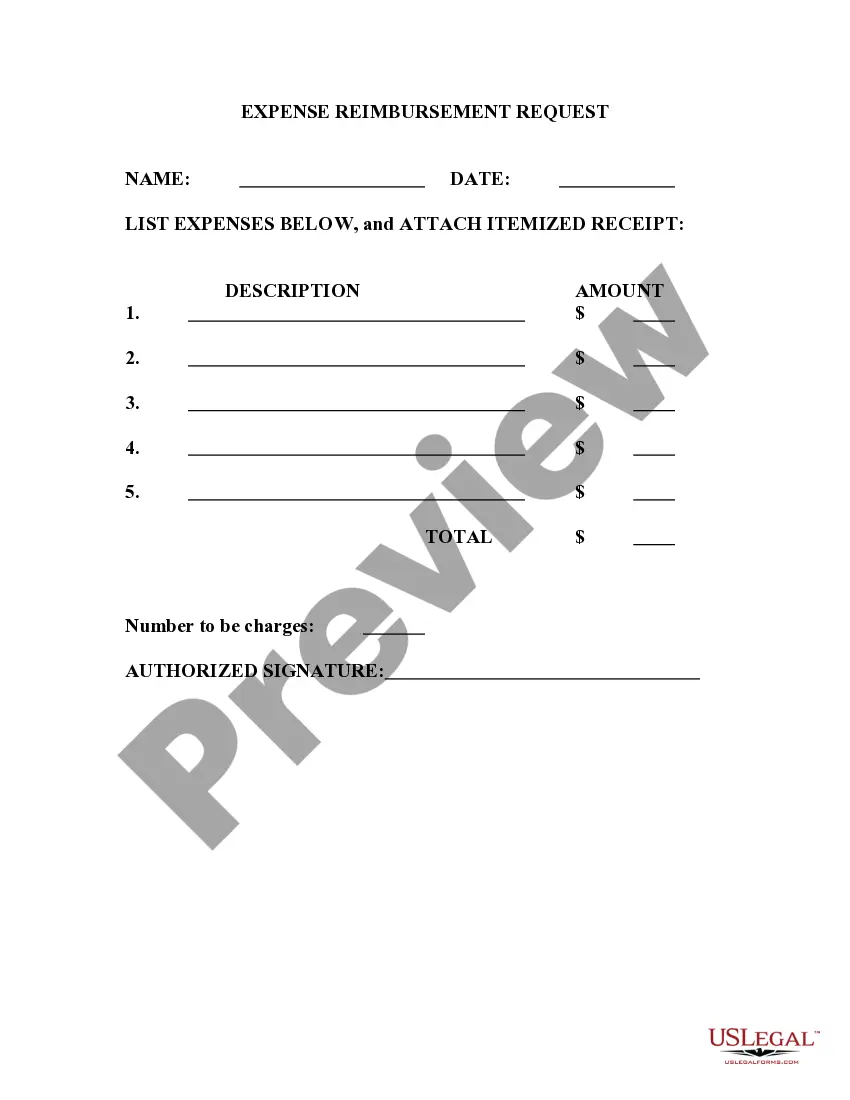
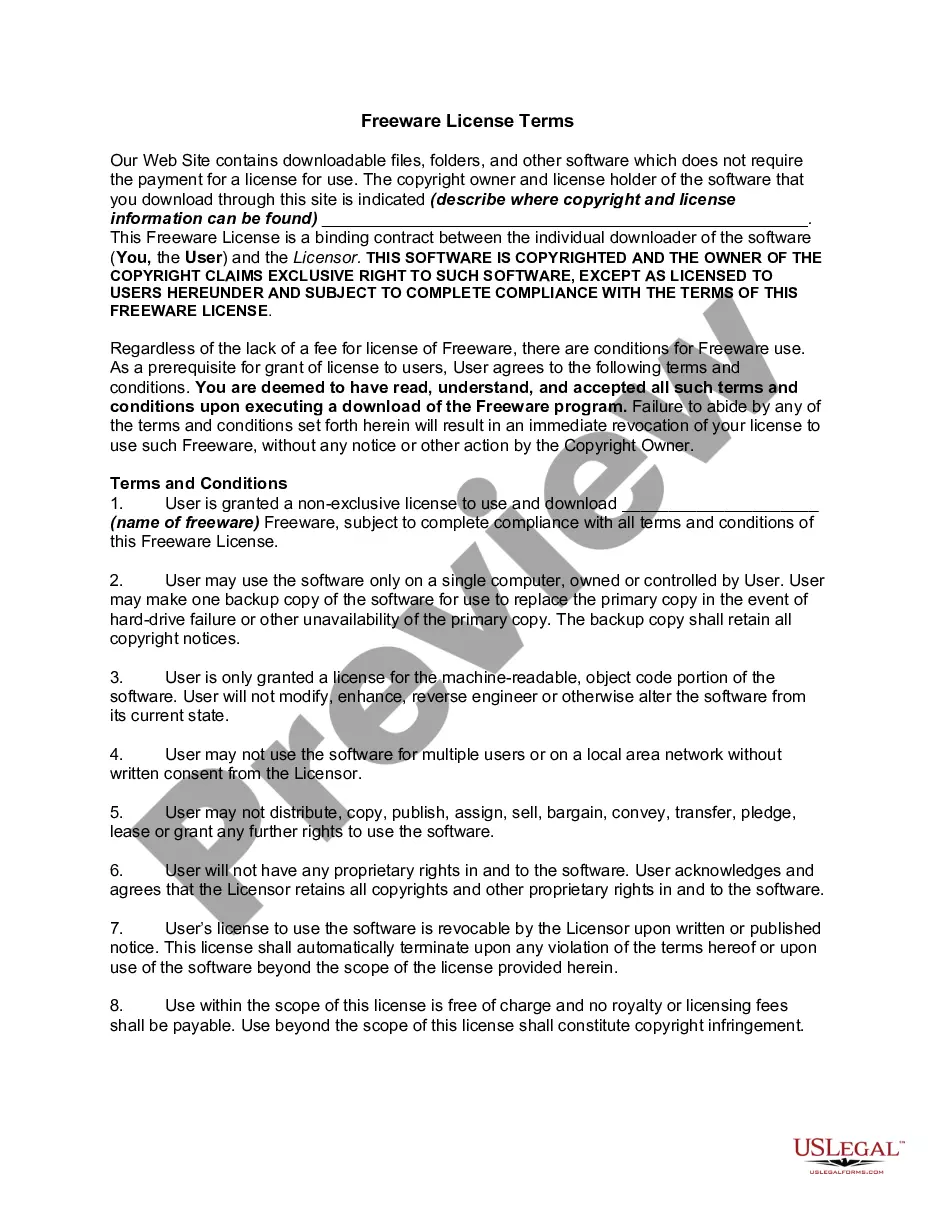
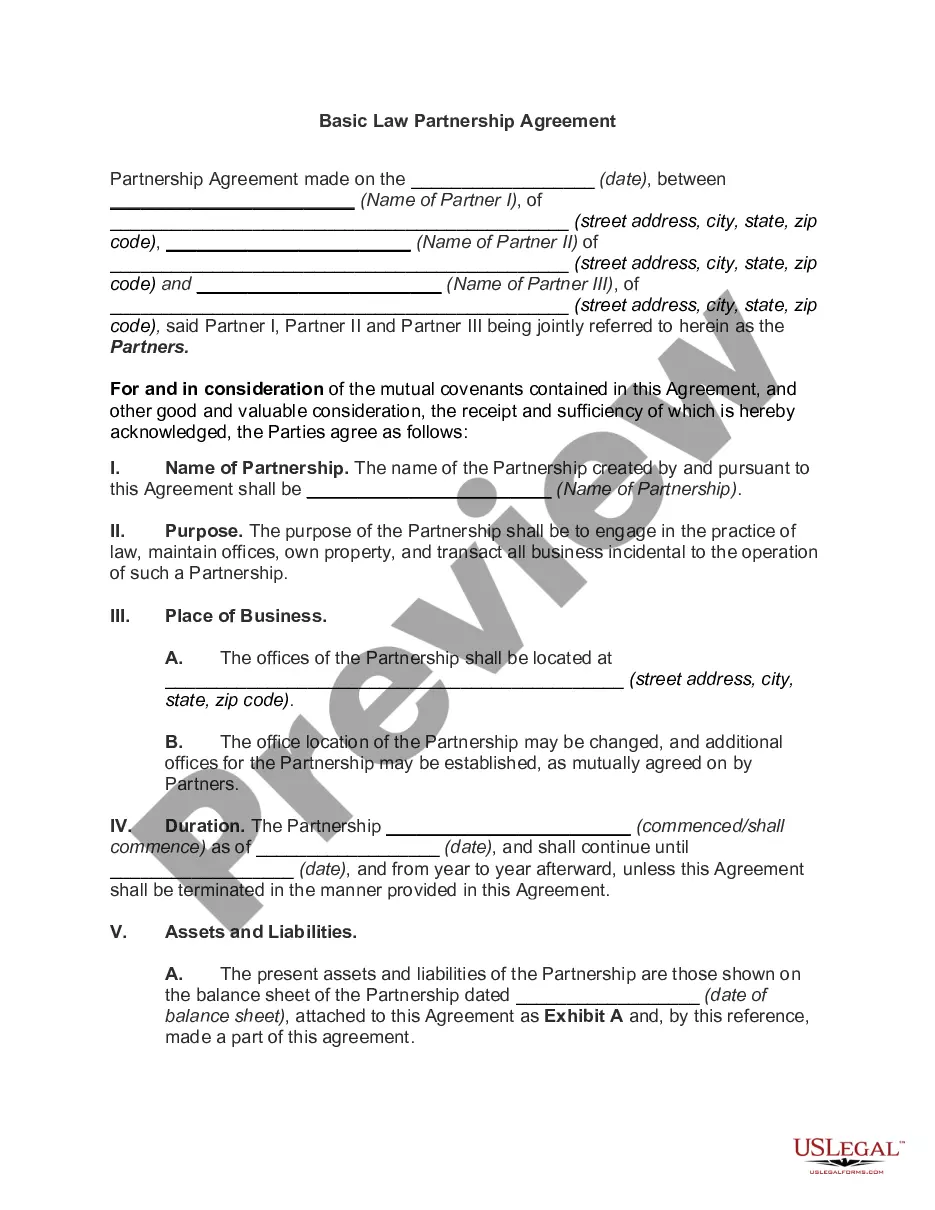
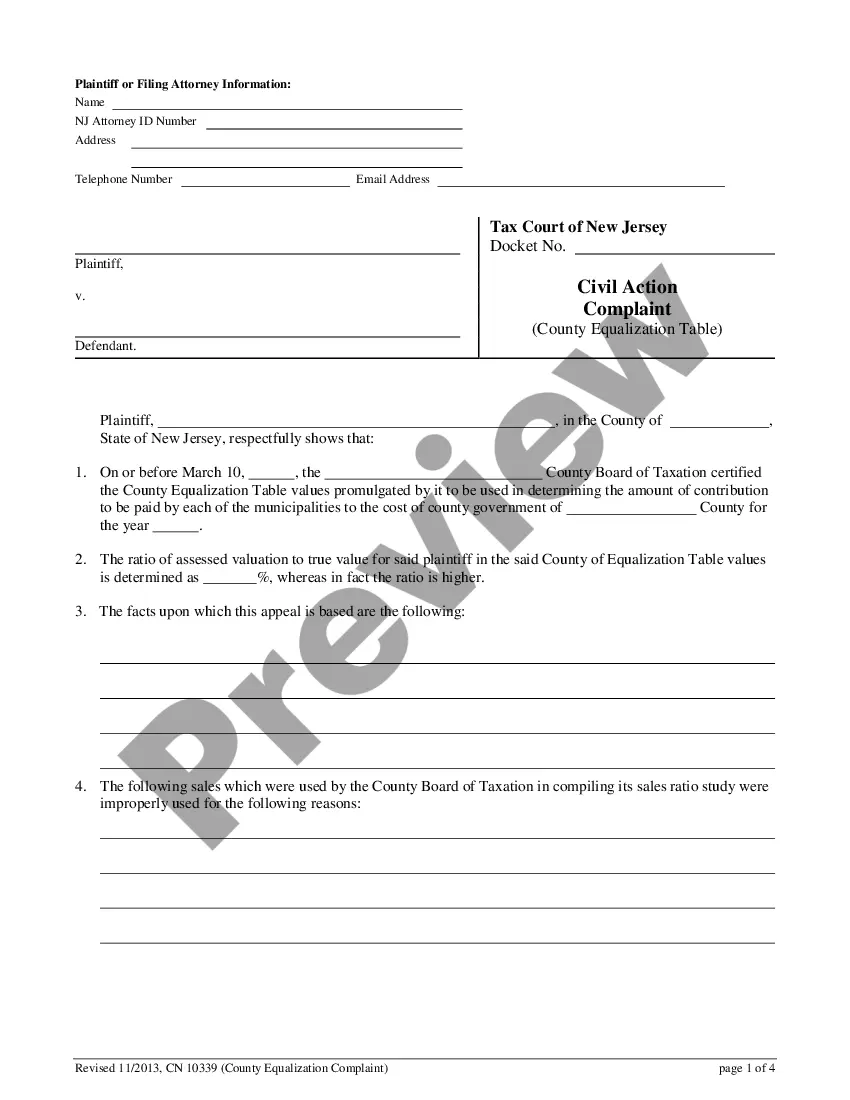
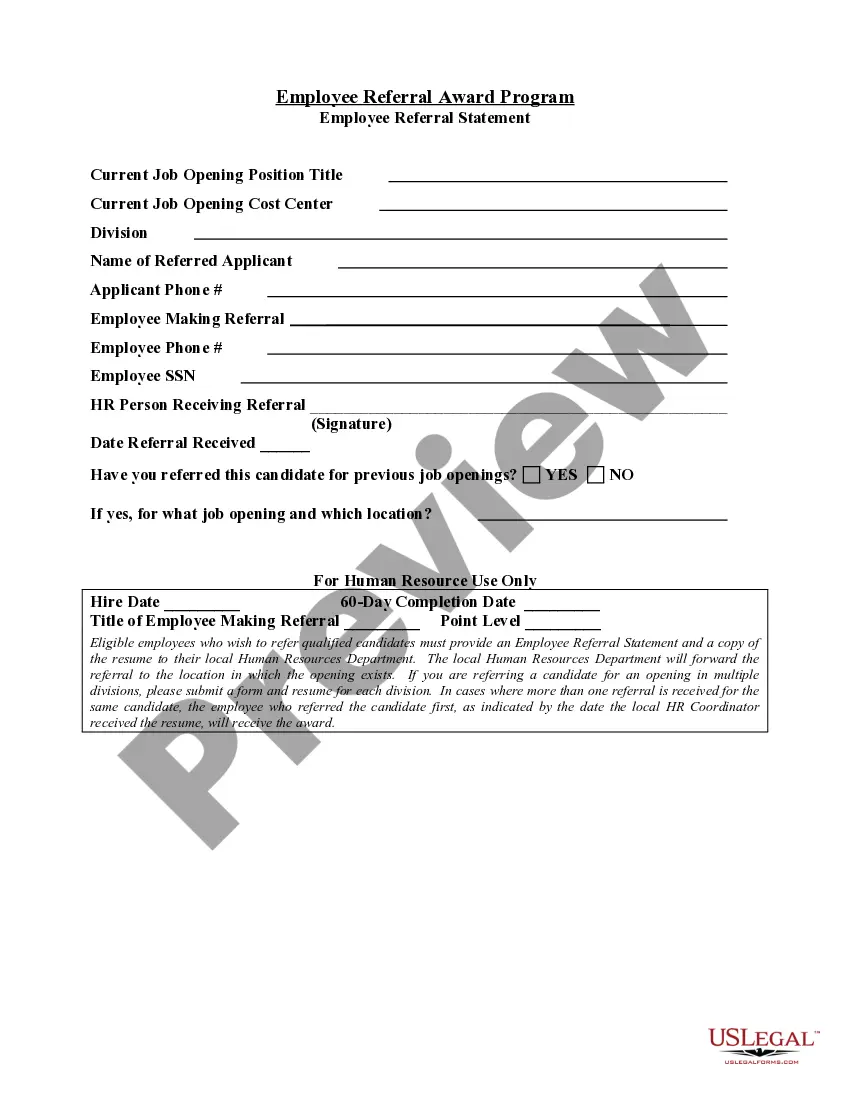
Preparing legal paperwork can be a real stress if you don’t have ready-to-use fillable templates. With the US Legal Forms online library of formal documentation, you can be confident in the blanks you obtain, as all of them comply with federal and state regulations and are examined by our specialists. So if you need to prepare Pennsylvania instructions for Completing Utilization Review Request, our service is the perfect place to download it.
Getting your Pennsylvania instructions for Completing Utilization Review Request from our service is as easy as ABC. Previously authorized users with a valid subscription need only sign in and click the Download button once they find the correct template. Afterwards, if they need to, users can take the same document from the My Forms tab of their profile. However, even if you are new to our service, signing up with a valid subscription will take only a few minutes. Here’s a brief guideline for you:
- Document compliance verification. You should carefully examine the content of the form you want and make sure whether it satisfies your needs and meets your state law requirements. Previewing your document and reviewing its general description will help you do just that.
- Alternative search (optional). If there are any inconsistencies, browse the library through the Search tab above until you find a suitable template, and click Buy Now once you see the one you want.
- Account registration and form purchase. Create an account with US Legal Forms. After account verification, log in and select your most suitable subscription plan. Make a payment to continue (PayPal and credit card options are available).
- Template download and further usage. Choose the file format for your Pennsylvania instructions for Completing Utilization Review Request and click Download to save it on your device. Print it to fill out your papers manually, or take advantage of a multi-featured online editor to prepare an electronic version faster and more efficiently.
Haven’t you tried US Legal Forms yet? Sign up for our service now to get any formal document quickly and easily any time you need to, and keep your paperwork in order!
Form popularity
FAQ
Utilization review (UR) is the process used by employers or claims administrators to review treatment to determine if it is medically necessary. All employers or their workers' compensation claims administrators are required by law to have a UR program.
In Pennsylvania, the statute of limitations for workers' compensation claims is three years from the date of injury. If you have been injured at work and denied either medical benefits or wage loss benefits under the workers' compensation law, you must file a Claim Petition within three years of the date of injury.
The utilization review process provides for the impartial review of the reasonableness or necessity of medical treatment rendered to, or proposed for, work-related injuries and illnesses.
The proposed employer assessment factor is 0.0318. This factor, in concert with the proposed employer assessment procedure, is subject to approval by the Insurance Commissioner.
Utilization reviews serve to evaluate each patient's care before, during and after procedures to ensure they receive adequate care throughout their hospital stay. Some UR nurses may oversee patient discharge and play a role in designing after-care plans, referred to as case management.