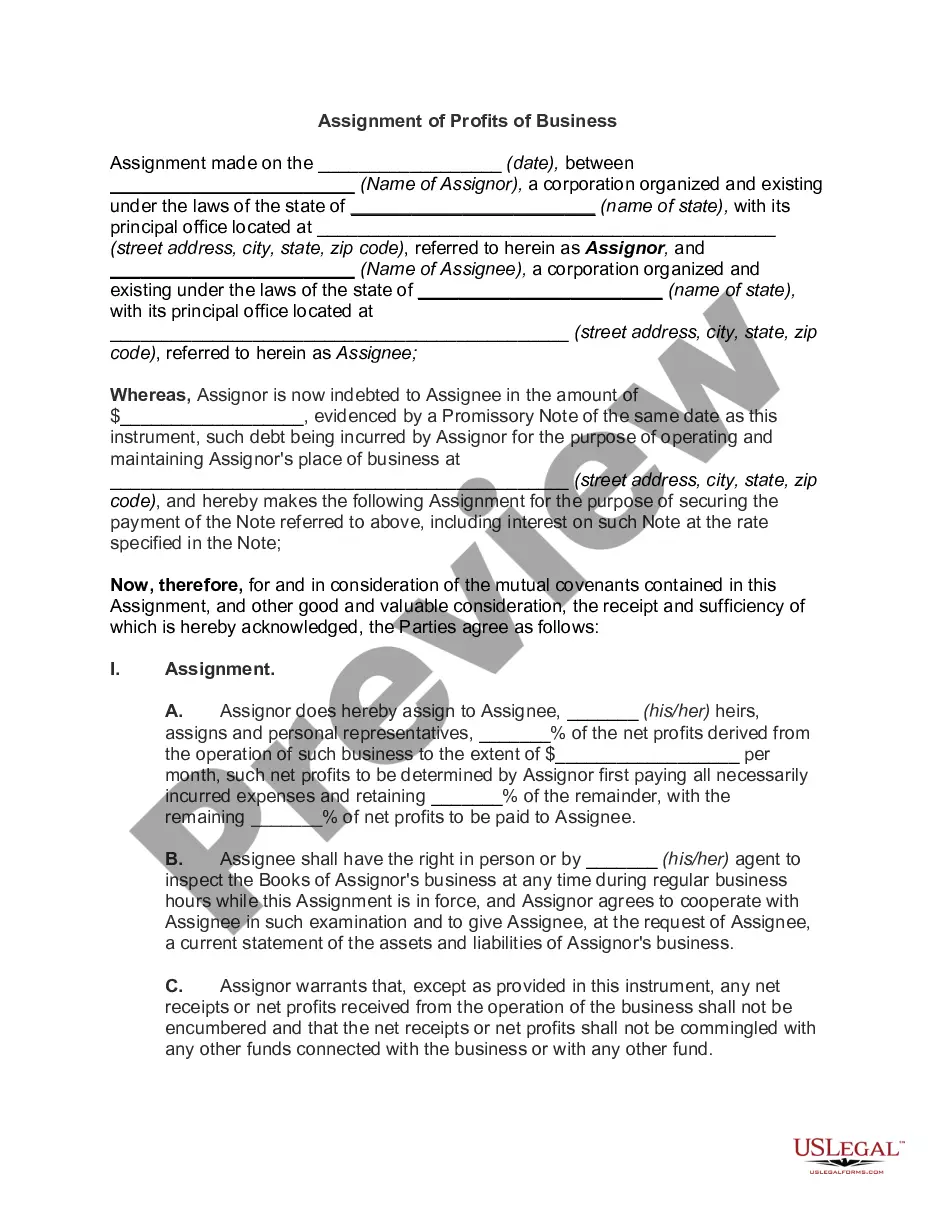
Pennsylvania COBRA Continuation Coverage Election Notice is a document that informs employees of their rights to continue their health insurance coverage under the Consolidated Omnibus Budget Reconciliation Act (COBRA). COBRA provides individuals with the option to continue their employer-sponsored health insurance for a limited period of time after experiencing a qualifying event such as job loss, reduction in work hours, or certain life events like divorce or death of a covered employee. The Pennsylvania COBRA Continuation Coverage Election Notice is a crucial document that outlines the specific eligibility criteria, deadlines, and procedures for individuals to elect and maintain their COBRA coverage. It describes the rights and obligations of both the employer and the qualified beneficiaries, ensuring they are aware of their options and responsibilities. This notice is generally provided by the employer or the group health plan administrator to employees and their covered dependents. The content of the Pennsylvania COBRA Continuation Coverage Election Notice typically includes the following relevant information: 1. Coverage Eligibility: The notice explains who is eligible for COBRA coverage, outlining the criteria and prerequisites for individuals to qualify for continuation coverage. 2. Qualifying Events: It details the specific situations or events that may trigger eligibility for COBRA, such as termination of employment, reduction in hours, or other qualifying events. 3. Notification Process: It provides information on how the qualified beneficiaries should notify the employer or plan administrator about a qualifying event in order to initiate the COBRA coverage process. 4. Coverage Period: The notice specifies the duration for which COBRA coverage can be maintained. Generally, it ranges from 18 to 36 months depending on the nature of the qualifying event. 5. Premium Payments: The notice provides details about the premium costs and payment methods required for COBRA coverage. It informs qualified beneficiaries about the payment schedule, due dates, and consequences of late payments or non-payment. 6. Alternative Coverage Options: The notice may explain alternative options available to individuals, such as purchasing coverage through the Health Insurance Marketplace or eligibility for other government programs. 7. Rights and Responsibilities: It outlines the rights and responsibilities of both employers and qualified beneficiaries under COBRA, ensuring compliance with the law and avoiding potential penalties. 8. Termination of Coverage: The notice specifies circumstances under which COBRA coverage may be terminated, such as failure to pay premiums, obtaining other group health coverage, or exhaustion of the maximum coverage period. It's important to note that while the content of the Pennsylvania COBRA Continuation Coverage Election Notice may vary slightly depending on specific plan details and employer requirements, the fundamental information remains the same. The purpose of the notice is to provide clear and comprehensive information to qualified beneficiaries, enabling them to make informed decisions regarding their health insurance coverage.
Pennsylvania COBRA Continuation Coverage Election Notice
Description
How to fill out Pennsylvania COBRA Continuation Coverage Election Notice?
If you need to full, acquire, or print out authorized file templates, use US Legal Forms, the greatest selection of authorized varieties, that can be found online. Use the site`s simple and easy handy search to get the documents you require. Different templates for company and personal uses are categorized by classes and states, or keywords. Use US Legal Forms to get the Pennsylvania COBRA Continuation Coverage Election Notice with a handful of clicks.
In case you are already a US Legal Forms client, log in in your bank account and then click the Download switch to obtain the Pennsylvania COBRA Continuation Coverage Election Notice. Also you can entry varieties you earlier saved in the My Forms tab of the bank account.
Should you use US Legal Forms for the first time, refer to the instructions below:
- Step 1. Be sure you have selected the form for the correct city/land.
- Step 2. Use the Review choice to check out the form`s information. Never overlook to read through the information.
- Step 3. In case you are unhappy with the type, use the Look for discipline on top of the monitor to find other variations from the authorized type design.
- Step 4. Upon having identified the form you require, click on the Acquire now switch. Select the rates prepare you favor and put your references to sign up on an bank account.
- Step 5. Process the financial transaction. You should use your charge card or PayPal bank account to accomplish the financial transaction.
- Step 6. Choose the structure from the authorized type and acquire it in your device.
- Step 7. Complete, modify and print out or indication the Pennsylvania COBRA Continuation Coverage Election Notice.
Every authorized file design you acquire is your own property for a long time. You might have acces to each and every type you saved inside your acccount. Click the My Forms segment and select a type to print out or acquire again.
Contend and acquire, and print out the Pennsylvania COBRA Continuation Coverage Election Notice with US Legal Forms. There are many expert and condition-distinct varieties you may use to your company or personal requires.
Form popularity
FAQ
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
COBRA costs an average of $599 per month. An Obamacare plan of similar quality costs $462 per monthbut 94% of people on HealthSherpa qualify for government subsidies, bringing the average cost down to $48 per month.
The federal COBRA law allows employees at larger businesses (20 or more employees) to purchase continuation health coverage after they leave employment for 18 months (or, in some cases, 36 months) after their employment ends.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
Pennsylvania's Mini-COBRA applies to employees of smaller businesses (2-19 employees), though it only allows for 9 months of coverage.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
COBRA continuation coverage lets you stay on your employer's group health insurance plan after leaving your job. COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. It's shorthand for the law change that required employers to extend temporary group health insurance to departing employees.