Pennsylvania Individual Notice of Preexisting Condition Exclusion refers to a legal document that outlines the provisions and conditions regarding preexisting medical conditions for individuals seeking health insurance coverage in the state of Pennsylvania. This notice is crucial for both insurance providers and policyholders as it informs individuals about the exclusionary periods and restrictions that may apply to their coverage based on their prior health condition. Under Pennsylvania law, there are several types of Individual Notice of Preexisting Condition Exclusions that insurance companies must adhere to: 1. Standard Exclusion Period: This type of exclusion imposes a specific time frame during which the insurance policy will not cover any expenses related to preexisting medical conditions. The length of the exclusion period can vary but usually lasts no longer than 12 months. 2. Look-Back Period: Insurance providers may conduct a review of an individual's medical history, known as the look-back period, to identify any preexisting conditions that may impact coverage. This period typically goes back five years, but it can vary depending on the policy. 3. Creditable Coverage Exemption: If an individual can provide evidence of prior creditable health insurance coverage, they may be exempt from the preexisting condition exclusion period. Creditable coverage includes most types of insurance, such as group health plans, individual health insurance, and government programs like Medicaid or Medicare. 4. Continuous Coverage Exemption: This exemption applies to individuals who have maintained continuous health insurance coverage without a significant gap in coverage. By continuously being insured, individuals may be able to bypass the preexisting condition exclusion, as long as they do not experience a break in coverage exceeding 63 days. Understanding the Pennsylvania Individual Notice of Preexisting Condition Exclusion is crucial for both insurance companies and individuals seeking coverage. Insurance providers must clearly communicate these exclusionary periods and restrictions to policyholders to ensure they are aware of any limitations on their coverage. Conversely, individuals should carefully review and understand the notice before purchasing a policy to fully comprehend how their preexisting conditions may impact their access to healthcare services.
Pennsylvania Individual Notice of Preexisting Condition Exclusion
Description
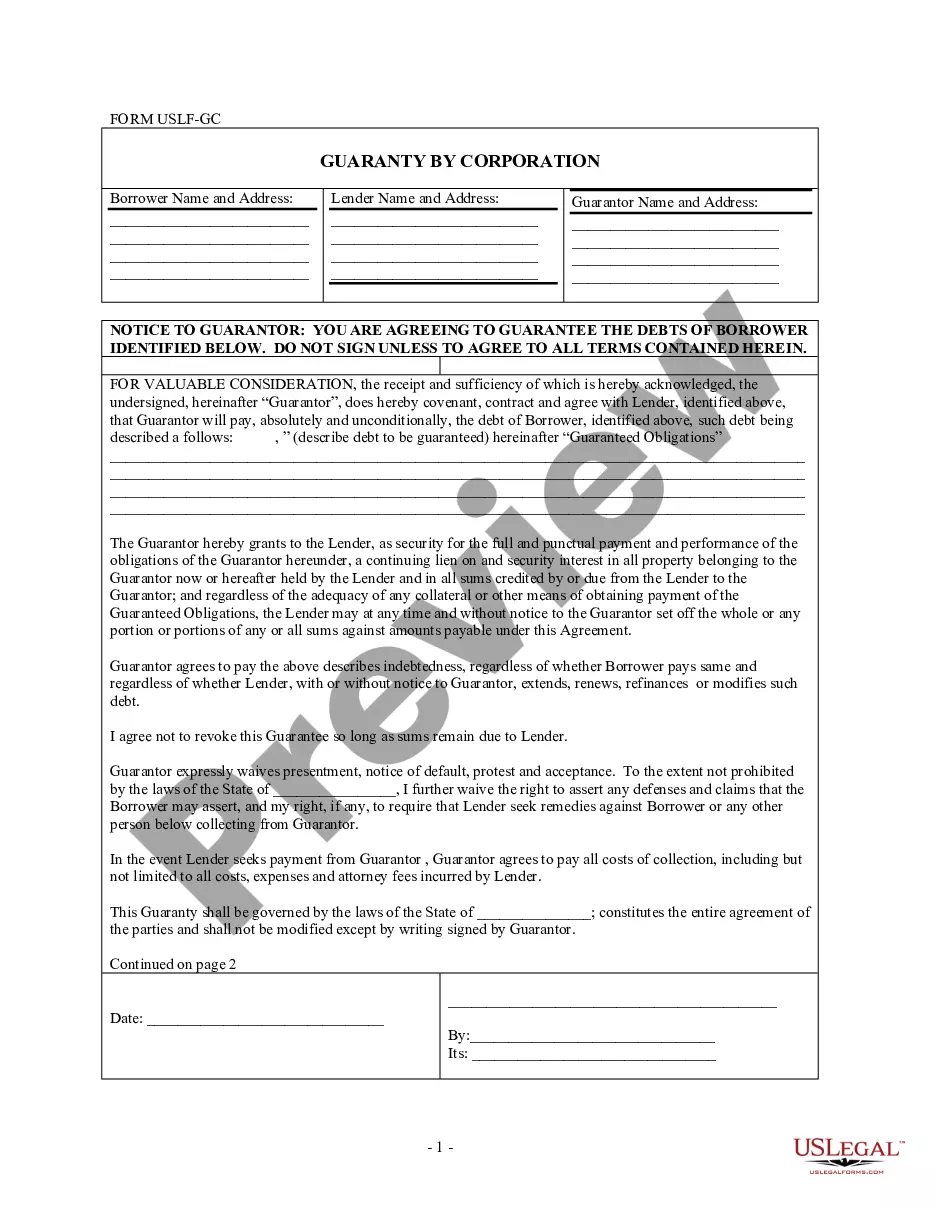
How to fill out Pennsylvania Individual Notice Of Preexisting Condition Exclusion?
If you want to complete, obtain, or print out lawful papers layouts, use US Legal Forms, the biggest variety of lawful varieties, that can be found on the Internet. Use the site`s simple and convenient research to discover the paperwork you need. Various layouts for enterprise and individual uses are categorized by types and says, or key phrases. Use US Legal Forms to discover the Pennsylvania Individual Notice of Preexisting Condition Exclusion in just a handful of mouse clicks.
Should you be presently a US Legal Forms customer, log in in your accounts and click on the Acquire option to have the Pennsylvania Individual Notice of Preexisting Condition Exclusion. Also you can gain access to varieties you formerly delivered electronically from the My Forms tab of your accounts.
Should you use US Legal Forms for the first time, refer to the instructions below:
- Step 1. Be sure you have chosen the form to the proper town/country.
- Step 2. Take advantage of the Preview choice to look over the form`s articles. Never neglect to read the outline.
- Step 3. Should you be unhappy with all the develop, use the Research field at the top of the display screen to locate other types of your lawful develop design.
- Step 4. After you have identified the form you need, select the Get now option. Choose the costs program you prefer and add your credentials to register for an accounts.
- Step 5. Process the deal. You should use your charge card or PayPal accounts to accomplish the deal.
- Step 6. Choose the formatting of your lawful develop and obtain it on the product.
- Step 7. Full, revise and print out or signal the Pennsylvania Individual Notice of Preexisting Condition Exclusion.
Each lawful papers design you buy is your own property forever. You might have acces to every develop you delivered electronically inside your acccount. Click the My Forms area and select a develop to print out or obtain once more.
Be competitive and obtain, and print out the Pennsylvania Individual Notice of Preexisting Condition Exclusion with US Legal Forms. There are millions of expert and condition-specific varieties you can utilize for your personal enterprise or individual needs.