Rhode Island Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
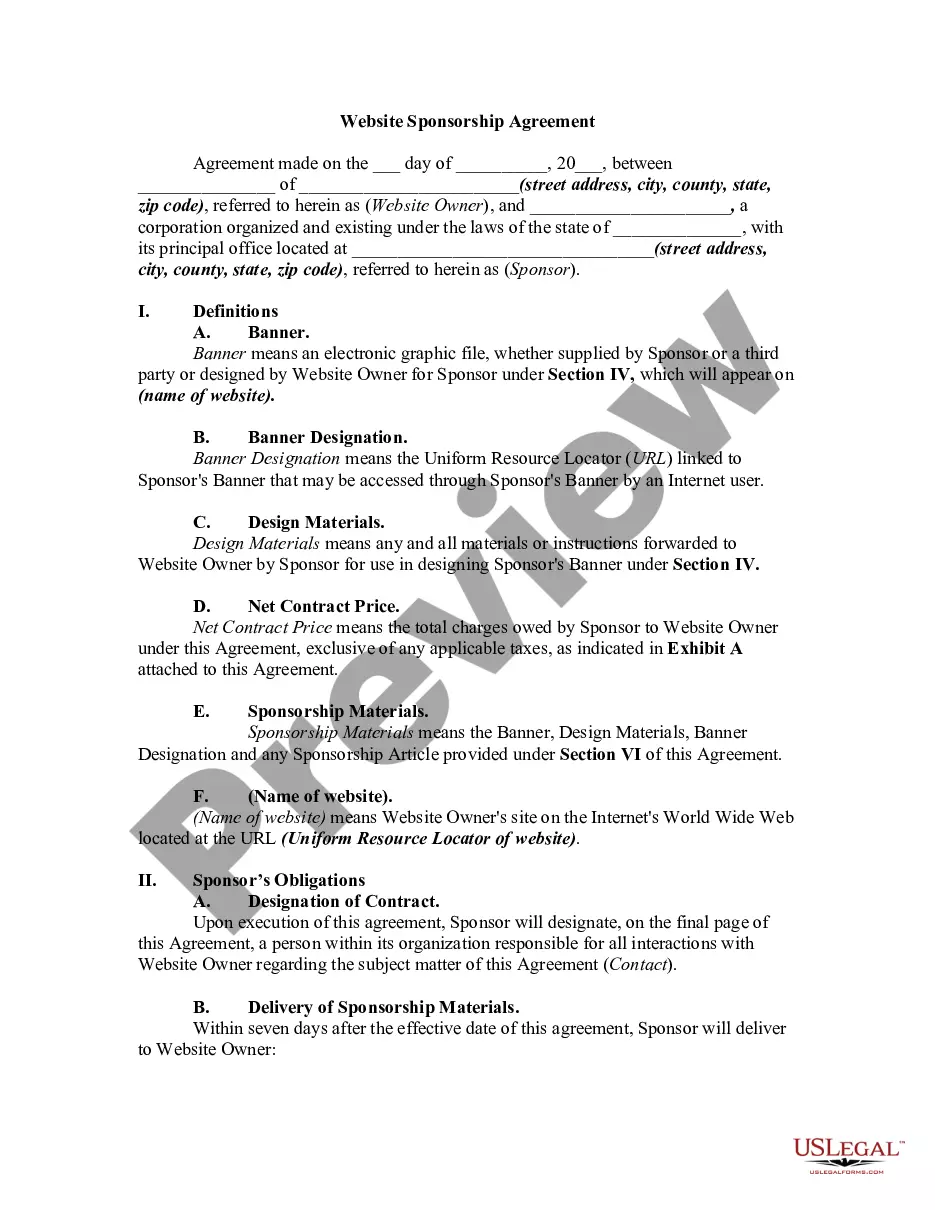
US Legal Forms - one of the greatest libraries of legal forms in the United States - delivers a wide range of legal document layouts you can acquire or print out. Making use of the site, you can find 1000s of forms for organization and specific uses, categorized by types, claims, or keywords and phrases.You will find the newest versions of forms like the Rhode Island Notice from Employer to Employee Regarding Early Termination of Continuation Coverage within minutes.
If you already possess a membership, log in and acquire Rhode Island Notice from Employer to Employee Regarding Early Termination of Continuation Coverage through the US Legal Forms catalogue. The Down load option will show up on each and every form you perspective. You have accessibility to all in the past downloaded forms within the My Forms tab of your profile.
If you wish to use US Legal Forms the very first time, here are simple recommendations to obtain started out:
- Ensure you have picked out the right form for your area/state. Click the Preview option to check the form`s content. See the form explanation to ensure that you have chosen the appropriate form.
- When the form doesn`t satisfy your requirements, make use of the Lookup area towards the top of the monitor to find the one who does.
- In case you are happy with the shape, validate your option by simply clicking the Purchase now option. Then, pick the costs prepare you like and provide your references to sign up for an profile.
- Method the purchase. Make use of your charge card or PayPal profile to accomplish the purchase.
- Select the structure and acquire the shape on the device.
- Make adjustments. Fill out, edit and print out and signal the downloaded Rhode Island Notice from Employer to Employee Regarding Early Termination of Continuation Coverage.
Each and every web template you put into your money does not have an expiry time and is your own forever. So, if you want to acquire or print out an additional backup, just proceed to the My Forms area and click about the form you want.
Get access to the Rhode Island Notice from Employer to Employee Regarding Early Termination of Continuation Coverage with US Legal Forms, one of the most comprehensive catalogue of legal document layouts. Use 1000s of skilled and state-distinct layouts that meet your small business or specific requires and requirements.
Form popularity
FAQ
Rhode Island is an employment-at-will state, which means that without a written employee contract, employees can be terminated for any reason at any time, provided that the reason is not discriminatory and that the employer is not retaliating against the employee for a rightful action.
Initial COBRA notices must generally be provided within 14 days of the employer notifying the third-party administrator (TPA) of a qualifying event.
Meet the Deadlines You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
Rhode Island is an employment-at-will state, which means that without a written employee contract, employees can be terminated for any reason at any time, provided that the reason is not discriminatory and that the employer is not retaliating against the employee for a rightful action.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA) amended the Public Health Service Act, the Internal Revenue Code and the Employee Retirement Income Security Act (ERISA) to require employers with 20 or more employees to provide temporary continuation of group health coverage in certain situations
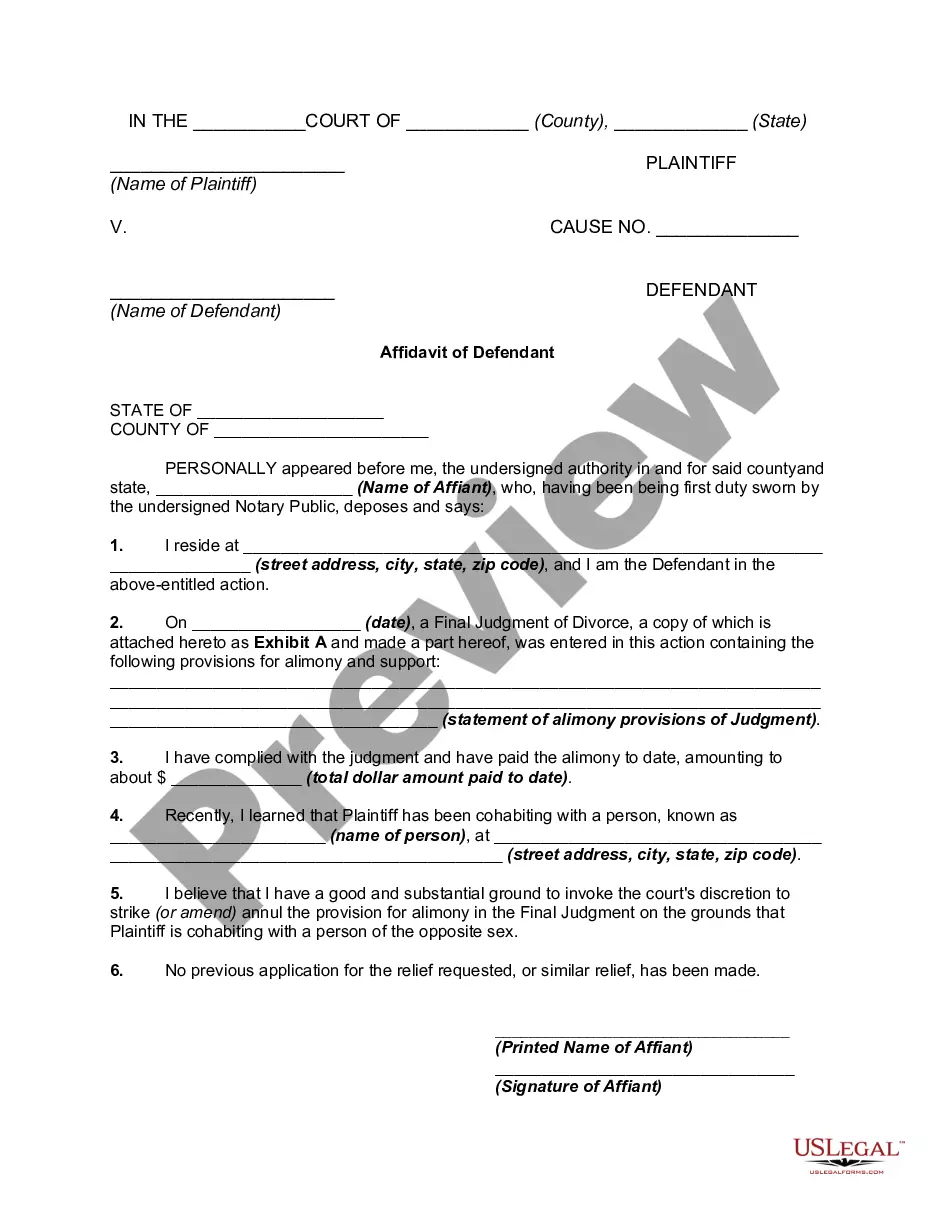
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
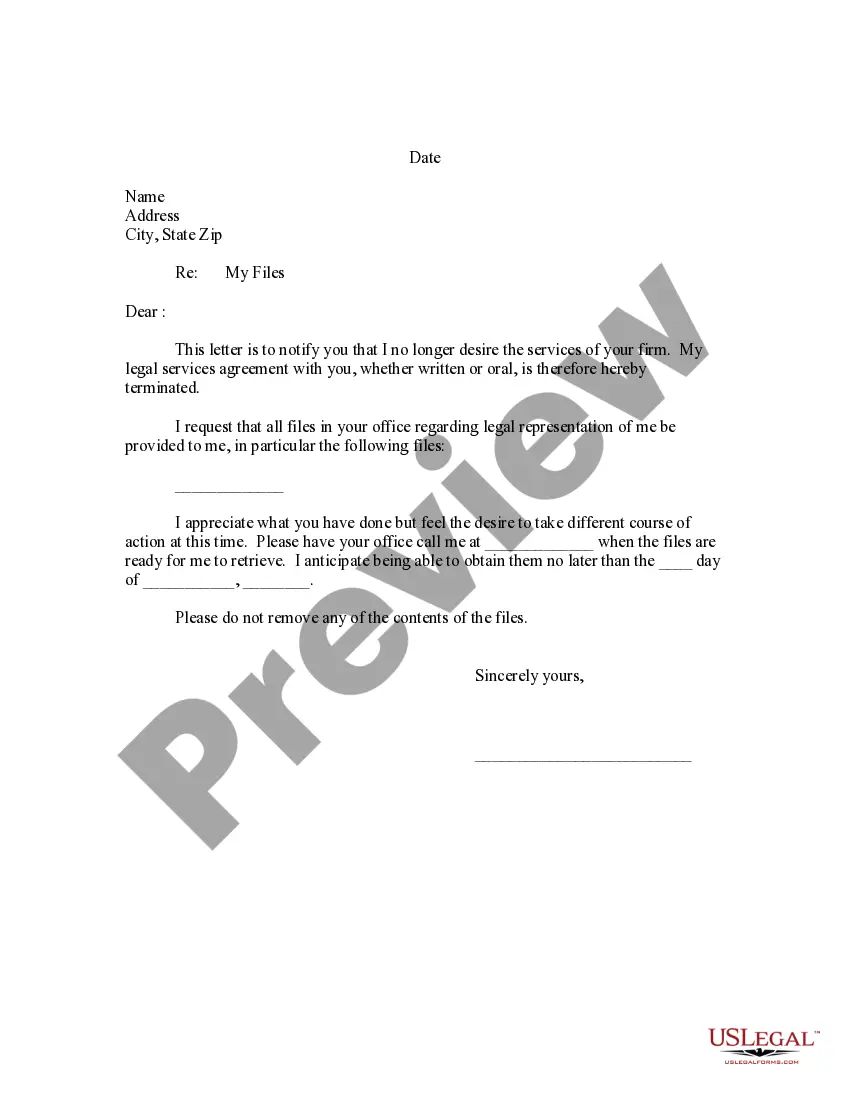
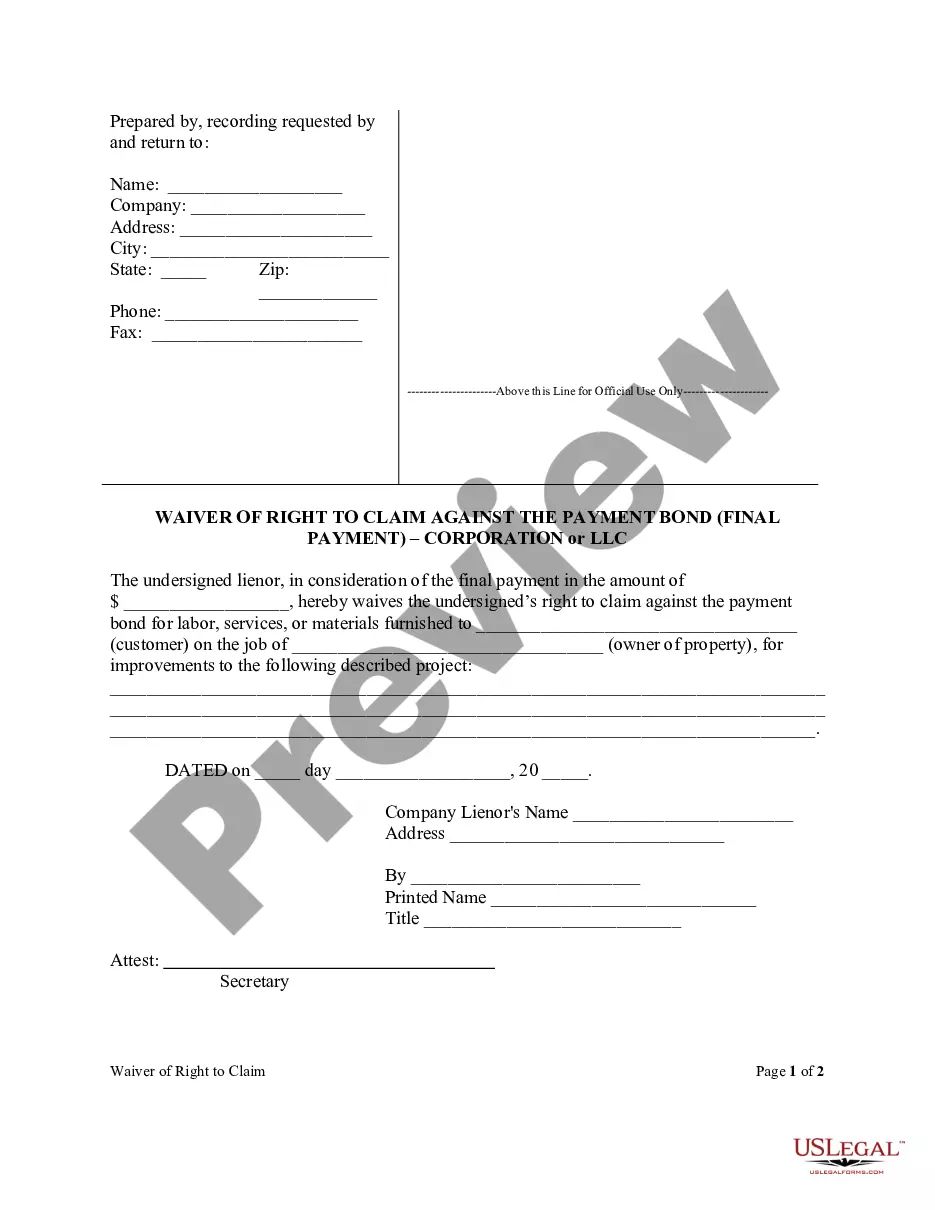
COBRA Notice of Early Termination of Continuation Coverage Continuation coverage must generally be made available for a maximum period (18, 29, or 36 months).
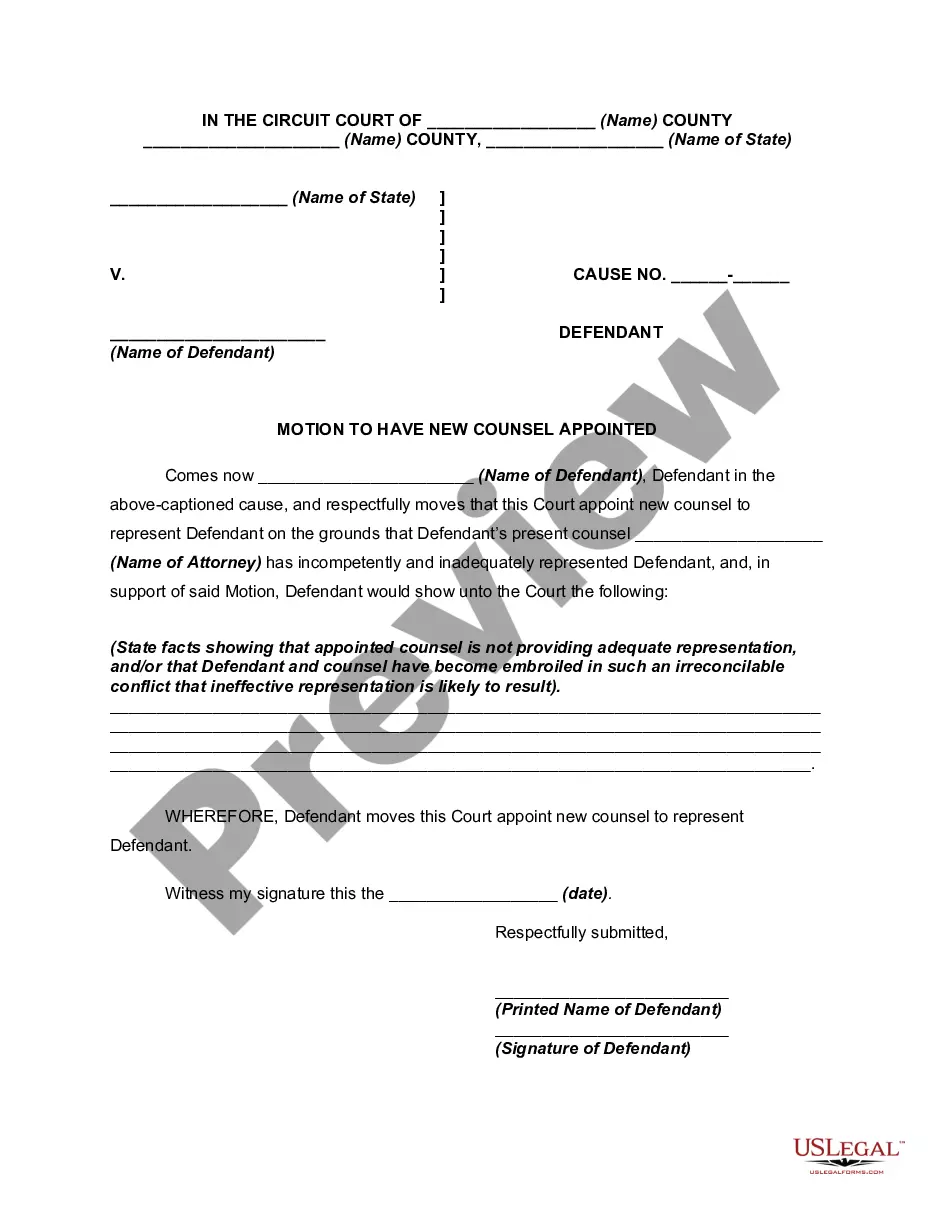
Federally, and in most states, a termination letter is not legally required. In some states, currently including Arizona, California, Illinois and New Jersey, written termination notices are required by law. Some of these states have specific templates employers must use for the letter.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.