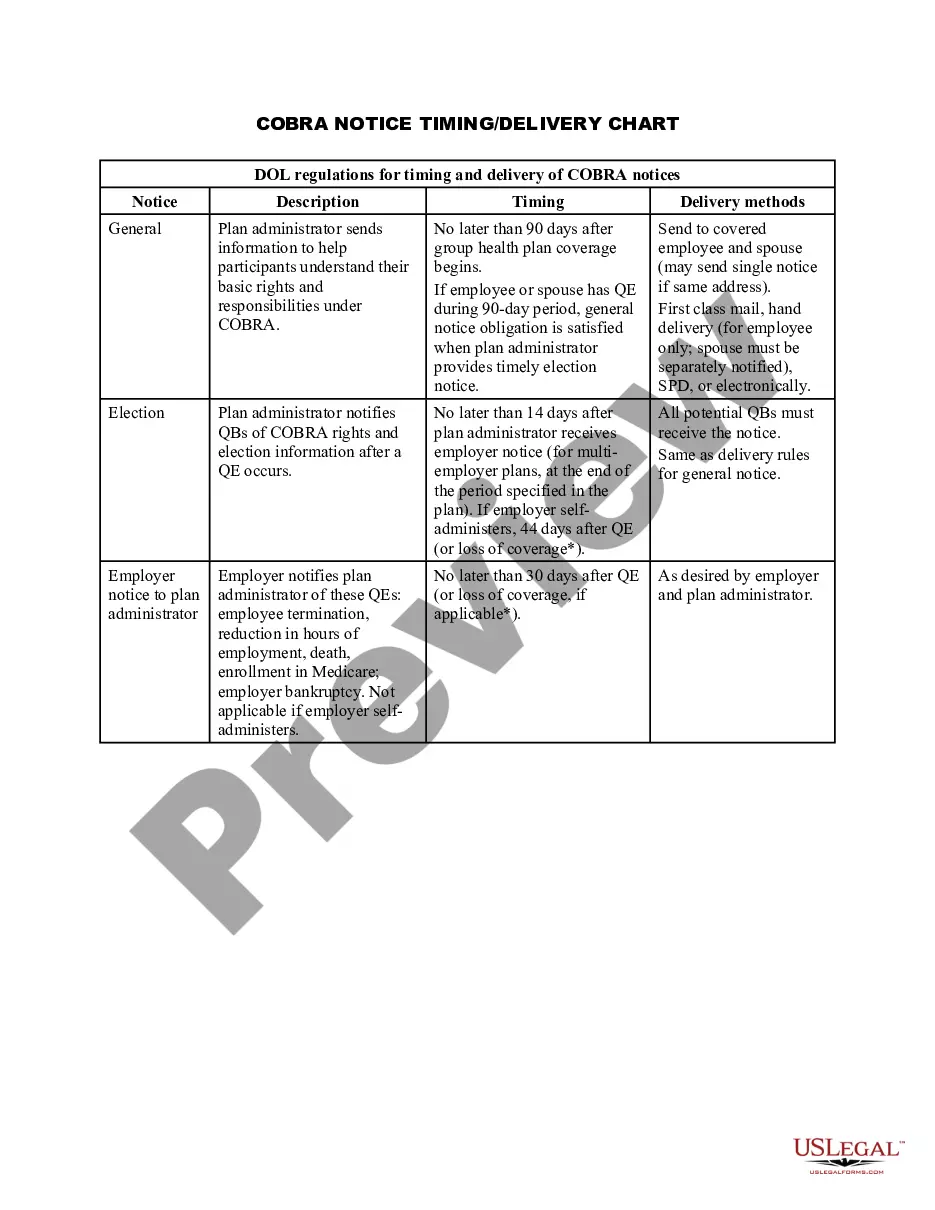
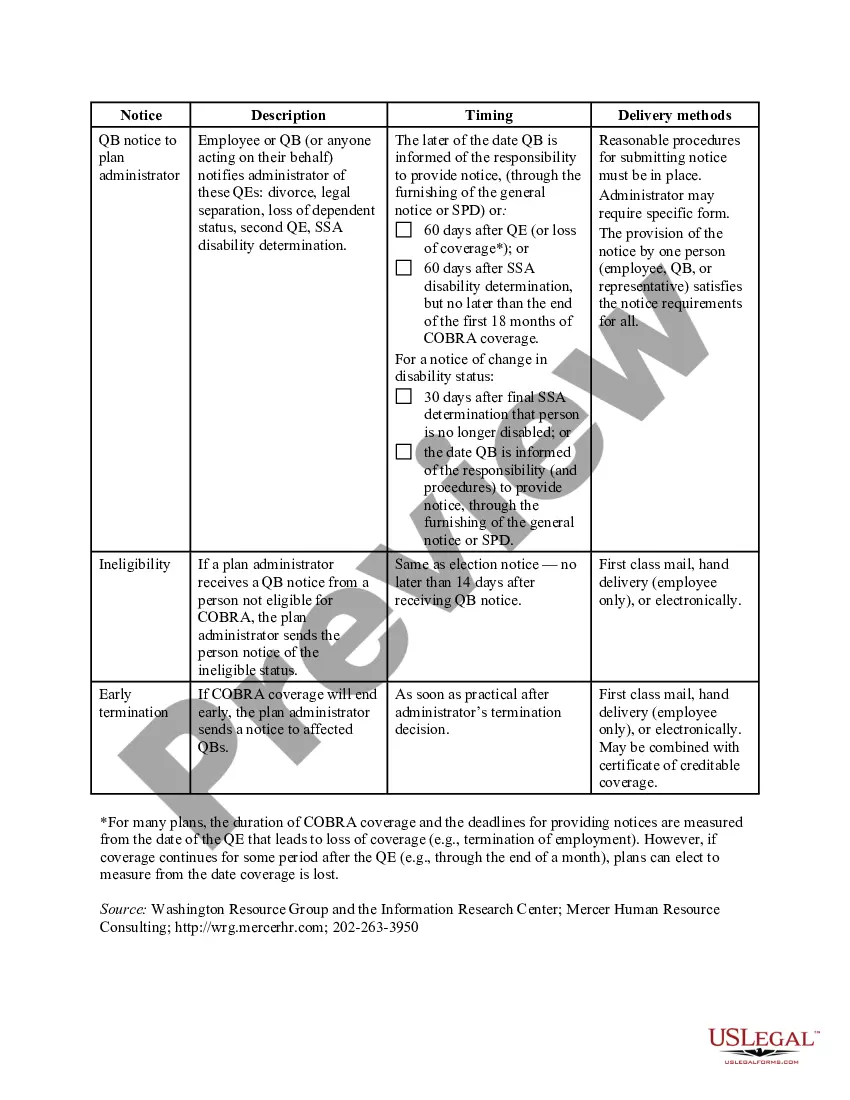
Rhode Island COBRA Notice Timing Delivery Chart is a document that provides important information regarding the timing and delivery requirements for COBRA notices in Rhode Island. COBRA, which stands for Consolidated Omnibus Budget Reconciliation Act, is a federal law that allows certain employees and their dependents to continue their health insurance coverage for a limited period of time after experiencing a qualifying event that would otherwise result in loss of coverage. Rhode Island, like other states, has specific regulations regarding the timing and delivery of COBRA notices. The Rhode Island COBRA Notice Timing Delivery Chart outlines the specific requirements that employers must follow when providing COBRA notices to their employees and beneficiaries. This chart is designed to ensure that individuals who are eligible for COBRA coverage receive the necessary information in a timely manner. It helps employers understand the exact timelines and deadlines they must adhere to in order to comply with state regulations. The chart highlights various types of COBRA notices that need to be delivered within specific timeframes. Some different types of Rhode Island COBRA notices include: 1. General Notice: This notice is typically provided to all covered employees and their dependents when they initially become eligible for group health insurance coverage. It explains the rights and responsibilities under COBRA and provides information on how to elect COBRA benefits if a qualifying event occurs. 2. Qualifying Event Notice: This notice is sent to employees and beneficiaries within a specified time after a qualifying event occurs, such as termination of employment or reduction in work hours. It informs them of their eligibility for COBRA continuation coverage and provides details on how to elect coverage. 3. Election Notice: This notice is sent to eligible individuals who have experienced a qualifying event, providing them with the opportunity to elect COBRA coverage. It outlines the coverage options available, the cost of coverage, and the deadline for making an election. 4. Premium Notice: This notice is sent to individuals enrolled in COBRA coverage on a monthly basis, informing them of the premium due, the due date, and any applicable grace period. 5. Termination Notice: This notice is sent to individuals whose COBRA coverage is being terminated. It provides information on the reasons for termination and any alternative coverage options that may be available. By following the guidelines outlined in the Rhode Island COBRA Notice Timing Delivery Chart, employers can ensure that they comply with state regulations and provide the necessary information to their employees and beneficiaries in a timely manner. It is essential for employers to understand and adhere to these requirements to avoid any penalties or legal issues related to COBRA compliance in Rhode Island.
Rhode Island COBRA Notice Timing Delivery Chart
Description
How to fill out Rhode Island COBRA Notice Timing Delivery Chart?
You are able to devote time on the Internet looking for the legal record design that meets the federal and state requirements you want. US Legal Forms offers 1000s of legal types that are reviewed by professionals. It is simple to obtain or printing the Rhode Island COBRA Notice Timing Delivery Chart from the assistance.
If you already have a US Legal Forms account, it is possible to log in and then click the Obtain button. Afterward, it is possible to complete, modify, printing, or signal the Rhode Island COBRA Notice Timing Delivery Chart. Every single legal record design you get is the one you have permanently. To obtain another copy of any obtained kind, go to the My Forms tab and then click the related button.
If you are using the US Legal Forms internet site the very first time, stick to the straightforward instructions listed below:
- Very first, make sure that you have selected the proper record design for that state/city that you pick. Browse the kind information to make sure you have picked out the right kind. If available, make use of the Review button to appear from the record design as well.
- If you want to get another version of your kind, make use of the Search discipline to obtain the design that fits your needs and requirements.
- Upon having found the design you desire, click Buy now to proceed.
- Select the rates prepare you desire, key in your references, and sign up for a free account on US Legal Forms.
- Complete the deal. You can utilize your Visa or Mastercard or PayPal account to pay for the legal kind.
- Select the format of your record and obtain it to the system.
- Make modifications to the record if needed. You are able to complete, modify and signal and printing Rhode Island COBRA Notice Timing Delivery Chart.
Obtain and printing 1000s of record templates while using US Legal Forms website, which offers the greatest selection of legal types. Use skilled and condition-distinct templates to deal with your small business or individual demands.