South Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
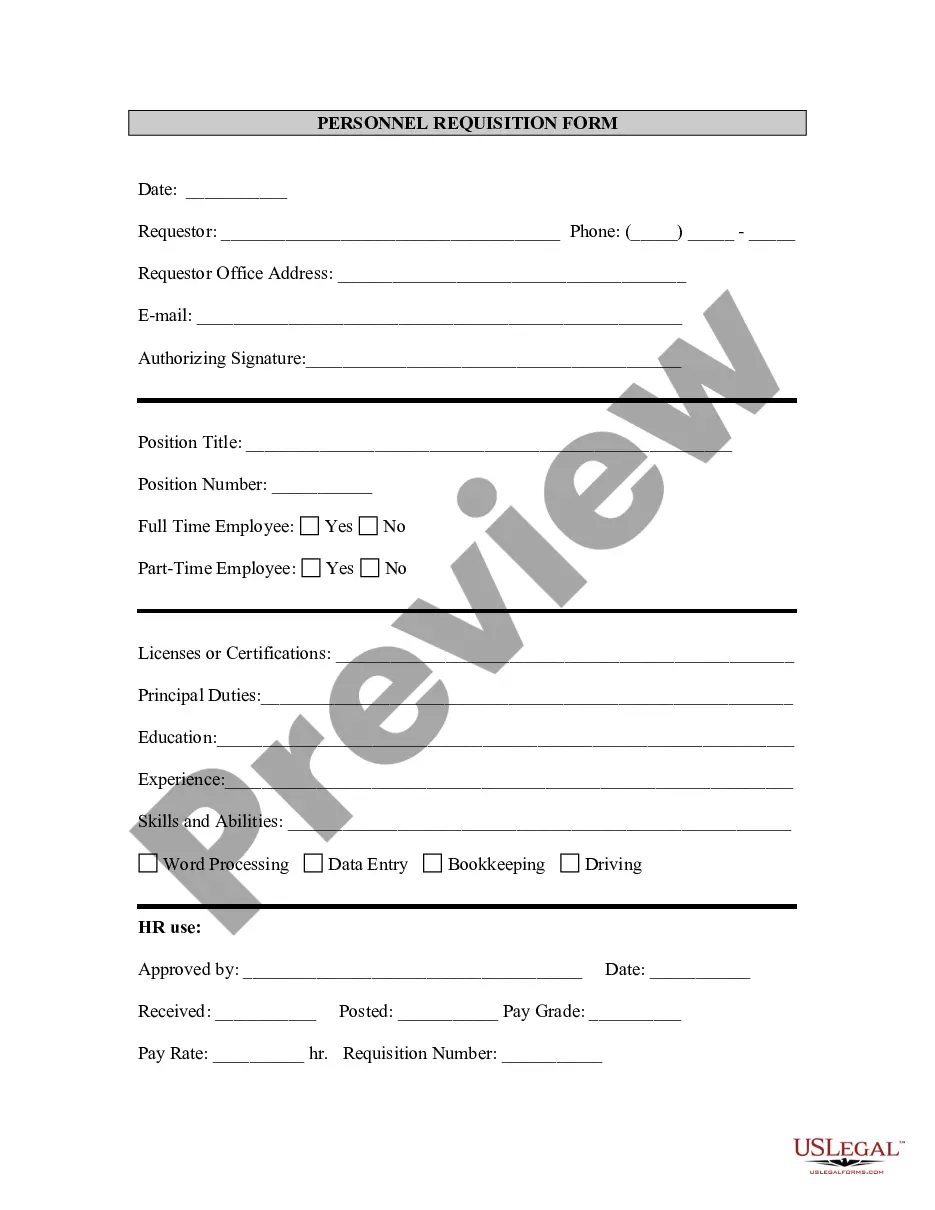
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
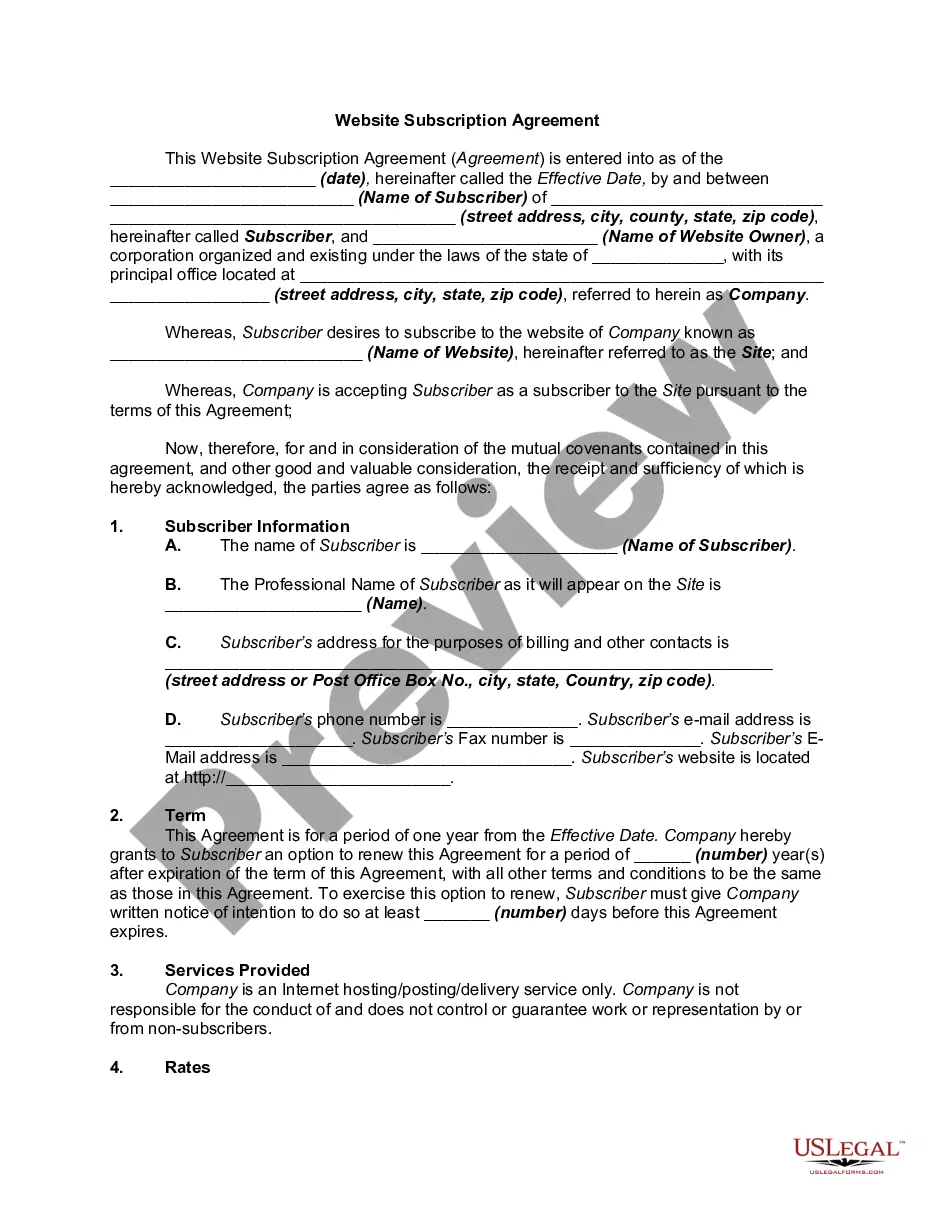
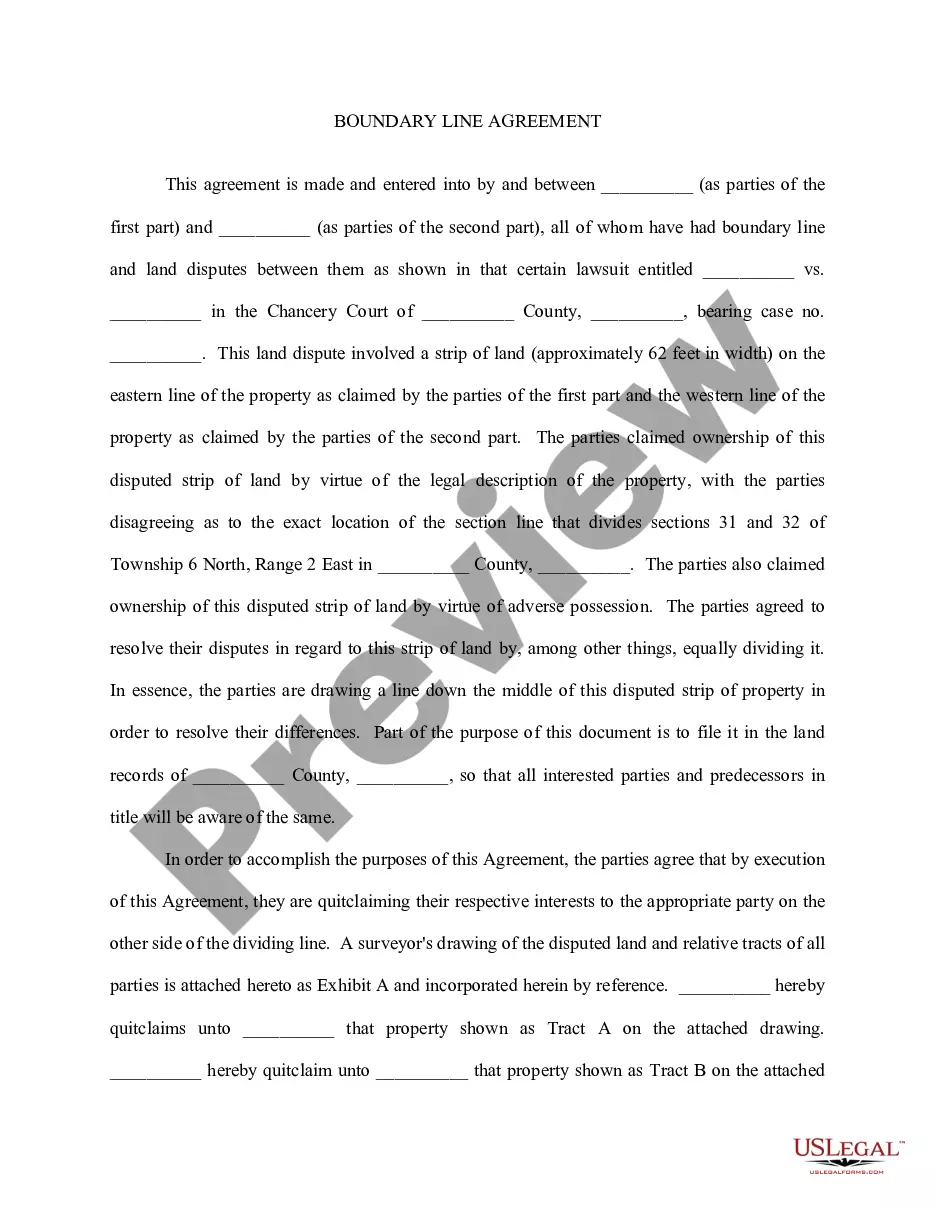
US Legal Forms - one of the biggest libraries of lawful forms in the United States - provides an array of lawful file layouts you are able to obtain or produce. Utilizing the internet site, you can find a large number of forms for organization and individual purposes, categorized by classes, suggests, or keywords.You will find the newest types of forms such as the South Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage in seconds.
If you have a monthly subscription, log in and obtain South Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage from the US Legal Forms collection. The Download option will appear on each and every type you perspective. You gain access to all formerly acquired forms in the My Forms tab of the bank account.
If you would like use US Legal Forms the very first time, listed here are basic directions to help you get started:
- Be sure you have selected the right type to your town/region. Click the Preview option to examine the form`s content material. Look at the type description to ensure that you have selected the appropriate type.
- When the type does not satisfy your specifications, utilize the Search industry towards the top of the display screen to discover the the one that does.
- If you are pleased with the shape, confirm your option by clicking the Purchase now option. Then, choose the pricing program you favor and provide your qualifications to register for the bank account.
- Method the purchase. Make use of credit card or PayPal bank account to perform the purchase.
- Choose the structure and obtain the shape on the gadget.
- Make modifications. Complete, modify and produce and indicator the acquired South Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage.
Each and every format you put into your money does not have an expiry particular date and is also your own permanently. So, if you want to obtain or produce one more copy, just proceed to the My Forms segment and click about the type you want.
Gain access to the South Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage with US Legal Forms, by far the most substantial collection of lawful file layouts. Use a large number of professional and status-particular layouts that satisfy your business or individual needs and specifications.
Form popularity
FAQ
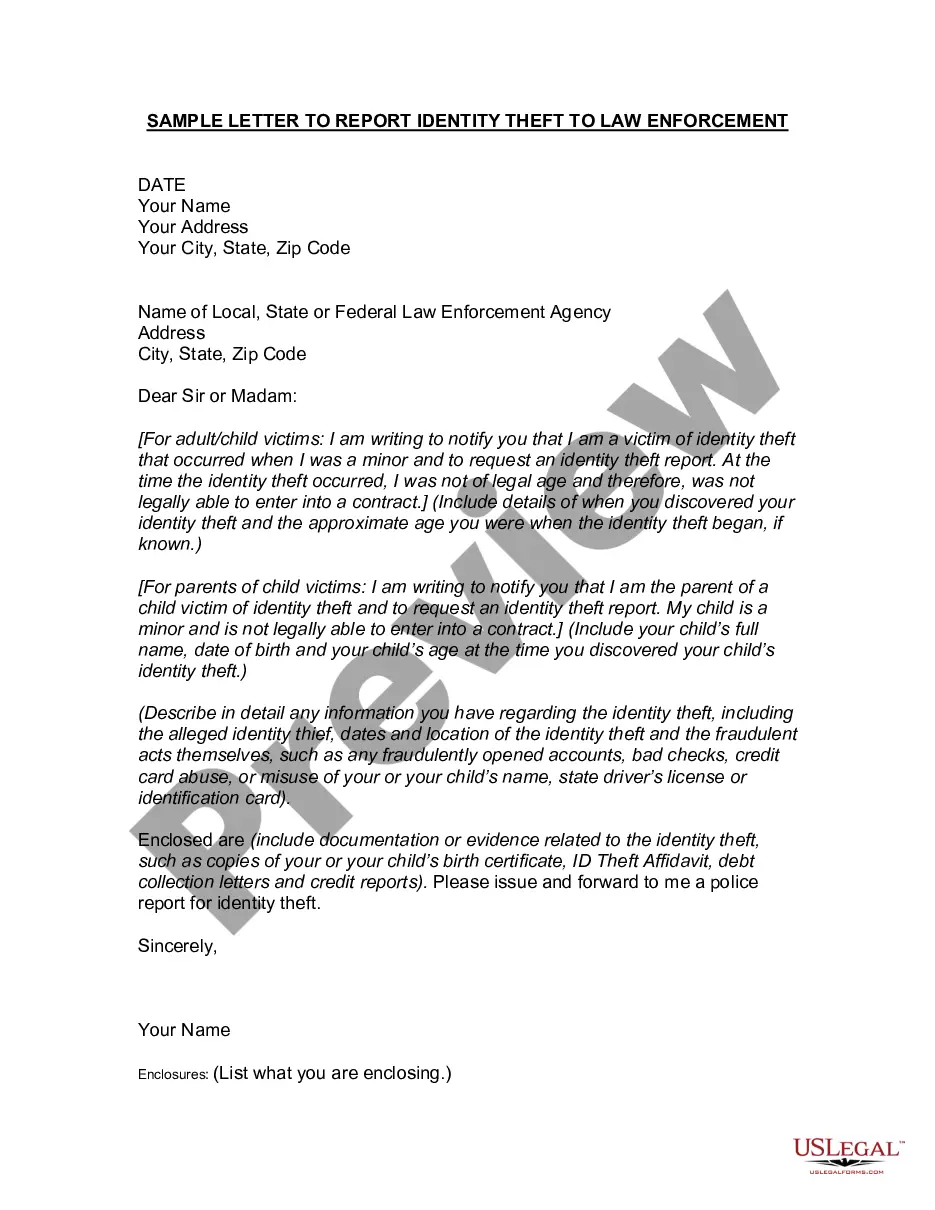
The Consolidated Omnibus Budget Reconciliation Act, known as COBRA, is a federal law that allows employees to continue their employer-provided health insurance after they are laid off or fired, or they otherwise become ineligible for benefits (for example, because they quit or their hours are reduced below the
Under COBRA, if you leave your current job, you have the option to continue your health care coverage for up to 18 months. You are required to pay the full premium yourself, even if your employer paid part of your premium while you were employed, and the employer may charge an additional, limited administrative fee.
Meet the Deadlines You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
Initial COBRA notices must generally be provided within 14 days of the employer notifying the third-party administrator (TPA) of a qualifying event.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
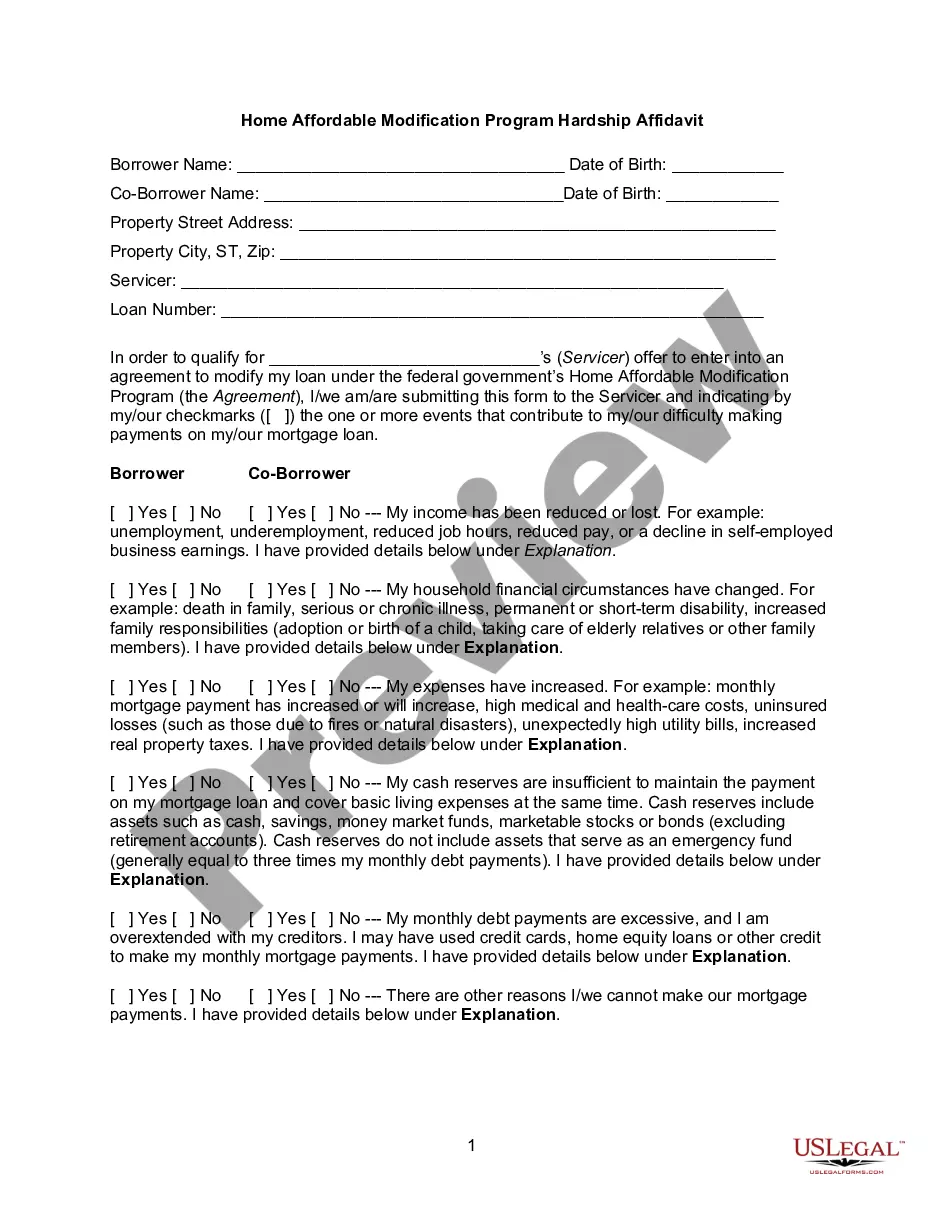
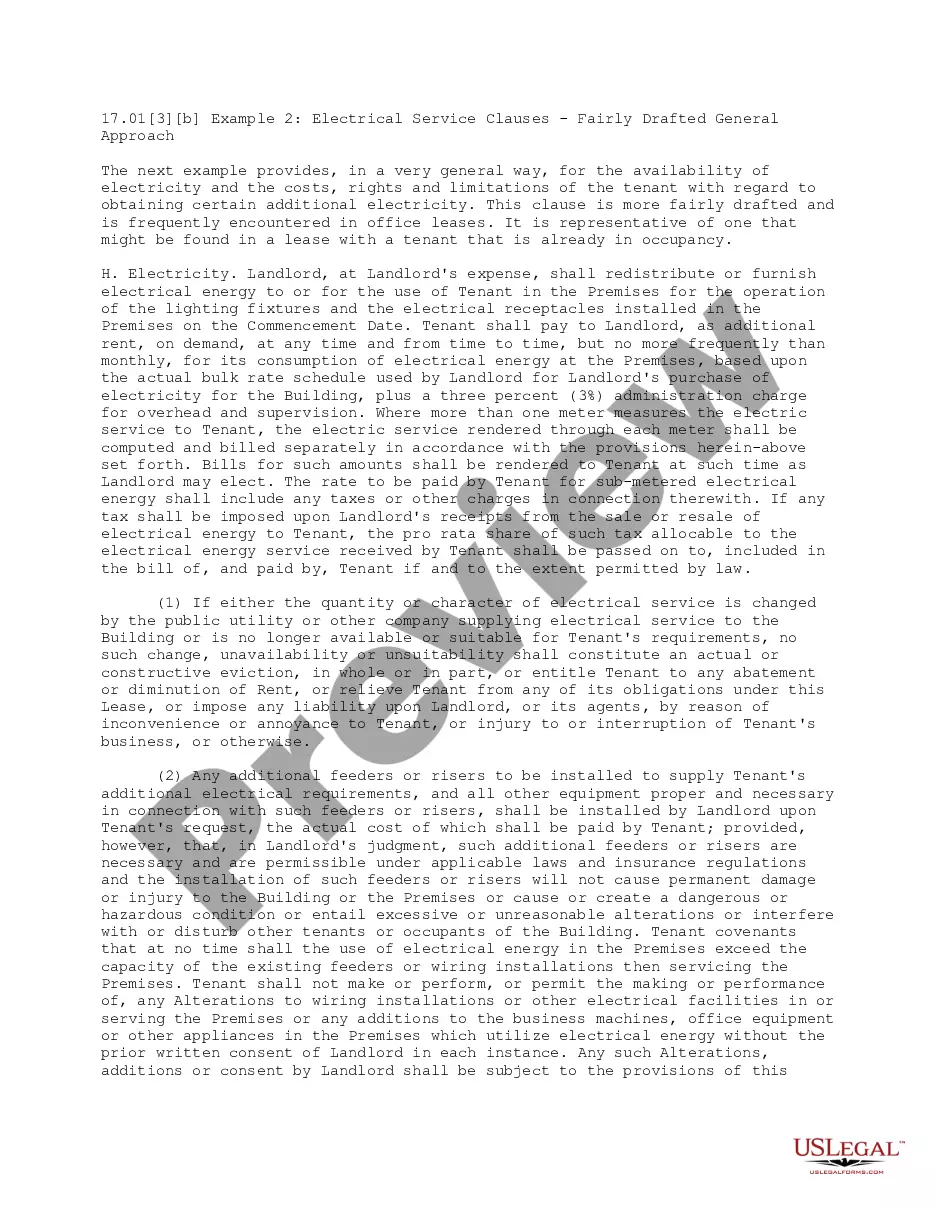
COBRA Notice of Early Termination of Continuation Coverage Continuation coverage must generally be made available for a maximum period (18, 29, or 36 months).
On Average, The Monthly COBRA Premium Cost Is $400 700 Per Person. Continuing on an employer's major medical health plan with COBRA is expensive. You are now responsible for the entire insurance premium, whereas your previous employer subsidized a portion of that as a work benefit.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
COBRA generally applies to all private-sector group health plans maintained by employers that have at least 20 employees on more than 50 percent of its typical business days in the previous calendar year. Both full- and part-time employees are counted to determine whether a plan is subject to COBRA.