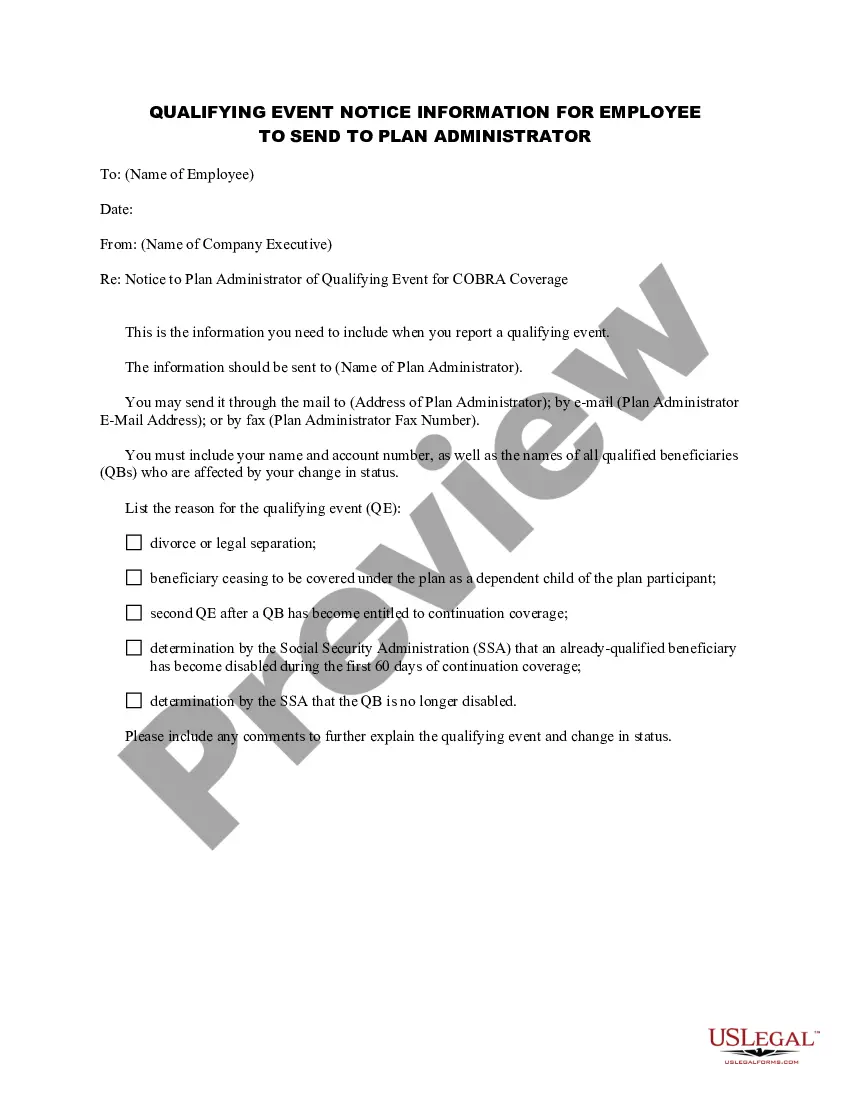
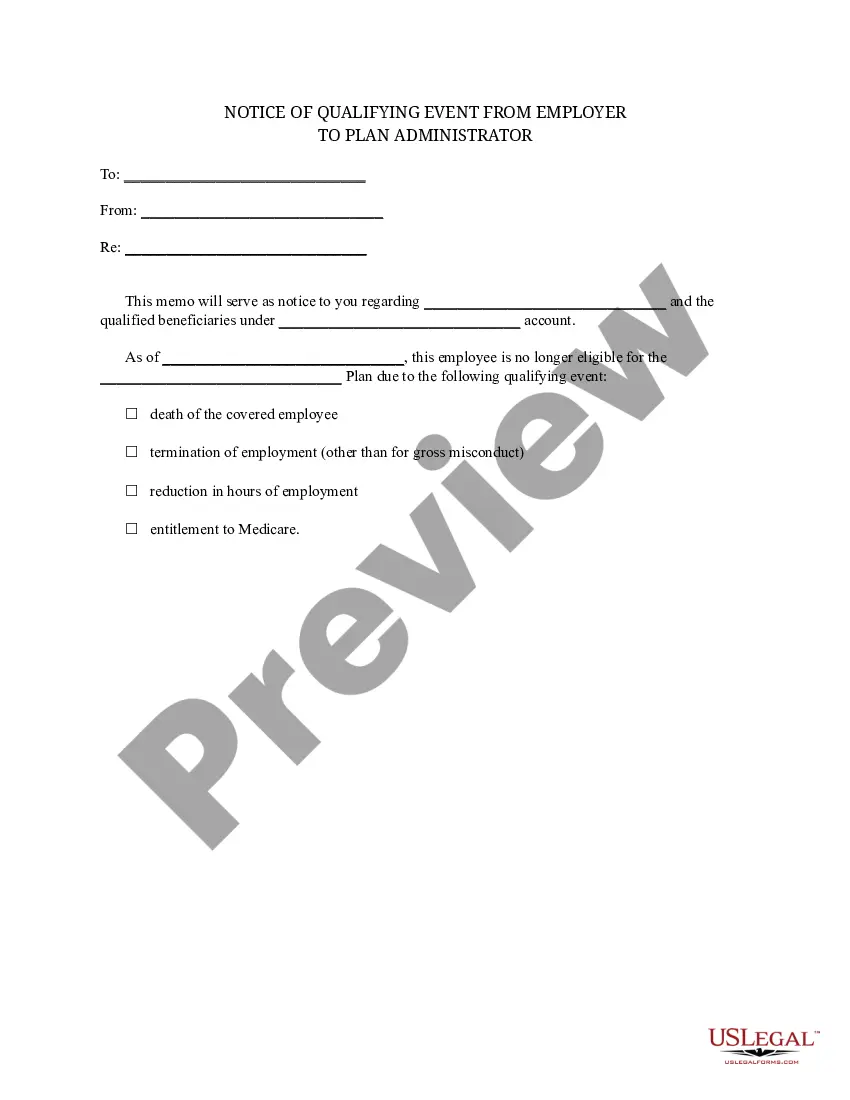
South Dakota Notice of Qualifying Event from Employer to Plan Administrator
Description
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
US Legal Forms - one of the most prominent collections of legal documents in the United States - offers a range of legal template forms that you can download or print.
By using the site, you can access thousands of forms for business and personal purposes, organized by categories, states, or keywords. You can obtain the latest versions of forms such as the South Dakota Notice of Qualifying Event from Employer to Plan Administrator in just minutes.
If you already have a subscription, Log In and download the South Dakota Notice of Qualifying Event from Employer to Plan Administrator from your US Legal Forms library. The Download button will appear on every form you view. You can access all previously saved forms in the My documents tab of your account.
Process the purchase. Use your credit card or PayPal account to complete the transaction.
Choose the format and download the form to your device. Make modifications. Fill out, edit, print, and sign the saved South Dakota Notice of Qualifying Event from Employer to Plan Administrator. Every template you added to your account does not expire and is yours indefinitely. So, if you wish to download or print another copy, simply visit the My documents section and click on the form you need. Gain access to the South Dakota Notice of Qualifying Event from Employer to Plan Administrator with US Legal Forms, the most comprehensive library of legal document templates. Utilize thousands of professional and state-specific templates that meet your business or personal requirements.
- To start using US Legal Forms for the first time, here are simple instructions.
- Ensure you have chosen the correct form for your city/state.
- Click the Review button to check the form's details.
- Read the form description to ensure you have selected the correct form.
- If the form does not meet your requirements, use the Search field at the top of the screen to find one that does.
- If you are satisfied with the form, confirm your choice by clicking the Acquire now button.
- Then, select the pricing plan you prefer and provide your details to register for an account.
Form popularity
FAQ
Codified Laws Sec. 58-18-7). Continuation coverage for 18 months must be provided to employees upon leaving employment or the termination of the coverage by the insurer and their eligible dependents (S.D. Codified Laws Sec.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Qualifying events include the following: Death of the covered employee. Termination or reduction of hours of the covered employee's employment for reasons other than gross misconduct. Divorce or legal separation from a covered employee.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
For covered employees, the only qualifying event is termination of employment (whether the termination is voluntary or involuntary) including by retirement, or reduction of employment hours. In that case, COBRA lasts for eighteen months.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.