Tennessee Cobra Notice
Description
How to fill out Tennessee Cobra Notice?
Preparing legal paperwork can be a real burden unless you have ready-to-use fillable templates. With the US Legal Forms online library of formal documentation, you can be certain in the blanks you obtain, as all of them correspond with federal and state laws and are examined by our experts. So if you need to complete Tennessee Cobra Notice, our service is the perfect place to download it.
Getting your Tennessee Cobra Notice from our service is as simple as ABC. Previously authorized users with a valid subscription need only sign in and click the Download button after they find the correct template. Afterwards, if they need to, users can get the same blank from the My Forms tab of their profile. However, even if you are unfamiliar with our service, registering with a valid subscription will take only a few moments. Here’s a brief guideline for you:
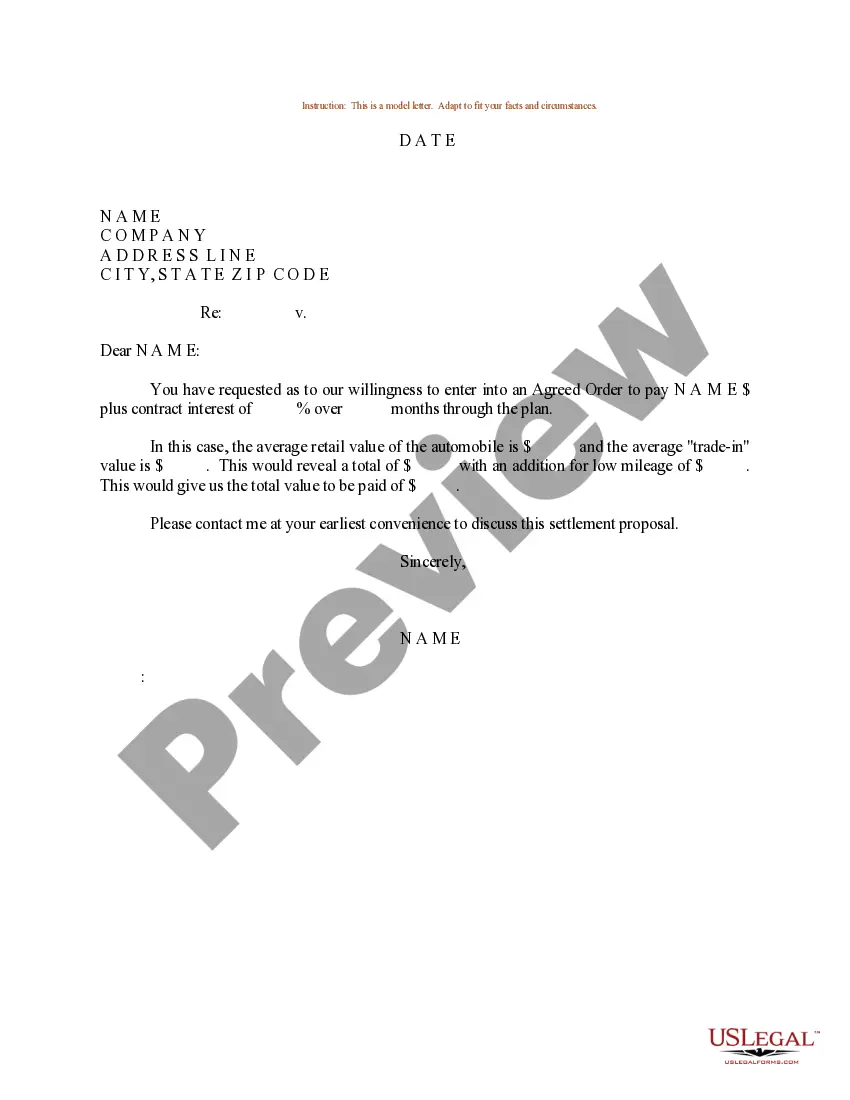
- Document compliance verification. You should carefully examine the content of the form you want and make sure whether it satisfies your needs and fulfills your state law requirements. Previewing your document and looking through its general description will help you do just that.
- Alternative search (optional). If you find any inconsistencies, browse the library through the Search tab on the top of the page until you find an appropriate blank, and click Buy Now once you see the one you need.
- Account creation and form purchase. Register for an account with US Legal Forms. After account verification, log in and select your most suitable subscription plan. Make a payment to continue (PayPal and credit card options are available).
- Template download and further usage. Select the file format for your Tennessee Cobra Notice and click Download to save it on your device. Print it to fill out your papers manually, or use a multi-featured online editor to prepare an electronic copy faster and more effectively.
Haven’t you tried US Legal Forms yet? Subscribe to our service now to get any official document quickly and easily every time you need to, and keep your paperwork in order!
Form popularity
FAQ
How long does it take for COBRA to kick in? With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
COBRA coverage follows a "qualifying event". An example of a qualifying event would be if your hours were reduced or you lost your job (as long as there was no gross misconduct). Your employer must mail you the COBRA information and forms within 14 days after receiving notification of the qualifying event.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, ? Death of the covered employee, ? Covered employee becoming entitled to Medicare, or ? Employer bankruptcy.
Generous Time to Enroll. You have 60 days to enroll in COBRA once your employer-sponsored benefits end. Even if your enrollment is delayed, you will be covered by COBRA starting the day your prior coverage ended. You will receive a notice from your employer with information about deadlines for enrollment.
Through COBRA, individuals pay the entire monthly premium plus a two percent administrative fee, and may be able to remain insured with their health plan for up to 18, 29, or 36 months. All COBRA benefit questions should be directed to Benefits Administration at 615.741. 3590 or 800.253. 9981.
Initial COBRA Notice. Date of Notice: Notice of Rights Under COBRA. The COBRA statute requires that continuation coverage be offered to covered employees and their covered dependents in order to continue their State-sponsored health/dental/vision benefit(s) in the event coverage is lost due to certain qualifying events
You may be able to keep your job-based health plan through COBRA continuation coverage. COBRA coverage lets you pay to stay on your job-based health insurance for a limited time after your job ends (usually 18 months). You usually pay the full premium yourself, plus a small administrative fee.
Through COBRA, individuals pay the entire monthly premium plus a two percent administrative fee, and may be able to remain insured with their health plan for up to 18, 29, or 36 months. All COBRA benefit questions should be directed to Benefits Administration at 615.741. 3590 or 800.253. 9981.