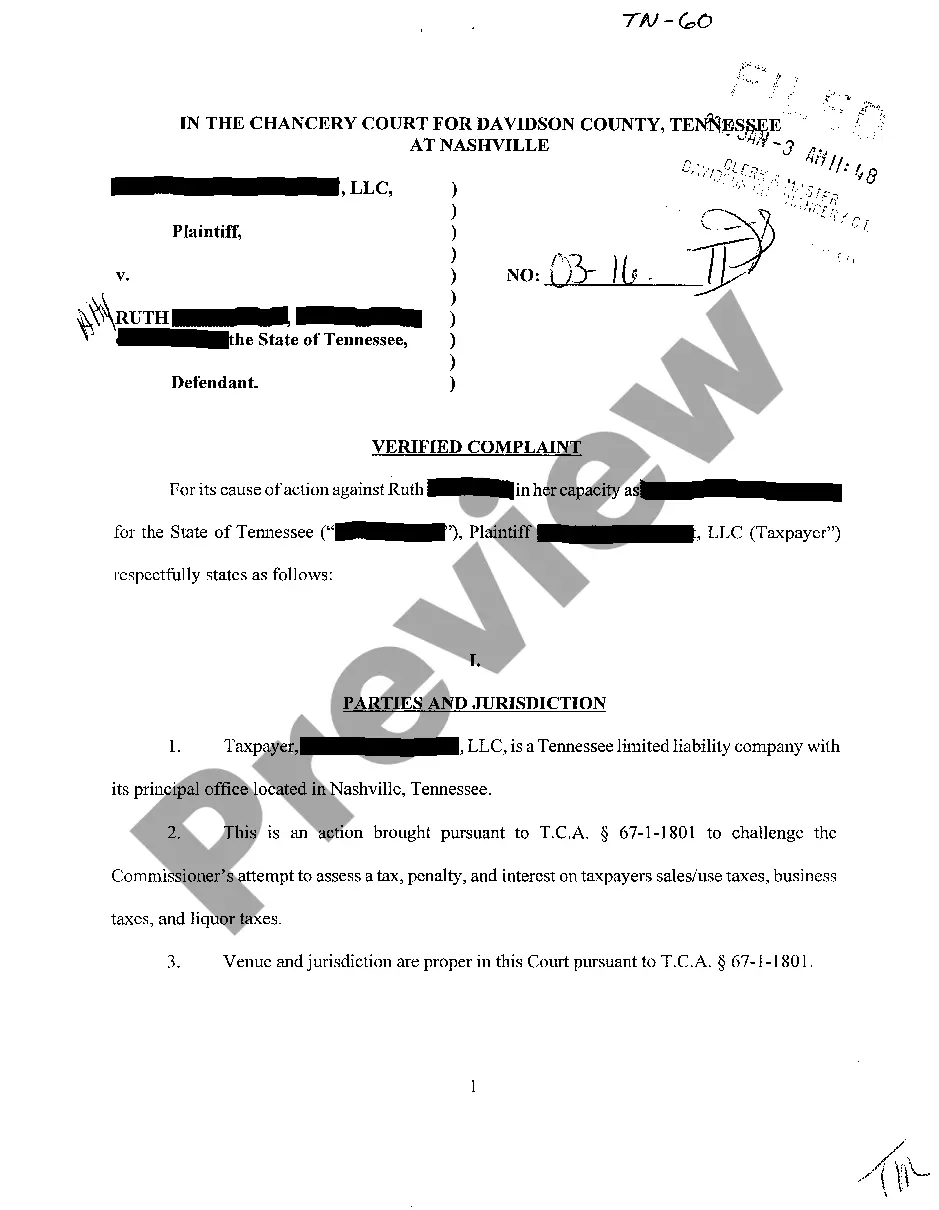
Tennessee Provider Registration for Utilization Review Form
Description
How to fill out Tennessee Provider Registration For Utilization Review Form?
Dealing with legal documentation requires attention, accuracy, and using well-drafted templates. US Legal Forms has been helping people countrywide do just that for 25 years, so when you pick your Tennessee Provider Registration for Utilization Review Form template from our service, you can be sure it meets federal and state laws.
Working with our service is straightforward and fast. To get the necessary document, all you’ll need is an account with a valid subscription. Here’s a quick guideline for you to obtain your Tennessee Provider Registration for Utilization Review Form within minutes:
- Remember to attentively check the form content and its correspondence with general and law requirements by previewing it or reading its description.
- Look for an alternative official blank if the previously opened one doesn’t match your situation or state regulations (the tab for that is on the top page corner).
- Log in to your account and download the Tennessee Provider Registration for Utilization Review Form in the format you need. If it’s your first time with our website, click Buy now to continue.
- Create an account, choose your subscription plan, and pay with your credit card or PayPal account.
- Choose in what format you want to save your form and click Download. Print the blank or upload it to a professional PDF editor to prepare it paper-free.
All documents are created for multi-usage, like the Tennessee Provider Registration for Utilization Review Form you see on this page. If you need them one more time, you can fill them out without re-payment - just open the My Forms tab in your profile and complete your document whenever you need it. Try US Legal Forms and accomplish your business and personal paperwork rapidly and in full legal compliance!
Form popularity
FAQ
Utilization review (UR) is the process of reviewing an episode of care. The review confirms that the insurance company will provide appropriate financial coverage for medical services. The UR process and the UR nurse facilitate minimizing costs.
Utilization review (UR) is the process used by employers or claims administrators to review treatment to determine if it is medically necessary. All employers or their workers' compensation claims administrators are required by law to have a UR program.
Utilization review (UR) is the process used by employers or claims administrators to review treatment to determine if it is medically necessary. All employers or their workers' compensation claims administrators are required by law to have a UR program.
In Tennessee, you need to report your work-related injury to your supervisor within 15 days of the accident (or the date when a doctor first tells you that your injury is work-related) so that the proper forms and paperwork can be completed.
Utilization Review (UR) is the evaluation of medical care services for the treatment provided to an injured worker. This evaluation is done to ensure that the services are necessary, appropriate, and likely to be effective.
Form C-41 Wage Statement. This form enables EMPLOYERS to calculate the correct compensation due to an injured employee. Please complete the form and submit to EMPLOYERS within 5 days after your knowledge of any accident that has caused your employee to be disabled for more than 7 calendar days.
There are three activities within the utilization review process: prospective, concurrent and retrospective.
Other examples of utilization reviews might include determining whether or not a patient should be transferred to a specialty trauma ICU at a regional center or getting insurance approval for an extended hospital stay that goes beyond the typical guidelines.