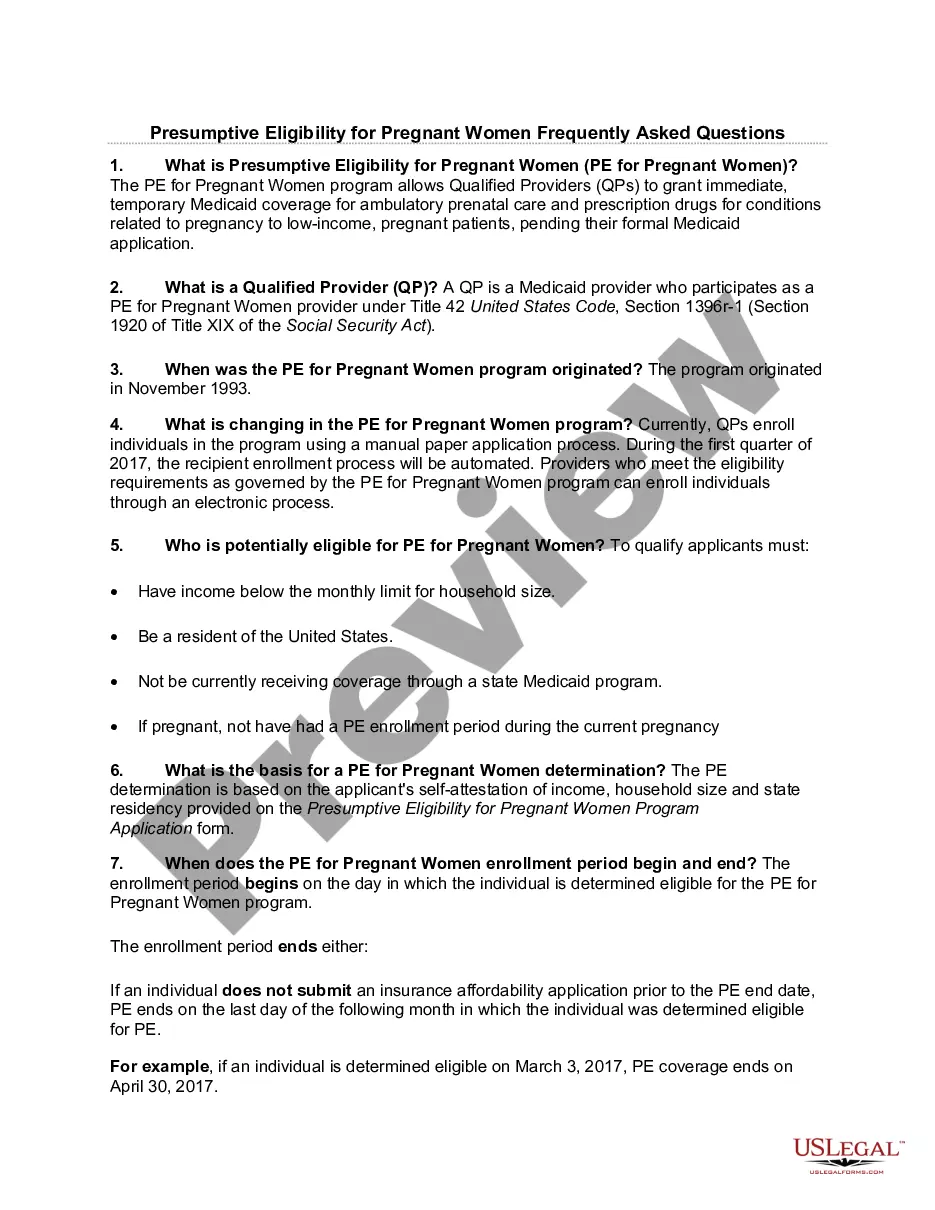
Tennessee Presumptive Eligibility for Pregnant Women FAQ
Description
How to fill out Presumptive Eligibility For Pregnant Women FAQ?
US Legal Forms - one of many biggest libraries of lawful types in the United States - provides a variety of lawful file layouts you may acquire or printing. While using internet site, you can find a large number of types for organization and personal functions, categorized by types, says, or key phrases.You can find the most up-to-date variations of types much like the Tennessee Presumptive Eligibility for Pregnant Women FAQ in seconds.
If you have a subscription, log in and acquire Tennessee Presumptive Eligibility for Pregnant Women FAQ in the US Legal Forms library. The Acquire option will show up on every single develop you look at. You have accessibility to all formerly acquired types in the My Forms tab of your respective accounts.
In order to use US Legal Forms the very first time, here are simple guidelines to help you get started off:
- Make sure you have chosen the correct develop for your personal town/area. Go through the Review option to review the form`s content. See the develop description to actually have selected the right develop.
- In case the develop does not suit your requirements, utilize the Search discipline at the top of the screen to get the the one that does.
- When you are satisfied with the shape, verify your choice by visiting the Buy now option. Then, opt for the prices program you like and give your references to sign up to have an accounts.
- Method the transaction. Utilize your bank card or PayPal accounts to accomplish the transaction.
- Pick the formatting and acquire the shape in your gadget.
- Make alterations. Load, revise and printing and indication the acquired Tennessee Presumptive Eligibility for Pregnant Women FAQ.
Each and every web template you put into your account lacks an expiry date and is also the one you have forever. So, if you would like acquire or printing an additional version, just proceed to the My Forms section and click in the develop you want.
Get access to the Tennessee Presumptive Eligibility for Pregnant Women FAQ with US Legal Forms, one of the most considerable library of lawful file layouts. Use a large number of skilled and express-distinct layouts that meet up with your small business or personal demands and requirements.
Form popularity
FAQ
To apply for Medicaid in Tennessee, applicants must submit various documentation, including proof of income, identification, and residency. Additional documents may be needed based on individual circumstances, such as pregnancy. Ensuring you have the right paperwork can expedite the application process. For more information on the documentation you need, refer to the Tennessee Presumptive Eligibility for Pregnant Women FAQ for detailed guidance.
The Tennessee eligibility determination system assesses applicants for Medicaid and TennCare based on various factors, including income and household size. This system helps streamline the application process and ensures that eligible individuals receive timely care. Users can access useful tools and resources through uslegalforms to better understand their eligibility. It’s key to stay informed, especially when exploring information on the Tennessee Presumptive Eligibility for Pregnant Women FAQ.
If you don't have health insurance, you may be able to get low-cost or free prenatal care from Planned Parenthood, community health centers, or other family planning clinics. You might also qualify for health insurance through your state if you're pregnant.
The TennCare Presumptive Medicaid Program provides TennCare Medicaid enrollment coverage for pregnant women to encourage early entry into prenatal care and for women diagnosed with breast or cervical cancer for access to early medical services for treatment.
Medicaid can also deny pregnant women because their household size is too small relative to the total income. Therefore, you do not want to omit a dependent unknowingly or include an extra wage earner and hurt your eligibility.
All Health Insurance Marketplace® and Medicaid plans cover pregnancy and childbirth. This is true even if your pregnancy begins before your coverage starts. Maternity care and newborn care services provided before and after your child is born are essential health benefits.
How long does it take? You will find out whether or not you are eligible for Medicaid within 45-60 days after you apply. Any Special Circumstances? If you are pregnant and eligible, you can get a Medicaid certification form on the same day that you apply.
Texas Health and Human Services (HHS) staff have 15 business days to process the application from the day they received it. Once eligibility is determined, the pregnant woman enrolls in a CHIP perinatal health plan on behalf of her unborn child.
If you're pregnant when you apply, an insurance plan can't reject you or charge you more because of your pregnancy. Once you're enrolled, your pregnancy and childbirth are covered from the day your plan starts.
Under the ACA, all Marketplace plans must cover pre-existing conditions you had before coverage started. According to Healthcare.gov, pregnancy is not considered a pre-existing condition. So if you were pregnant at the time that you applied for new health coverage: You can't be denied coverage due to your pregnancy.